Microbes – friend or foe?
Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Saturday, 27 April 2024, 12:17 AM
Microbes – friend or foe?
Introduction
This course looks at two aspects of microbes. The first section covers the way that bacteria cause disease and how they can become resistant to the antibiotics used to treat them. The second covers the important role that microbes play in treating sewage to purify the water so that it can be returned to rivers or to the sea.
This OpenLearn course is an adapted extract from the Open University course SG071 Learn about microbes.
Learning outcomes
After studying this course, you should be able to:
demonstrate general knowledge and understanding of some of the basic facts, language, concepts and principles relating to microbiology and its importance and applications in biological and health sciences and environmental sciences
understand the contribution that microbiology can make to informed debate on medical and environmental issues
make sense of information presented in different ways, including textual, numerical and graphical material.
1 Disease-causing bacteria
Surprisingly, many bacteria that cause disease are ones that are naturally present in or on our bodies. Bacteria that co-exist with the human body are known as commensal bacteria. It is a change in the normal situation, caused for example by a wound, which gives them a chance to grow and become a menace rather than remain a harmless natural inhabitant. Commensals also maintain a natural microbial balance in the body and help prevent pathogens from becoming abundant.
One of the most important groups of commensal bacteria is the genus Streptococcus, which can cause numerous infections including pneumonia. Streptococcus pyogenes is perhaps the most infamous and is sometimes known as the ‘flesh-eating’ bacterium. In fact, the condition known as necrotising fasciitis, an infection of the deeper layers of the skin, causing large-scale deterioration of flesh, is very rare. More commonly Streptococcus pyogenes strains are involved in causing skin infections, meningitis and pharyngitis (‘strep throat’); each one of these may be caused by different strains. About one-tenth of the population carry the Strep. pyogenes bacterium around in their throats and noses and usually it does no harm at all. (Note that because the genera Streptococcus and Staphylococcus can be easily confused if referred to in their abbreviated form, simply by the first letter of their genus, their names are instead often shortened to Strep. and Staph.) Strep. pyogenes is not destroyed by the immune system because it carries proteins on its cell surface that resemble human proteins, thus fooling the system into thinking it is part of the human body and preventing it being destroyed. About one-fifth of the population have Strep. pneumoniae in their body and it too can produce a surface layer that allows it to evade the immune system. A commensal species can cause an infection if its growth becomes out of balance with the rest of the natural microbial population in the human body. The population size and activity of each commensal species are normally kept in check by competition from other commensals, but if the balance is disrupted then some commensals or even foreign microbes may get a chance to multiply and become more active.
Many of the anaerobic bacteria naturally found in our gut may also become the cause of disease. The most common culprits are those in the phylum Bacteroides, which most of the time are beneficial. They exclude more dangerous pathogens from the gut, essentially by out-competing them for space and food. However, outside the gut and out of control in other areas of the body, these organisms can become a serious problem, causing abscesses, blood infection, infections under the skin and infections of the abdominal cavity.
Bacteria of the genus Clostridium are common in soil and can be responsible for a range of diseases in people. Often they are picked up from soil or from poorly cleaned food.
Which species of Clostridium causes tetanus?
Tetanus is caused by C. tetani.
The clostridia produce toxins, which affect the nervous system. So, if C. tetani gets into a wound and multiplies, the toxins are released, enter the bloodstream and from there travel to the nerves and result in the excessive contraction of some of the muscles in the face, causing lockjaw (the common name for tetanus). Of all the clostridia species in the wild, C. botulinum produces the most powerful toxin and it is responsible for botulism, a type of food poisoning that is potentially fatal. The best known of the clostridia is C. difficile, one of the few clostridia naturally present in the human population. About 3% of adults are thought to carry it in their gut. It rarely causes disease unless the natural population of microbes in the gut has been disturbed, such as during the administering of antibiotics, which kill off many of the natural gut microbes. In this case, C. difficile can multiply uncontrollably and release its toxins causing toxic shock syndrome (TSS), with a range of symptoms including a rash, high fever, low blood pressure, confusion and ultimately coma and multiple organ failure, resulting in death.
