1.1 Evolution of antibiotic resistance in microbes
Infections caused by bacteria but not treatable by common antibiotics, are one of the greatest healthcare concerns today. One of the most problematic microbes, alongside C. difficile, is the so-called hospital ‘superbug’ MRSA.
What do the initials MRSA stand for?
MRSA stands for methicillin-resistant Staphylococcus aureus.
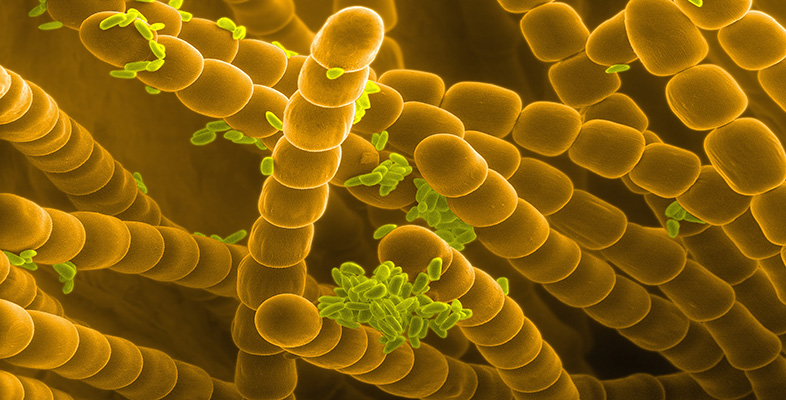
Methicillin is a type of antibiotic that was previously used to kill this bacterium, though it has now been superseded by more stable antibiotics such as flucloxacillin. In fact, the initials can equally well mean ‘multiple-resistant Staphylococcus aureus’, a reference to the bacterium’s resistance to a range of antibiotics. There are well over 30 different Staphylococcus species that grow in characteristic clumps, like tiny bunches of grapes (Figure 1). About 10 of these species are natural human commensals but can, under some conditions, develop into serious pathogens.
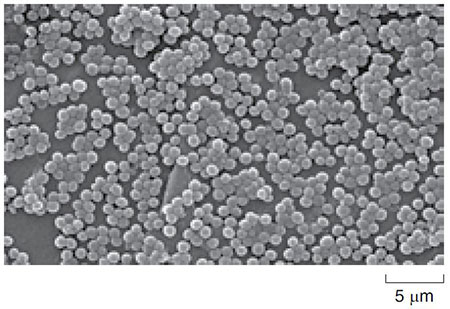
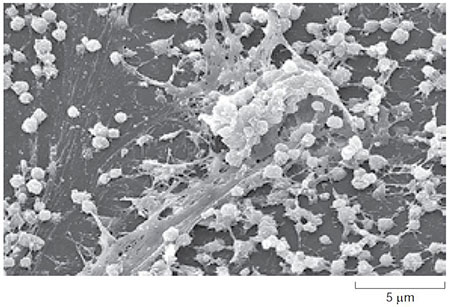
Staph. aureus is of particular concern because it can cause a wide range of disease conditions from toxic shock syndrome (TSS) to skin infections, particularly infecting people with weakened immune systems or with wounds, making it a problem in hospitals. Although the bacterium can grow without oxygen, it grows and reproduces more quickly if oxygen is present. Such bacteria are called facultative anaerobes. In healthy people Staph. aureus naturally lives in the armpits and in the nose, but once it is inside the body it forms biofilms which protect it against the immune system and allow it to proliferate. Biofilms can form anywhere bacteria can find a surface to attach to, even including an apparently smooth surface such as plastic (Figure 2).
Understanding how microbes develop resistance against antibiotics is one of the most important challenges in modern microbiology. It appears that antibiotic resistance genes arose by the process of mutation.
What is meant by the term mutation?
Mutations are random changes which occur in the DNA of living organisms, due to the DNA replication process not being perfectly efficient every time.
Although mutations occur naturally, they can also be induced by radiation and certain drugs. Most mutations are harmful to the organism possessing them, and so that individual dies. However, occasionally, by chance, a mutation can occur that is beneficial to the organism. In the case of microbes, this could be a mutation in a gene which allows the microbe to survive in the presence of antibiotics, i.e. to be resistant to antibiotics. Because microbes divide by binary fission, the mutant gene can spread very rapidly, as every offspring of the resistant microbe has an exact copy of the DNA and so will also carry the mutant gene. So, if one in 10 000 bacteria in a colony within a wound being treated with an antibiotic such as flucloxacillin, developed a mutation which made it resistant to the antibiotic, the other 9999 bacteria would die, but that one would survive and divide and within a few days, there could be a new colony of 10 000 resistant bacteria in the wound.
The antibiotic resistance genes may function in several ways. For example, they can cause the microbes to produce substances that change the structure of the cell wall to prevent the antibiotic entering or that break down the antibiotic before it can do any harm. Or they may change biochemical pathways (sets of reactions which produce important substances in the microbe), to by-pass the parts of the pathway which are normally sensitive to the antibiotic. The antibiotic resistance genes seem to be amongst those genes that are carried on plasmids.
What are plasmids and how do they relate to chromosomal DNA?
Plasmids are small circular pieces of DNA found in bacteria. They are from 10 to 1000 times smaller than the main circular DNA loop (bacterial chromosome) which forms the genomic DNA.
Crucially, for the progress of antibiotic resistance, plasmids can be transferred from one microbe to another by a process called conjugation.
In one sentence, describe what happens to the chromosomal DNA of a microbe when it undergoes binary fission.
The DNA of the microbe is copied and one copy is put into each of the two new microbial cells produced in the binary fission process.
