Public Health Approaches to Infectious Disease
Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Saturday, 20 April 2024, 8:38 AM
Public Health Approaches to Infectious Disease
Introduction
This course focuses on the strategies available in the twenty-first century to tackle major infectious diseases, including pneumonia, diarrhoea, malaria, HIV/AIDS, measles, tuberculosis and infections of the newborn. Infection poses a major threat to public health all over the world, but it disproportionately affects children in low- and middle-income countries (LMICs), where pneumonia and diarrhoeal diseases are the two largest causes of death among those under five years old.
The aim of the course is to give you clear insights and memorable examples of:
- the importance of surveillance and mapping of infectious disease outbreaks in human populations and their impact on human lives
- the biological, socioeconomic and other circumstances influencing the transmission of pathogenic (disease-causing) bacteria, viruses and parasites
- the success of some low-cost, community based public health campaigns to prevent, treat or control infections, illustrated by a video of a unique rural health programme in Ethiopia and a case study of how guinea worm disease has been brought to the brink of global eradication
- the challenges that must be overcome in order to make further progress in reducing the burden of infectious disease and meeting the associated Millennium Development Goals (MDGs)agreed by the international community in 2000.
This OpenLearn course is an adapted extract from the Open University course : SK320 Infectious disease and public health.
Learning outcomes
After studying this course, you should be able to:
define and use, or recognise definitions and applications of, each of the glossary terms for the course
summarise the main features of the current global burden of infectious disease and the public health movement that has evolved to reduce its impact, emphasising the contributions of epidemiology, water quality, sanitation and hygiene, global infectious disease surveillance networks, and evidence-based interventions such as vaccination programmes
use appropriate examples and interpret unfamiliar examples presented to you, to illustrate successful public health strategies that: use education to support behavioural changes that enable people to protect themselves, their children or other community members from infection; promote resistance to infection in the human host; isolate a source of infection to prevent it from being passed on; tackle an environmental source of infection
consider a range of public health strategies, including unfamiliar examples, and identify the levels of prevention (primary, secondary, tertiary) involved in their implementation
use or analyse examples of public health interventions to illustrate the importance of international and national prevention programmes, community participation and community health workers in controlling infectious disease.
1 The global burden of infectious disease
In 2008, a total of 8.8 million children died before their fifth birthday – half of them in Sub-Saharan Africa. Pneumonia, diarrhoea, malaria, HIV/AIDS and measles caused 44% of these deaths in children under five years (Figure 1). Newborn deaths from sepsis and tetanus in the first four weeks of life accounted for a further 7%, and many of the 17% of deaths attributed to ‘other causes’ were also due to infection, including TB and meningitis exacerbated by malnutrition, which contributes to over one-third of all child deaths. (Note that the ‘non-infectious neonatal causes’ depicted in the figure refer to deaths resulting from prematurity, birth asphyxia, trauma and congenital abnormalities.)
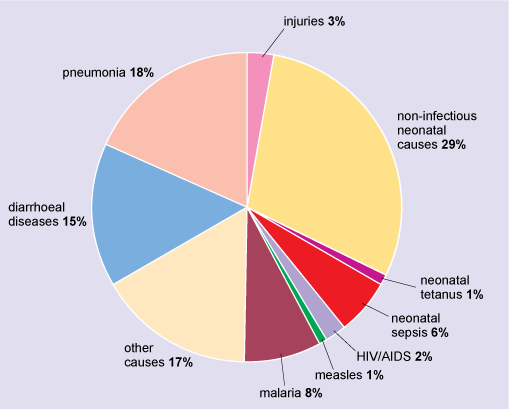
The figure is a pie chart showing the percentages of the total deaths among children in 2008 due to different causes, as follows: non-infectious neonatal causes, 29 per cent; pneumonia, 18 per cent; diarrhoeal diseases, 15 per cent; malaria, 8 per cent; neonatal sepsis, 6 per cent; injuries, 3 per cent; HIV/AIDS, 2 per cent; measles, 1 per cent; neonatal tetanus, 1 per cent; and all other causes combined, 17 per cent.
Although the impact of infectious disease episodes and deaths is disproportionately felt among the populations of low- and middle-income countries (LMICs), the richer nations of the world have not escaped. For example, infectious and parasitic diseases were responsible for 201 751 admissions to National Health Service (NHS) hospitals in England in the budget year 2010–2011, an increase of 10% on the previous year – the biggest percentage rise of any disease admission group (Hospital Episode Statistics, 2011). It was largely due to a 29% increase in admissions of children aged under 15 with non-hepatitis, non-influenza viral infections, and it confirms a rising trend. This category of hospital admissions has risen by 84% in England since 2006–2007.