Not all bacteria produce spores, but C. difficile does. Why might this be a problem in treating it?
The spores produced by the bacterium allow it to be spread around easily in the environment, including amongst staff and patients in hospitals. The spores also give C. difficile resistance to many extreme environmental conditions, which allows it to survive for long periods of time in the natural environment outside human bodies and makes it difficult to kill on surfaces and in the air.
Question 1
Using the data in the current section, of a group of 100 people how many would, on average, be found to carry one of Streptococcus pyogenes, Streptococcus pneumoniae or Clostridium difficile? Why are individuals carrying these microbes generally not ill?
Answer
Streptococcus pyogenes is found in one-tenth of the population, so that means that 10 people in every hundred would carry it. Streptococcus pneumoniae occurs in one-fifth of the population, which is 20 in every hundred individuals and Clostridium difficile is found in 3% of the population, 3 in every hundred people. So if each person only carried one species, then 33 people in every hundred (33%) of the population would be infected with one of the three species. In fact, probably some people will carry two, and a few might be harbouring all three, so the number of infected people is likely to be less than 33 in every hundred. As long as the people carrying these microbes have immune systems which are functioning efficiently, they are not taking antibiotics and they do not have any wounds or similar injuries, the microbes are kept under control and do not multiply and cause disease. However, when patients are admitted to hospital they are increasingly screened (tested) for these microbes so that precautions can be taken to prevent the spread of infection.
Equally infamous is Escherichia coli, a Gram-negative bacterium found naturally living in the gut. E. coli normally colonises the gut within the first two days after birth. Like so many bacteria, usually it is a harmless commensal, but there are some strains of the bacterium that are harmful. One of the most well known is E. coli strain O157, which can cause serious food poisoning by producing toxins. In young children and the elderly or in people whose immune system is not functioning properly, it can be fatal.
1.1 Evolution of antibiotic resistance in microbes
Infections caused by bacteria but not treatable by common antibiotics, are one of the greatest healthcare concerns today. One of the most problematic microbes, alongside C. difficile, is the so-called hospital ‘superbug’ MRSA.
What do the initials MRSA stand for?
MRSA stands for methicillin-resistant Staphylococcus aureus.
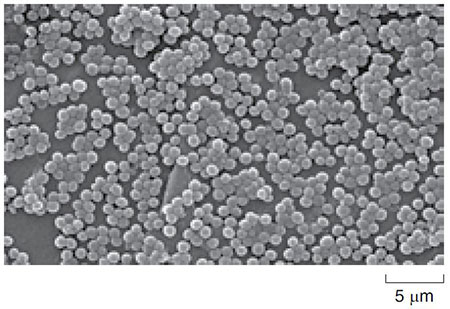
Methicillin is a type of antibiotic that was previously used to kill this bacterium, though it has now been superseded by more stable antibiotics such as flucloxacillin. In fact, the initials can equally well mean ‘multiple-resistant Staphylococcus aureus’, a reference to the bacterium’s resistance to a range of antibiotics. There are well over 30 different Staphylococcus species that grow in characteristic clumps, like tiny bunches of grapes (Figure 1). About 10 of these species are natural human commensals but can, under some conditions, develop into serious pathogens.
