4.7 Antidepressants, BDNF levels and neurogenesis in the hippocampus
If stress leads to a decline in neurogenesis, antidepressants seem to have exactly the opposite effect. There is now good evidence, from experimental work on rats, that ADMs such as Prozac®, an SSRI which increases levels of serotonin in the brain, stimulate the production of new neurons in the hippocampus (Malberg et al., 2000).
Importantly, Malberg et al. (2000) found that ADMs such as SSRIs only stimulate neurogenesis in the hippocampus if given every day for several weeks.
Why is this an important finding?
Because it fits well with, and has the potential to explain, the observation above that ADMs such as SSRIs show clinical efficacy only after several weeks of being given daily.
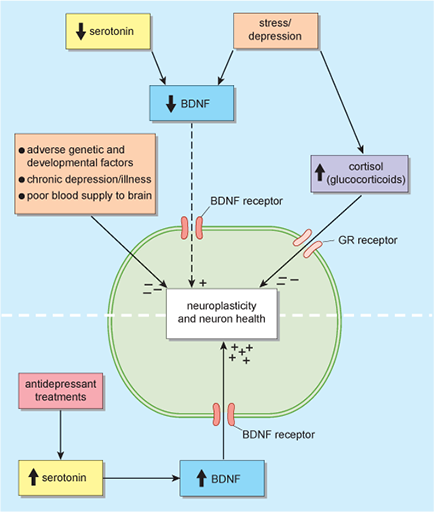
How does serotonin, levels of which are increased by SSRIs, have an effect on neurogenesis? It appears that serotonin stimulates the production of BDNF.
Why are BDNF levels low in the first place? Experimental evidence suggests that stress (which, as you saw, releases powerful hormones such as glucocorticoids into the blood), reduces the levels of BDNF produced in the hippocampus, by damaging neurons in the hippocampus. This reduction in BDNF levels appears to be prevented or reversed by ADM treatment (Warner-Schmidt and Duman, 2006).
Indeed current evidence suggests that many antidepressant treatments, including SSRIs, electroconvulsive therapy (ECT), and exercise exert their effects by stimulating the production of BDNF in brain areas such as the hippocampus.
Clearly, the neurotrophic hypothesis offers a much more complex and integrated view of the possible causes of depression, as shown in Figure 11. (The schema shown in Figure 11 also allows for the possibility that unknown genetic vulnerabilities could affect neurons and their capacity to produce BDNF.)
To recap, the implication is that neurogenesis, promoted by ADMs via the release of BDNF, underlies the efficacy of ADMs. Thus a final question is whether there is any evidence for this. That is, are changes in behaviour consequent on taking ADMs linked to hippocampal neurogenesis? So far, this issue has been addressed in a study using animals, but it appears that there is indeed a link. Santarelli et al. (2003) found that if neurogenesis in the hippocampus was suppressed, ADMs failed to affect behaviour. The results do not prove that a lack of neurogenesis causes depression, or that increased neurogenesis cures it, but it does suggest that neurogenesis is an important factor.