You will not be surprised to know that these small circles of DNA are also replicated and transferred into both of the new cells when one cell divides. There can be from one to more than a thousand copies of the same plasmid in any one microbe. In the process of conjugation, illustrated in Figure 3, one microbe can pass a plasmid to another of the same species. Two microbes come together and one of them extends an appendage called a pilus.
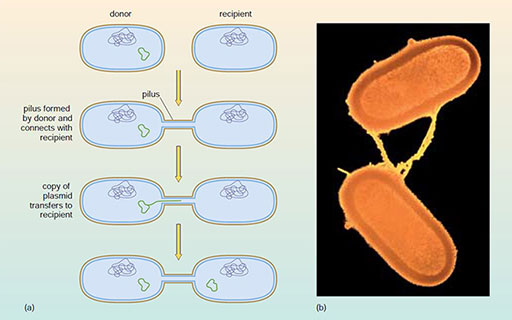
In conjugation the pilus is a hollow fibre a few micrometres long, that can connect the two microbes. One of the plasmids in one of the microbes opens up, is copied and is transferred along the length of the pilus into the attached microbe. Since the antibiotic-resistance genes are on the plasmids, this can result in the transfer of such resistance from one microbe to another. When that microbe divides (by binary fission) the resistance will be passed on to all of its offspring. This appears to be one of the reasons for the rapid spread of resistant microbes in hospitals. Conjugation does, of course, occur between microbes in other environments too and is a way in which genes that enable microbes to survive particular environmental stresses can be passed from one to another.
Question 2
It has been suggested that conjugation in microbes is a form of sexual reproduction. Identify one similarity and one difference between the two processes.
Answer
Both processes involve DNA from two individuals. In conjugation, two cells come together and one extends a pilus. In sexual reproduction, two individuals come together and mate. However, in conjugation, the main part of the DNA (the genomic DNA) is not usually involved; a subsidiary piece, called a plasmid, is usually transferred. In sexual reproduction, half of the DNA of one individual is combined with half from the other, so that the offspring has characteristics of both parents.
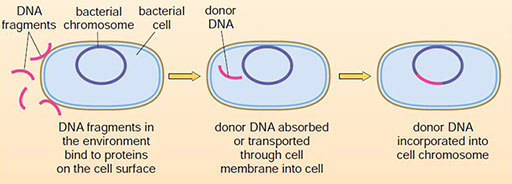
Yet another reason for the rapid spread of resistance genes and the adaptation to new antibiotics is the remarkable ability that microbes have to take up DNA, across the wall of their cells, from their environment without receiving it from another microbe. This process is known as transformation and is illustrated in Figure 4.
How could ‘naked’ DNA (that is, DNA not inside cells) be present in the environment?
The DNA must have been produced by living cells, probably other microbes, originally. After their death, the walls of the cells would break down and the DNA would be released into the environment, to be taken up in the transformation process.
Question 3
Give two differences between conjugation and transformation in bacteria.
Answer
These are the two obvious differences.
- Conjugation requires the presence of another microbe, whereas transformation does not need any other living cells to be present, just the DNA.
- Conjugation generally transfers plasmid DNA only. In transformation, the foreign DNA could be derived from many different sources and is taken up as naked DNA from the environment.
Additionally, in conjugation, the DNA transfer is usually successful. The transformation process may not be successful as the DNA fragment taken up may be destroyed in the cell.
Transformation allows genes which are completely new to that species to be taken up and incorporated into its DNA, where they may function correctly. Thus a microbe in which resistance to a particular antibiotic had never previously been seen, could take up a fragment of DNA which had been released into the environment on the death of another entirely different microbe. This fragment of DNA could contain a gene which confers resistance to that antibiotic if successfully integrated and, after several cycles of binary fission, a new resistant population could appear.
The spread of resistance to antibiotics can be surprisingly rapid. After the antibiotic penicillin was introduced for general use in 1947, Staphylococcus aureus became resistant to it in four years. In 1959, a new antibiotic, methicillin, was used to treat these resistant strains but the first methicillin-resistant strains (MRSA) were detected only two years later in 1961. These strains have recently spread to hospitals throughout the world. More recently, new strains are emerging that are resistant to the more modern antibiotic, vancomycin. VRSA (Vancomycin-resistant Staphylococcus aureus) appeared in 2002. The introduction of a new synthetic antibiotic linezolid in 2000, resulted in resistant strains appearing in 2003.
Linezolid is a synthetic antibiotic, that is, it is produced by chemical synthesis initially in a laboratory, then on a commercial scale. How are antibiotics like penicillin produced?
Antibiotics like penicillin are all produced by microbes such as the Actinobacteria. Penicillin itself is extracted from the fungus Penicillium.
Antibiotic resistance can be thought of as an arms race between microbes and humans. Each time a new antimicrobial agent is developed, a microbe eventually undergoes a genetic alteration that allows it to acquire resistance which may spread through the microbial population. A major activity in microbiology is to find new antimicrobial agents to keep up with the ever-changing resistance of microbes. The spread of resistance has been made easier by two particular aspects of medical practice. The widespread use of antibiotics for minor infections increases the chance that a resistant strain of microbe might arise because more species of microbes come into contact with antibiotics. Resistance to antibiotics is also caused by patients taking incomplete antibiotic courses. This exposes microbes to concentrations of antibiotics which are not lethal, but are at sufficient concentrations preferentially to give an advantage to bacteria in the population that do have resistance. There is the risk that microbes with partial resistance may be more likely to survive and more quickly develop complete resistance. These resistant bacteria then multiply and dominate the population. By finishing a course of antibiotics one is more likely to kill the target microbes and so prevent them from developing resistance.