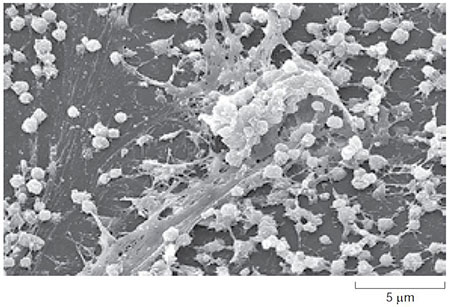
Staph. aureus is of particular concern because it can cause a wide range of disease conditions from toxic shock syndrome (TSS) to skin infections, particularly infecting people with weakened immune systems or with wounds, making it a problem in hospitals. Although the bacterium can grow without oxygen, it grows and reproduces more quickly if oxygen is present. Such bacteria are called facultative anaerobes. In healthy people Staph. aureus naturally lives in the armpits and in the nose, but once it is inside the body it forms biofilms which protect it against the immune system and allow it to proliferate. Biofilms can form anywhere bacteria can find a surface to attach to, even including an apparently smooth surface such as plastic (Figure 2).
Understanding how microbes develop resistance against antibiotics is one of the most important challenges in modern microbiology. It appears that antibiotic resistance genes arose by the process of mutation.
What is meant by the term mutation?
Mutations are random changes which occur in the DNA of living organisms, due to the DNA replication process not being perfectly efficient every time.
Although mutations occur naturally, they can also be induced by radiation and certain drugs. Most mutations are harmful to the organism possessing them, and so that individual dies. However, occasionally, by chance, a mutation can occur that is beneficial to the organism. In the case of microbes, this could be a mutation in a gene which allows the microbe to survive in the presence of antibiotics, i.e. to be resistant to antibiotics. Because microbes divide by binary fission, the mutant gene can spread very rapidly, as every offspring of the resistant microbe has an exact copy of the DNA and so will also carry the mutant gene. So, if one in 10 000 bacteria in a colony within a wound being treated with an antibiotic such as flucloxacillin, developed a mutation which made it resistant to the antibiotic, the other 9999 bacteria would die, but that one would survive and divide and within a few days, there could be a new colony of 10 000 resistant bacteria in the wound.
The antibiotic resistance genes may function in several ways. For example, they can cause the microbes to produce substances that change the structure of the cell wall to prevent the antibiotic entering or that break down the antibiotic before it can do any harm. Or they may change biochemical pathways (sets of reactions which produce important substances in the microbe), to by-pass the parts of the pathway which are normally sensitive to the antibiotic. The antibiotic resistance genes seem to be amongst those genes that are carried on plasmids.
What are plasmids and how do they relate to chromosomal DNA?
Plasmids are small circular pieces of DNA found in bacteria. They are from 10 to 1000 times smaller than the main circular DNA loop (bacterial chromosome) which forms the genomic DNA.
Crucially, for the progress of antibiotic resistance, plasmids can be transferred from one microbe to another by a process called conjugation.
In one sentence, describe what happens to the chromosomal DNA of a microbe when it undergoes binary fission.
The DNA of the microbe is copied and one copy is put into each of the two new microbial cells produced in the binary fission process.
You will not be surprised to know that these small circles of DNA are also replicated and transferred into both of the new cells when one cell divides. There can be from one to more than a thousand copies of the same plasmid in any one microbe. In the process of conjugation, illustrated in Figure 3, one microbe can pass a plasmid to another of the same species. Two microbes come together and one of them extends an appendage called a pilus.
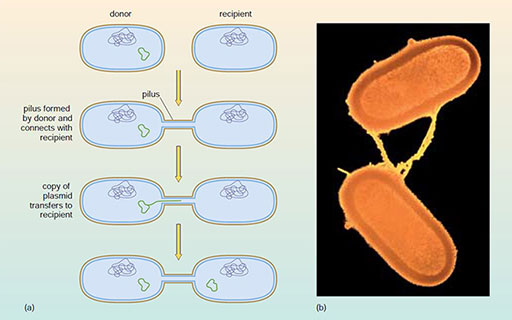
In conjugation the pilus is a hollow fibre a few micrometres long, that can connect the two microbes. One of the plasmids in one of the microbes opens up, is copied and is transferred along the length of the pilus into the attached microbe. Since the antibiotic-resistance genes are on the plasmids, this can result in the transfer of such resistance from one microbe to another. When that microbe divides (by binary fission) the resistance will be passed on to all of its offspring. This appears to be one of the reasons for the rapid spread of resistant microbes in hospitals. Conjugation does, of course, occur between microbes in other environments too and is a way in which genes that enable microbes to survive particular environmental stresses can be passed from one to another.