1.1 Acute respiratory infections
Influenza, pneumonia and other acute respiratory infections (ARIs) are often forgotten in the focus on TB, HIV/AIDS and malaria, but they rank first among infectious causes of disease worldwide:
- The average global burden of seasonal influenza alone is about 600 million cases per year, of which 3 million result in severe illness, causing between 0.25 and 0.5 million deaths (WHO, 2009a). Pandemic influenza occurs at unpredictable intervals with the emergence of new variant influenza viruses.
- The ‘swine flu’ epidemic in 2009 caused by an H1N1 virus spread rapidly to 208 countries; the speed of transmission overwhelmed the capacity for laboratory confirmation of cases, especially in low-resource countries, but clinical diagnosis suggests that several million people were symptomatically infected and at least 12 220 died (WHO, 2009b).
- Pneumonia is the largest infectious cause of death among young people globally (see Figure 1), accounting for an estimated 1.5 million deaths in children under 5 years – more than TB, HIV/AIDS and malaria combined in this age group. Pneumonia is mainly due to the bacteria Streptococcus pneumoniae and Haemophilus influenzae type b (Hib), the respiratory syncytial virus (RSV) and parainfluenza viruses, all of which also affect elderly people worldwide. A major underlying cause of susceptibility to these pathogens is inflammation of the lungs due to atmospheric pollution; this is a major problem particularly among women, children and elderly people who are persistently exposed to indoor smoke from cooking fires in poor rural communities.
- The World Health Organization (WHO) estimates that up to 18 million episodes of pneumococcal disease and around 16 million episodes of RSV disease occur globally every year.
1.2 Diarrhoeal diseases
Worldwide, there are about 2 billion cases of diarrhoeal disease every year, including cholera, dysentery (bloody diarrhoea), giardiasis and a long list of bacterial and viral causes. They are the second largest infectious cause of death among young children (Figure 1), killing about 1.4 million annually, 80% of them under two years of age (WHO, 2009c). Even in the USA, the richest nation on Earth, diarrhoeal diseases cause an estimated 38.4 million episodes annually and around 1700 deaths (Scallan et al., 2011).
The pathogens causing diarrhoeal diseases are transmitted in contaminated food and water and from hand to mouth (the faecal–oral route). A major underlying cause is the shaming fact that in 2010 around 780 million people (11% of the global population) lacked access to improved sources of drinking water (Figure 2), and 2.5 billion – 37% of the world’s population – had no access to basic sanitation (UNICEF and WHO, 2012). However, steady progress is being made: in the 20 years from 1990 to 2010, an estimated 2 billion people gained access to improved drinking water and 1.8 billion gained access to improved sanitation (i.e. a covered pit latrine or better). These changes are gradually reducing the impact of diarrhoeal diseases on children’s health.

The figure comprises two photos. In (a), a boy is crouched beside a shallow, dirty stream and is using a plastic bottle to collect water. In (b), the boy is drinking the water from the bottle.
1.3 Tuberculosis
Tuberculosis (TB) has overtaken HIV/AIDS globally as the largest infectious cause of death by a single pathogen. Kaufmann reports that in 2011:
- Every minute of every day, nearly 20 people were infected with Mycobacterium tuberculosis and four people died from TB.
- One-third of the global population (well over 2 billion people) were carriers of TB bacteria.
- There were over 9 million new or relapsed active cases.
- Over 2 million people with chronic TB died.
Although the prevalence of TB is highest in the poorer countries of South-East Asia and Sub-Saharan Africa (Figure 3), it is resurging in Eastern Europe and increasing in the richest parts of the world. For example, there were over 9000 new cases of TB in England and Wales in 2011, most of them in London (HPA, 2012).

In this photo, the health worker is dispensing the medication from a small spoon into the palm of the woman’s hand.
1.4 HIV/AIDS
Worldwide, HIV incidence (the number of new cases occurring in a given period, usually one calendar year) has stabilised and deaths have been declining in recent years (UN, 2010). However, the impact on the global burden of HIV-related disease is still huge.
Global HIV incidence stabilised at around 2.7 million new HIV infections annually between 2007 and 2010 (the most recent year for which data are available at the time of writing). AIDS-related deaths fell from 2 million in 2008 to 1.8 million in 2010 due to the expansion of access to effective antiretroviral therapy. One outcome of this success is that HIV prevalence (the number of people living with HIV infection) is steadily increasing – to 34 million in 2010. Just over 2 million of those people were children under 15 years infected via mother-to-child transmission (WHO, UNAIDS and UNICEF, 2011).
People with HIV are primarily in LMICs, but richer parts of the world are also affected. For example, according to the Health Protection Agency, 91 500 people in the UK were estimated to be living with HIV at the end of 2010, of whom 6660 were newly diagnosed in that year and around 24% were unaware of their infection status (HPA, 2011a).
1.5 Malaria
The prevalence and incidence of malaria has also been steadily decreasing worldwide, but 216 million new cases still occurred in 2010, with an estimated 655 000 deaths in that year, mainly among young children and pregnant women. It is a shocking truth that an African child dies from malaria every 60 seconds. Although there were 126 000 fewer deaths globally in 2010 than in 2009, malaria still accounted for 22% of the deaths of African children (WHO, 2011a).
In October 2011, some progress was announced from large-scale clinical trials of the RTS,S/AS01 malaria vaccine, which reduced the incidence of new infections among young African children by 50% (RTS,S Clinical Trials Partnership, 2011). This is a significant breakthrough, representing the first vaccine with established clinical effectiveness in preventing a human infectious disease caused by a parasite.
However, it is not yet known how long the protection will last, and 50% efficacy is well below the desired 95% achieved by some well-established vaccines, e.g. against measles or diphtheria. But the RTS,S/AS01 vaccine also includes surface antigens from hepatitis B viruses and gives good protection against the latter. Combined (or combination) vaccines such as this one are highly effective because they protect children against two or more diseases at the same time.
Can you identify any other combined vaccines from your own experience?
You may have suggested the MMR vaccine against measles, mumps and rubella; or the DTP vaccine against diphtheria, tetanus and pertussis (whooping cough).
1.6 Other infectious disease headlines
Here are some other estimates from the WHO (accessed in 2011).
- Over 350 million people are chronically infected with hepatitis B virus (HBV) and 130–170 million with hepatitis C virus (HCV), causing over 1 million deaths from liver disease and hepatic cancer annually (WHO, 2008, 2011b).
- Excluding HIV and HBV, there are around 350 million new cases of the major sexually transmitted infections, including gonorrhoea, chlamydia and syphilis, which has a disproportionate effect on infants. Approximately 12 million new infections with Treponema pallidum pallidum occur every year, including 1.5 million babies born with congenital syphilis – the most common infection passed from mother to newborn baby. This is more prevalent even than congenital HIV, but far less publicised. In Africa alone, congenital syphilis causes the death of almost 500 000 babies every year (WHO, 2007).
- Around 1.5 billion people are infected with intestinal worms. A typical child in a poor rural environment in a low-income country commonly carries around 1000 hookworms, roundworms and whipworms, causing anaemia, stunted growth and increased vulnerability to other infectious diseases (WHO, 2012a).
- The so-called ‘neglected tropical diseases’ include Schistosoma parasites, which infect 207 million people worldwide – 85% of them in Africa, causing an estimated 200 000 deaths annually. Around 12 million people in 88 countries are chronically infected with Leishmania parasites, which cause severe cutaneous (Figure 4a) or visceral (Figure 4b) disease (WHO, 2012b).

The figure comprises two photos. (a) shows the face of a child with an oval-shaped ulceration on the left cheek. The child shown in (b) has a lean body, as evidenced by the outline of his ribs, but has a very distended abdomen.
- Around 500 000 people are blinded by the microscopic parasitic worm Onchocerca volvulus (WHO, 2012c) and over 120 million people worldwide are infected with Wuchereria bancrofti, the parasite causing lymphatic filariasis (WHO, 2012d).
- The viral haemorrhagic fevers are epidemic-prone diseases, which are increasing their geographical range and the number of people affected. Annually, it is estimated there are:
- 200 000 cases of yellow fever, causing 30 000 deaths
- 300 000–500 000 cases of Lassa fever, causing 5000 deaths
- up to 50 million dengue virus infections, including at least 250 000 cases of haemorrhagic fever and 24 000 deaths (WHO, 2012e).
With this daunting background in mind, the next section illustrates the diversity of public health approaches to controlling the huge burden of infectious diseases. An additional aim is to demonstrate the importance of addressing local needs and engaging local communities in interventions to improve public health, as you will see particularly in a slidecast on ‘Infectious disease and public health in rural Ethiopia’ in Section 4 (Video 1), and when you read about the guinea worm eradication campaign in Section 5.
2 The public health approach
The term public health refers to the ‘science and art of preventing disease, prolonging life, and promoting health’ (Winslow, 1920) and encompasses everything affecting the health of a population as a whole, rather than the individuals of which it is composed. A population may be all members of a nation or geographical region, or a defined group, for example all children under five years of age, all members of a minority ethnic group, or all women during the potential childbearing years. Public health is also concerned with non-communicable diseases, for example cancers, cardiovascular diseases and diabetes.
Here we focus specifically on the public health approach to infectious disease. This encompasses four broad areas of work:
- surveillance, monitoring and reporting of disease outbreaks and analysis of epidemiological data to shed light on the underlying causes, and inform actions to bring outbreaks under control
- direct intervention to prevent infection, e.g. through vaccination, reducing environmental sources of pathogens, or isolation and treatment of infected individuals
- education to promote behaviour change that reduces the risk of infection, or reduces the impact of an infectious disease outbreak
- organising and supporting community action to promote and sustain a healthier population and local environment and to coordinate community responses to outbreaks of infectious disease.