Question 2
It has been suggested that conjugation in microbes is a form of sexual reproduction. Identify one similarity and one difference between the two processes.
Answer
Both processes involve DNA from two individuals. In conjugation, two cells come together and one extends a pilus. In sexual reproduction, two individuals come together and mate. However, in conjugation, the main part of the DNA (the genomic DNA) is not usually involved; a subsidiary piece, called a plasmid, is usually transferred. In sexual reproduction, half of the DNA of one individual is combined with half from the other, so that the offspring has characteristics of both parents.
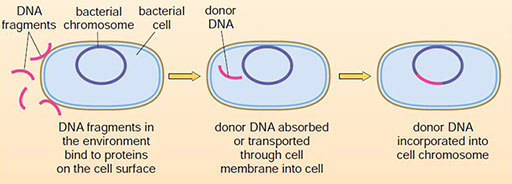
Yet another reason for the rapid spread of resistance genes and the adaptation to new antibiotics is the remarkable ability that microbes have to take up DNA, across the wall of their cells, from their environment without receiving it from another microbe. This process is known as transformation and is illustrated in Figure 4.
How could ‘naked’ DNA (that is, DNA not inside cells) be present in the environment?
The DNA must have been produced by living cells, probably other microbes, originally. After their death, the walls of the cells would break down and the DNA would be released into the environment, to be taken up in the transformation process.
Question 3
Give two differences between conjugation and transformation in bacteria.
Answer
These are the two obvious differences.
- Conjugation requires the presence of another microbe, whereas transformation does not need any other living cells to be present, just the DNA.
- Conjugation generally transfers plasmid DNA only. In transformation, the foreign DNA could be derived from many different sources and is taken up as naked DNA from the environment.
Additionally, in conjugation, the DNA transfer is usually successful. The transformation process may not be successful as the DNA fragment taken up may be destroyed in the cell.
Transformation allows genes which are completely new to that species to be taken up and incorporated into its DNA, where they may function correctly. Thus a microbe in which resistance to a particular antibiotic had never previously been seen, could take up a fragment of DNA which had been released into the environment on the death of another entirely different microbe. This fragment of DNA could contain a gene which confers resistance to that antibiotic if successfully integrated and, after several cycles of binary fission, a new resistant population could appear.
The spread of resistance to antibiotics can be surprisingly rapid. After the antibiotic penicillin was introduced for general use in 1947, Staphylococcus aureus became resistant to it in four years. In 1959, a new antibiotic, methicillin, was used to treat these resistant strains but the first methicillin-resistant strains (MRSA) were detected only two years later in 1961. These strains have recently spread to hospitals throughout the world. More recently, new strains are emerging that are resistant to the more modern antibiotic, vancomycin. VRSA (Vancomycin-resistant Staphylococcus aureus) appeared in 2002. The introduction of a new synthetic antibiotic linezolid in 2000, resulted in resistant strains appearing in 2003.
Linezolid is a synthetic antibiotic, that is, it is produced by chemical synthesis initially in a laboratory, then on a commercial scale. How are antibiotics like penicillin produced?
Antibiotics like penicillin are all produced by microbes such as the Actinobacteria. Penicillin itself is extracted from the fungus Penicillium.