All of these areas are addressed in the rest of this course after a very brief review of the origins of the public health movement.
2.1 Threats to public health from urbanisation and industrialisation
Sanitarianism
The public health movement began in England in the nineteenth century in response to the huge toll of deaths from infectious disease in the urban slums and overcrowded tenement buildings that sprang up to house the influx of workers during the Industrial Revolution. An inspirational group of philanthropists founded the ‘sanitary movement’ or ‘sanitarianism’, with the aim of protecting the public health from sickness, which they recognised arose primarily from the polluted urban environment of the period.
The term ‘public’ encapsulates their focus on protecting the health of the population as a whole, rather than on treating or preventing disease in its individual members, and this emphasis characterises the public health approach today.
Quarantine
Quarantine is a period of enforced isolation or restriction of travel or activity. It is one of the oldest forms of public health intervention, pre-dating the germ theory of disease. In the nineteenth and early twentieth centuries, ‘fever’ hospitals and TB sanitariums were built outside major centres of population in Europe and the USA, to quarantine their patients away from the rest of society. This approach is still being applied in modern times: for example, in 2003, an isolation hospital was constructed in Southern China to quarantine people infected with the severe acute respiratory syndrome (SARS) virus.
Epidemiology
From its earliest period, the advocates of public health strategies for tackling infectious disease promoted an evidence-based approach, collecting systematic data on the incidence and prevalence of disease, the geographical location, socio-economic circumstances and behaviour of cases, and the impact of interventions on subsequent disease rates. The insistence on evidence led to the gradual development of a new academic discipline – epidemiology – the collection, analysis and interpretation of data on the occurrence, distribution, potential causes and control of diseases, disorders, disabilities and deaths in populations.
Epidemiology remains central to modern public health in the twenty-first century, but the methods of data collection now involve global monitoring and surveillance networks and huge online databases.
2.2 Public health surveillance and response in a globalised world
The rise of holidays abroad, cheap air travel, and the mass population migrations triggered by conflict and economic hardship are characteristics of the modern world. It is not that people did not travel in the past, but that the opportunities and the speed of travel are much greater now, so public health systems are faced with the challenge of controlling new infections that can spread globally in a very short time. Similarly, trade routes still transport infected goods within countries as they have always done, but air freight enables infectious agents in foodstuffs to travel between continents in less than a day.
Globalisation requires global responses to prevent potential infectious disease pandemics. The gradual expansion of global health surveillance and response systems during the twentieth century through the efforts of governments and international organisations, such as the United Nations (UN) and WHO, was given new urgency by the HIV/AIDS pandemic from the mid-1980s onwards (Castillo-Salgado, 2010). This trend was accelerated by the emergence of SARS in 2003 and the identification of at least 30 other previously unknown human pathogens in recent decades. Ongoing concerns about possible pandemic strains of influenza virus and the rapid increase in drug-resistant strains of TB and malaria were additional factors in prompting the 194 member states of the WHO to approve revised International Health Regulations in 2005.
2.2.1 International Health Regulations: IHR (2005)
The main aim of the International Health Regulations (IHRs) or ‘IHR (2005)’ is to ensure early warning and prompt action to contain any public health emergency of international concern. The obligations include the adoption of seven areas of work (Box 1) and the commitment by member states to improve their ‘real time’ reporting of disease outbreaks to WHO via round-the-clock communication channels.
Box 1 Seven areas of work covered by WHO IHR (2005)
- Foster global partnerships.
- Strengthen national disease prevention, surveillance, control and response systems.
- Strengthen public health security in travel and transport, particularly at designated airports, seaports and ground crossings.
- Strengthen the WHO global alert and response (GAR) systems and standardised approaches to contain outbreaks of major epidemic-prone diseases and dangerous and emerging pathogens with the ability to cause serious health impact and to spread rapidly across borders (e.g. meningococcal meningitis, cholera, viral haemorrhagic fevers such as dengue and Lassa fever, yellow fever and other vector-borne viral infections, plague, anthrax, human influenza caused by a new subtype, poliomyelitis due to wild-type polio virus, smallpox and SARS).
- Strengthen the management of specific risks.
- Sustain rights, obligations and procedures.
- Conduct studies and monitor progress.
2.2.2 The WHO Global Outbreak Alert and Response Network
The central coordinating body within the WHO’s surveillance function is the Global Outbreak Alert and Response Network. There are now numerous international surveillance and response programmes (ISRPs), networks and online databases recording outbreaks of notifiable diseases, i.e. cases that health workers are legally required to notify (report) to a designated agency or public health officer.
The Global Influenza Surveillance Network illustrates the scope of one of the largest ISRPs: it consists of 111 national influenza detection centres in 83 countries around the world and four influenza reference laboratories in the USA, the UK, Japan and Australia. The reference laboratories collect and analyse influenza strains from the detection centres to give early warning of new variants that could pose a major risk to global health.
The IHRs incorporate the recognition that interventions that affect trade and travel also have the potential to affect the human rights of the individual.
Suggest some examples of interventions that have human rights implications for individual liberty and freedom to travel.
You might have considered border health checks and whether people who appear ill should be excluded or placed in compulsory quarantine. For example, during the swine flu pandemic, some airports introduced infrared cameras to identify and exclude passengers with a fever. Some countries require travellers to carry international vaccination certificates before they can enter, but this has implications for individuals who oppose vaccination and who may be prevented from travelling.
2.2.3 National surveillance agencies
The ability of national surveillance, response and reporting systems in WHO member states to monitor outbreaks of infectious disease of public health importance are less developed in LMICs where major disease outbreaks most often occur. But strenuous efforts to help them catch up are being made by agencies in wealthier countries.
The UK has four such agencies:
- the Health Protection Agency in England
- the National Public Health Service Wales
- Health Protection Scotland
- the Department of Health, Social Services and Public Safety, Northern Ireland.
The functions of the public health agencies in the four nations of the UK are similar and are encapsulated in the Act of Parliament that created the Health Protection Agency (HPA) in England (HM Government, 2004). Principally, the agencies all function to protect the community (or any part of the community) against infectious diseases and other dangers to health through surveillance and data analysis, and to provide advice and information to the general public, health professionals and national and local government.
The HPA also provides expertise to assist the British Commonwealth countries and Brazil, Russia, India, China and South Africa (known collectively as ‘BRICS’) to implement the WHO International Health Regulations – IHR (2005). Projects include:
- building meningococcal serology capacity across Sub-Saharan Africa
- improving public health emergency preparedness and response in India
- developing an influenza surveillance network across South America to detect antiviral drug resistance (HPA, 2011b).
The huge range of outbreaks reported via national infectious disease surveillance networks can be judged from the ‘snapshot’ in Table 1, based on data published in the international journal The Lancet Infectious Diseases in the four months from August to November 2011.
| Country, region or town | Infectious disease outbreak |
|---|---|
| Cambodia | 6 deaths (all children under 15 years) from H5N1 avian influenza |
| Canada, Ontario | 80 cases of Clostridium difficile in hospitals, causing 21 deaths |
| Central African Republic | 57 cases and 16 deaths from Vibrio cholerae infection |
| Congo, Brazzaville | more than 7000 cases of chikungunya, a mosquito-borne viral disease causing fever and prolonged arthritic inflammation of the joints |
| India, Eastern Uttar Pradesh and Bihar | more than 2000 cases and 400 deaths from mosquito-borne Japanese encephalitis virus and enterovirus infection from contaminated water |
| France, Vaucluse and Somme districts | 8 cases of botulism traced to eating contaminated green olive tapenade or tomato paste from a French food company |
| Pakistan, Punjab region | more than 4000 cases and at least 8 deaths from dengue fever, causing the closure of all schools in Lahore for 12 days |
| South Sudan, Jur River county | 12 new cases of cutaneous anthrax and 777 cases of guinea worm disease |
| England, Scotland and Wales | 250 infections and one death from Escherichia coli O157, possibly originating from leeks and potatoes |
| USA, Albuquerque, New Mexico | 5 cases and 3 deaths from hantavirus pulmonary syndrome, transmitted to humans from rodents |
| USA (24 states) | 109 infections and 23 deaths from listeriosis traced to Listeria monocytogenes in cantaloupe melons and lettuces |
| Vietnam (national epidemic) | more than 42 000 cases and 98 deaths from hand, foot and mouth disease, caused by picornaviruses |
| Zambia, Chama district | 278 cases and 5 deaths from anthrax, thought to have been contracted from contact with infected hippopotamus meat |
But such high-profile outbreaks are only the tip of the public health ‘iceberg’. Submerged below the level that excites media interest are the day-to-day public health routines of surveillance, direct intervention, education and community action that seek to control infection all over the world. Although these strategies save millions of lives every year and prevent many more episodes of infectious disease, they are largely disregarded outside public health circles.
The rest of this course will give you an insight into their diversity and the success of some public health campaigns to control – and in some cases eliminate – major infectious diseases.
2.3 Public health interventions
Surveillance and reporting are clearly essential to ensure coordinated action to protect public health, but the range of responses can be bewilderingly diverse. A useful way of thinking about direct public health interventions to control infectious disease is to distinguish between strategies that:
- use education to support behavioural changes that enable people to protect their own health or that of their children or other community members from infectious disease
- promote resistance to infection in the human host
- isolate a source of infection to prevent it from being passed on
- tackle an environmental source of infection.
For each of the categories 1 to 4, suggest one example of an intervention to control a specific infectious disease.
You may have chosen other examples, but here are some that illustrate the general principles.