Antibiotic resistance can be thought of as an arms race between microbes and humans. Each time a new antimicrobial agent is developed, a microbe eventually undergoes a genetic alteration that allows it to acquire resistance which may spread through the microbial population. A major activity in microbiology is to find new antimicrobial agents to keep up with the ever-changing resistance of microbes. The spread of resistance has been made easier by two particular aspects of medical practice. The widespread use of antibiotics for minor infections increases the chance that a resistant strain of microbe might arise because more species of microbes come into contact with antibiotics. Resistance to antibiotics is also caused by patients taking incomplete antibiotic courses. This exposes microbes to concentrations of antibiotics which are not lethal, but are at sufficient concentrations preferentially to give an advantage to bacteria in the population that do have resistance. There is the risk that microbes with partial resistance may be more likely to survive and more quickly develop complete resistance. These resistant bacteria then multiply and dominate the population. By finishing a course of antibiotics one is more likely to kill the target microbes and so prevent them from developing resistance.
2 Microbes in sewage treatment
All living things, including ourselves and microbes, need food to grow, maintain and repair their cells, and to provide a source of energy for life. However, we cannot digest all of the food we eat and what remains undigested, ends up in the sewage system. About 10 billion litres of sewage are produced every day in England and Wales and this has to be treated to remove harmful substances and pathogenic microbes before the waste can be safely released into the environment. The main component of sewage is organic matter (undigested food) but there are other substances such as oil, heavy metals, nitrogen and phosphorous compounds (from artificial fertilisers and detergents) which also have to be removed. Here you will consider the important role of microbes in the sewage treatment process.
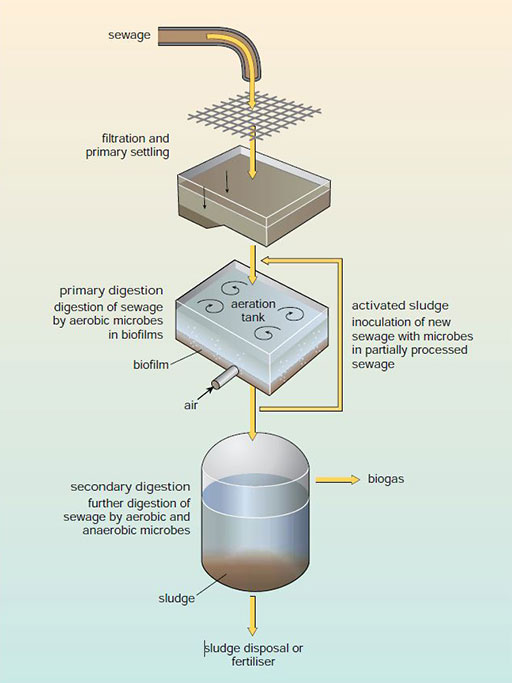
Sewage is actually a mixture of all types of waste water, including rain water and domestic water from toilets, baths and sinks. When sewage arrives at a treatment works (shown schematically in Figure 5), it is first filtered to remove large objects (e.g. condoms, tampons and cigarette ends) which have got into the system. These usually go to a landfill site or incinerator. The remaining material is then allowed to ‘settle’so that much of the solid material drops to the bottom of a tank. This solid material is then removed and usually buried in landfill, burnt or, after further treatment, used as fertiliser on agricultural land.
What then remains is the liquid portion, or effluent, which is rich in suspended organic matter and some pathogenic microbes. This liquid portion will ultimately be released into rivers or the sea but it is vital to first reduce the organic matter content and eliminate harmful microbes. To do this the liquid is fed into an aeration tank containing a complex community of microbes. The contents of the tank are mixed mechanically with air or air is bubbled through the tank. The microbes then use the organic material in the sewage as their source of carbohydrate for respiration.
The oxygen in the air allows the microbes to respire aerobically.What are the products of the aerobic respiration of carbohydrates like glucose?
Aerobic respiration can break down carbohydrates completely, producing just carbon dioxide and water (together with energy needed for the microbes to stay alive).
Aerobic respiration is the most efficient way of breaking down organic matter although some compounds in the effluent are not broken down completely. The tanks often contain porous solid materials, on which biofilms can develop, increasing the numbers of microbes and so the efficiency of the breakdown process. During this process, a fairly solid material known as activated sludge is formed. This contains a mix of microbes and undigested material. Since it contains all of the essential microbes to break down incoming waste, some of it is added to batches of new sewage (Figure 5). After this aerobic digestion, and a variety of other purification procedures, the liquid portion of the sewage is usually safe to discharge into rivers or the sea. The remaining activated sludge material is subjected to various other types of biological processes to reduce further the amount of organic matter it contains. Anaerobic bacteria are often used in this subsequent stage, since, although they grow more slowly, they can break down more complex materials that are difficult to degrade using microbes that respire aerobically. The gases produced in this anaerobic process are carbon dioxide and methane, a mixture called biogas, which can be collected and subsequently burned for energy production.
Sewage processing reduces the concentration of potentially harmful bacteria such as E. coli and Salmonella in the original sewage as many of them die during the processing because the conditions are not appropriate for them. It is also important to reduce the amount of organic compounds in the effluents released into rivers from sewage works. If this is not done, then microbes naturally present in the river use the organic compounds as a source of energy and reproduce in huge numbers. Since they respire aerobically, they use up much of the oxygen dissolved in the water, leaving little for other organisms such as invertebrates or fish, many of which will die. Sewage must therefore be treated to reduce the amount of organic matter, and thus reduce the Biological Oxygen Demand or BOD, defined as the amount of oxygen required by the aerobic microbes to decompose the organic compounds in a sample of water.
The process of sewage treatment can be thought of as a complex form of composting. The compost heap which you may have in your garden is like a miniature sewage treatment works. The centre usually becomes anaerobic as existing oxygen is used up. Closer to the top of the heap aerobic processes take place. Apart from the raw material, the other big difference between a sewage treatment works and a compost heap is that inside a compost heap, temperatures become high – well above 60 °C – which is detrimental to most species of microbes, but in which some can flourish.
Sewage works rely on the diverse capabilities of microbes for the complete process to be effective. Name three types of microbial activity that are used in the process and one that is not.
Aerobic and anaerobic respiration and fermentation play an important role in sewage treatment. Photosynthesis is generally not used in the sewage works because it is a process that builds organic compounds from carbon dioxide, whereas the objective of sewage works is to break down organic compounds.
Many of the microbes used in food and in industry are anaerobic so that they must be cultured in conditions without oxygen. In principle, anaerobic culturing is very similar to aerobic culturing. However, it does involve some specialist equipment and procedures which are described in Box 1.
Box 1 Growing anaerobic microbes and large-scale culturing
Why do you think anaerobic culturing would be more challenging than aerobic culturing?
Although some anaerobic microbes can tolerate small amounts of oxygen, many are obligate anaerobes, which means they are killed by oxygen. When culturing them, special efforts must be made to ensure that at no time during their manipulation using aseptic techniques are they exposed to oxygen.
Microbiologists have devised a range of methods for culturing anaerobic microbes. One of the most important pieces of equipment is a cabinet flushed with a gas such as nitrogen which allows manipulations to be carried out in an oxygen-free environment. The operator carries out the work through rubber gloves connected to the inside which prevents oxygen from entering the cabinet. When anaerobic microbes are cultured on Petri dishes, the dishes are also stored in airtight containers that are constantly flushed with nitrogen or carbon dioxide to keep them anaerobic. Many anaerobic organisms also need some unusual elements to grow, and these are added to the culture media.
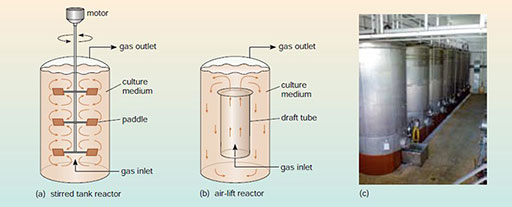
Growing anaerobic microbes on a large scale is essential for the industrial processes of brewing beer, making wine and carrying out other types of fermentation and for producing large quantities of microbes, for example yeast for bakeries. This is often done in giant metal vats called fermentation reactors which can hold many hundreds or thousands of litres of microbial culture (Figure 6c). The vats are provided with sensors to measure temperature and nutrient levels that allow computers to control the conditions within the reactors to ensure maximum growth of the microbes. One of the difficulties with such cultures is preventing the microbes from settling to the bottom of the vats.