- Education about hand washing with soap, particularly after defaecation and before handling food, is particularly effective at preventing diarrhoeal diseases (as you will read in Section 4.2.1).
- Vaccination with an inactivated preparation of influenza virus increases resistance to subsequent flu virus infection, provided the infective strain is the same as, or closely related to, a component of the vaccine (see the OpenLearn free course SK320_1 Influenza: A case study for more information). Vaccination programmes against a range of infectious agents are estimated to save the lives of over 2.5 million people, mainly young children, every year.
- Quarantine of infectious individuals has been practised for centuries, for example, in the isolation hospitals and TB sanitariums of the late nineteenth and early twentieth centuries, and during outbreaks of swine flu, bird flu and SARS.
- The provision of insecticide-treated nets (ITNs) is a highly effective environmental strategy for controlling the insect vectors of pathogens such as malaria parasites (Figure 5). ITNs not only protect the individuals sleeping under the nets, but they also reduce the local mosquito population by contact with the insecticide.
 ©© WHO/TDR/CrumpFigure 5 Insecticide-treated mosquito nets erected over sleeping mats offer effective protection from the mosquitoes that transmit malarial parasites (Plasmodium species).Show description|Hide descriptionFigure 5 Insecticide-treated mosquito nets erected over sleeping mats offer effective protection from the mosquitoes that transmit ...
©© WHO/TDR/CrumpFigure 5 Insecticide-treated mosquito nets erected over sleeping mats offer effective protection from the mosquitoes that transmit malarial parasites (Plasmodium species).Show description|Hide descriptionFigure 5 Insecticide-treated mosquito nets erected over sleeping mats offer effective protection from the mosquitoes that transmit ...The photo shows a sleeping mat on the ground which is enclosed by a mosquito net strung from ropes above it. A child seated on the mat is lifting the front of the net and emerging from the enclosed area.
Aside from vaccination programmes, what other major public health strategies could have a similarly huge impact on the control of infectious diseases in populations?
Among the most important strategies are the provision of clean drinking water, adequate sanitation and the safe disposal of sewage and refuse – exactly the same goals that the nineteenth-century founders of the public health movement campaigned for as basic human rights. The provision of effective, accessible and affordable health services is also vital.
Less visible, but no less significant, contributions to population health come from:
- the provision of transport and other infrastructures to enable widespread access to health and social services
- controls on the pollution of the environment by traffic, agriculture and industrial processes
- an education system that delivers a high rate of literacy in the population, particularly in women, which is strongly associated with reduced morbidity and mortality rates among their children
- gender equality in access to the means of subsistence, goods and services, including health care
- an economic structure that supports an adequate income, shelter and nutrition for all households
- a stable and equitable political system.
3 Levels of infectious disease prevention
The prevention of disease obviously has a potentially greater impact on public health than medical treatment, although – with the exception of vaccination programmes – infectious disease prevention has always been far less well funded or researched.
This section examines a hierarchy of public health interventions, which are traditionally considered to operate at three different ‘levels of prevention’. Although you should be aware that there is some artificiality in separating them in this way, they provide a useful framework to illustrate the diversity of public health strategies for preventing infectious disease.
3.1 Primary prevention strategies
Public health strategies aimed at the primary prevention of infectious disease seek to prevent new cases of infection from occurring by interrupting the transmission of pathogens to susceptible human hosts, or increasing their resistance to infection.
Vaccination operates at the level of primary prevention:
- directly, by increasing the resistance of the uninfected population to the pathogens from which the vaccine was prepared
- indirectly, by decreasing exposure to pathogens, because it reduces the proportion of infected individuals in the community who could transmit the infection to its unvaccinated members.
This protective effect is known as herd immunity, and the herd immunity level is reached when the ratio of immune-to-non-immune individuals is high enough to stop the infection circulating in the population because there are so few susceptible individuals.
Educating mothers about the benefits of breast feeding their babies exclusively for the first six months is another example of a primary prevention strategy. Breast feeding is promoted not only for its nutritional benefits but also to protect breast-fed infants against the pathogens that can contaminate feeding bottles, animal milk and infant formula prepared with unsafe water. Breast milk also contains maternal antibodies, so it provides babies with passive immunity against enteric pathogens.
Suggest some other examples of public health interventions aimed at the primary prevention of infectious disease.
You might have thought of many other examples in addition to our suggestions below.
- Distribution of free condoms in areas of high HIV prevalence, coupled with ‘safer sex’ education about sexually transmitted infections (STIs).
- Food safety legislation, inspection of catering premises and slaughterhouses, and education about hygienic food-handling practices to prevent outbreaks of food poisoning.
- Training community members to drain mosquito breeding sites near homes in endemic malaria areas, and distributing ITNs to cover beds at night.
- Education of community members who lack access to safe sources of water so that they know they should boil unsafe water before using it for drinking, cooking or mixing formula feeds for infants.
You will see as this course progresses that many other examples of public health interventions operate at the primary prevention level.
3.2 Secondary prevention strategies
Secondary prevention aims to detect new cases of infectious disease at the earliest possible stage and intervene in ways that prevent or reduce the risk of infection spreading further in the population. Some examples of how secondary prevention can be put into practice are described below.
Early treatment
This level of prevention involves infected (or exposed) individuals receiving early treatment to prevent the transmission of pathogens to susceptible hosts. Benefit to the individual may also result from treatment, but the aim from a public health perspective is to protect the community as a whole from further infections, rather than to aid the personal recovery of identified patients.
Education and health-related behaviour modification
Secondary prevention relies partly on educating the population about signs of illness that require prompt referral to the health service, coupled with systematic surveillance to detect and report cases quickly and respond with effective treatment. If the disease has the potential to generate an epidemic, it may be necessary to isolate (quarantine) infected individuals, who should also be educated about how they can prevent or reduce the risk of transmission to others.
Suggest examples of how the education of infected individuals could contribute to the secondary prevention of infection.
Some examples we thought of are:
- People with active TB counselled to cover their mouth when they cough, to avoid coughing close to other people, particularly in enclosed spaces, and to take their medication regularly.
- Pregnant women with HIV counselled about the importance of receiving antiretroviral therapy to reduce the risk of transmitting the virus to their baby.
- People with chlamydia infection counselled about abstinence and safer sex practices to avoid transmitting the bacteria to sexual partners.
Note that even if the condition is not curable by medical treatment, benefit to the community may also result if the education of infected people leads to health-related behaviour modification, i.e. long-lasting changes in behaviour that result in health gains, a reduction in health risks, or an increase in disease prevention. For example, the rates of new HIV infection among gay men in the UK and the USA declined after 1996 due to changes in sexual behaviour, but began rising again after antiretroviral therapy became widely available in high-income countries (CDC, 2001; HPA, 2011c).
Screening
Infected individuals can also be identified even before symptoms develop in systematic screening programmes, i.e. the application of a test or an investigation to large numbers of individuals to identify those at risk of developing a particular disease, or (in the case of infectious disease) those who are already infected. The screening service can target groups assumed to be at high risk; for example, people who are homeless or staying in migrant hostels are at the greatest risk of TB, so TB screening programmes may be directed towards these groups.
Clinical and/or microbiological screening programmes are a vital component of public health initiatives against infectious diseases all over the world, with the aim of secondary prevention as well as the treatment of individuals (Figure 6). If they are coupled with education on prevention among uninfected individuals given the ‘all clear’, screening programmes also contribute to primary prevention.

This photo shows two women, both carrying small children and queuing inside the health clinic. The women at the front of queue is holding out her hand while the seated healthworker takes a blood smear from one of her fingers.
Secondary prevention is most difficult where the infectious disease either has a prolonged asymptomatic (symptom-free) stage (e.g. for HIV this may last several years after infection), or can exist in an asymptomatic carrier state where the person becomes chronically infected but never develops disease symptoms and acts as a persistent reservoir of infection to others.
Suggest some examples (other than TB, HIV and malaria) that fit these criteria.
Your suggestions may have included viral hepatitis, typhoid, schistosomiasis, lymphatic filariasis, syphilis, chlamydia and gonorrhoea.
3.3 Tertiary prevention strategies
Medical treatment to prevent the worst outcomes of a disease in an individual is known as tertiary prevention. Although this may greatly improve the quality of life for that person, it has at most a limited impact on the spread of infectious disease. For example, physical therapies that support the rehabilitation of children with paralytic polio are at the tertiary level of prevention, i.e. they can reduce the impact of paralysis on the child’s quality of life, but they have no impact whatsoever on the spread of polio virus in a community.
However, tertiary strategies contribute to public health in a more subtle way. By alleviating the pain, distress and disability experienced by individuals, the community as a whole benefits from the input these people are enabled to make to the ‘social capital’ of all (Figure 7).

The photo shows a man, whose legs are distended by elephantiasis, standing over a small loom. He is weaving coir (the fibre extracted from coconut husks) to make a mat.
3.4 Combining prevention levels to promote public health
To illustrate how the hierarchy of prevention levels can operate in practice, consider our answers to the following worked example.
Example
Question
What measures can be taken against TB at the primary, secondary and tertiary levels of prevention?
Answer
Primary prevention: BCG vaccination and improved living standards, including better housing (reduction in crowding) and nutrition (improved host immunity).
Secondary prevention: screening programmes to detect cases of infection early (e.g. from sputum tests); treatment of early non-symptomatic infection with drugs such as isoniazid, or symptomatic TB with a multidrug regimen, ideally in a DOTS programme (see Box 2).