Why is this likely to be a problem?
Those microbes which settled first would be covered by those settling later and therefore would not be able to access the nutrients in the culture medium. They would probably die and decompose, and their breakdown products could then contaminate the culture, as well as resulting in a lower yield of microbes from the whole vat.
To prevent settling, the vats can be stirred mechanically by large paddles (Figure 6a) or oxygen-free air (mostly nitrogen) can be bubbled through to circulate the contents of the vat (Figure 6b). If aerobic microbes are being cultured, then similar vats are used but air or oxygen is bubbled through.
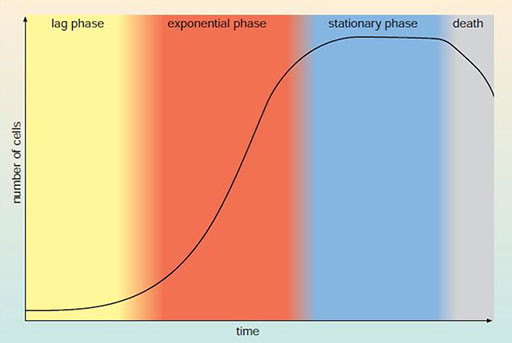
The growth of populations of microbes in the fermentation reactors (and in all other situations too), follows the basic pattern shown in the growth curve in Figure 7. When microbes are first added, they begin growing and dividing slowly as their enzyme systems adjust to the presence of new nutrients. This is referred to as the lag phase. After a period of time the microbes begin to grow and divide very rapidly to take advantage of the favourable growth conditions – the exponential phase. There may then come a point at which the microbes have used up some vital nutrient in the growth medium and they are no longer able to divide – the stationary phase. Eventually the microbes become old and start to die – the death phase. These growth stages are important for industrial processes. To produce the maximum amount of microbes and microbial products, they must be constantly provided with new nutrients to prevent them entering the stationary phase, hence the valves and tubes entering the fermentation reactors in Figure 6c. These are then harvested by being extracted from the medium in which the microbes are growing.
Conclusion
Most of the microbes in humans live a harmonious existence with human cells, but disease and infection can be caused when this balance is disrupted or when the body or immune system is weakened. Microbes can transfer genetic information between one another and this is one of the means by which antibiotic resistance is spread amongst the microbial population. The process is the origin of MRSA.
Beneficial microbes have an important role to play in the breakdown of human waste in sewage plants.
Acknowledgements
This course was written by Audrey Brown.
Except for third party materials and otherwise stated (see terms and conditions), this content is made available under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 Licence.
The material acknowledged below is Proprietary and used under licence (not subject to Creative Commons Licence). Grateful acknowledgement is made to the following sources for permission to reproduce material in this course:
Course image: Heiti Paves in WikiMedia made available under Creative Commons Attribution-ShareAlike 3.0 Licence.
Figure 1 CDC/Janice Carr & Jeff Hageman
Figure 2 Janice Carr/CDC
Figure 3 (b) Dr L Caro/Science Photo Library
Figure 6 (c) Kyle Laughlin/Flickr Photo Sharing.
Every effort has been made to contact copyright owners. If any have been inadvertently overlooked, the publishers will be pleased to make the necessary arrangements at the first opportunity.
Don't miss out:
If reading this text has inspired you to learn more, you may be interested in joining the millions of people who discover our free learning resources and qualifications by visiting The Open University - www.open.edu/ openlearn/ free-courses
Copyright © 2016 The Open University