Tertiary prevention: drug treatment of severe complications such as tubercular meningitis, and physical rehabilitation therapy for extrapulmonary TB, e.g. affecting the skeleton and mobility. (Note: ‘extrapulmonary’ means ‘outside the lungs’.)
The same principles can be applied to other examples.
Identify the level of prevention operating in each of the following strategies to control diarrhoeal diseases in children in a rural village in a low-income country.
- Drilling a deep tube well to access clean water and pumping it to standpipes.
- Digging cesspits and building latrines.
- Vaccinating children against rotaviruses.
- Teaching parents how to make and administer oral rehydration salts (ORS) to children with acute diarrhoea.
- Educating parents and children about the importance of hand washing before preparing food and after defaecation or urination.
- Administering intravenous fluids to children with severe dehydration caused by persistent diarrhoea.
Strategies 1–3 and 5 are examples of primary prevention to reduce the number of new cases of diarrhoeal diseases.
Strategy 4 is secondary prevention because ORS shortens the duration of the illness in infected children, which reduces the spread of causative organisms. However, it may also be life-saving – and therefore a tertiary prevention strategy for some children.
Strategy 6 is tertiary prevention, aimed at saving lives.
Box 2 Directly observed therapy, short course (DOTS)
In order to control TB, patients must regularly take antibiotics over a prolonged period of several months. Failure to do so can lead to a relapse of patient health and the possible development and spread of drug-resistant forms of TB.
In order to improve drug compliance in patients, the WHO devised a five-component TB control strategy called 'directly observed therapy, short course' (DOTS). DOTS addresses the problem of drug compliance by having either a designated health worker or some other responsible person directly observe a patient each time they take their antibiotics. This simple observation strategy (listed below as item 3) is further supported by an additional four aspects of medical and political infrastructure:
- political commitment with increased and sustained financing
- case detection through quality-assured bacteriology
- standardised treatment with supervision and patient support
- an effective drug supply and management system
- monitoring and evaluation system and impact measurement
4 Public health successes in controlling infectious disease
In this section you will explore some major successes in public health interventions to control infectious disease, and see how these encouraging indicators of progress have been achieved. This will involve studying an additional resource: a slidecast about infectious diseases and public health in Ethiopia (Video 1).
4.1 Vaccination revisited
In principle, a vaccination is a relatively simple event, because it does not require any changes to social structures or long-term personal behaviour, both of which may be difficult to achieve or sustain. The success of vaccination programmes is not dependent on radical changes in society; it depends on the organisation, funding and delivery of vaccines to populations in need of protection from vaccine-preventable diseases (VPDs).
By comparison with other public health interventions that could have an equal or greater impact, such as the universal provision of clean water and sanitation, vaccination is a relatively cheap disease prevention and health promotion strategy. It has achieved some notable successes, a number of which are briefly summarised here.
When the WHO initiated the Expanded Programme on Immunization (EPI) in 1974, fewer than 5% of the world’s infants were fully immunised during the first year of life against the six main VPDs:
- tuberculosis
- poliomyelitis
- diphtheria
- tetanus
- pertussis
- measles.
In order to track progress towards increasing vaccine coverage, WHO member states agreed to use the proportion of infants (i.e. those under one year) receiving all three scheduled doses of the combined vaccine against diphtheria, tetanus and pertussis (known as ‘DTP3 coverage’, or sometimes ‘DPT3 coverage’) as the main indicator of immunisation programme performance. By 2010, DTP3 coverage in WHO member states was protecting 85% of infants against these three diseases, with a target to reach 90% by 2015 (WHO, 2012g).
Coverage with measles-containing vaccines has also increased worldwide to 83% globally among children aged 12–23 months. This campaign has achieved a reduction from 4 million cases of measles and 2.6 million child deaths in 1980, to fewer than 118 000 cases contributing 1% of deaths in children under five in 2008 (WHO, 2012h).
Polio, measles and neonatal tetanus are the VPDs at the top of the WHO’s target list for global eradication, following the successful campaign to rid the world of smallpox.
4.1.1 The eradication of smallpox
On 8 May 1980, the WHO announced that smallpox had been eradicated from the world. Global eradication refers to the permanent worldwide reduction of cases to zero, with no known sources of infection that could generate a new case.
The declaration that the world was free of smallpox came more than two years after the last recorded cases in the three countries where the smallpox virus had proved hardest to eradicate: Somalia, Ethiopia and Kenya.
The global campaign against smallpox began in 1967. Back then, the estimated prevalence of the disease was 10 million cases, it was endemic in more than 30 countries and was frequently imported to at least 12 further countries. Against this background, how was worldwide eradication achieved in little more than ten years? The answer lies in certain features of the smallpox virus, the efficacy of the vaccine that prevents it, and the manifestations of the disease, as explained in Box 3.
Box 3 Special features of smallpox as an eradication target
- Smallpox is a DNA virus with a relatively stable genome, which does not generate variant strains; therefore, the same vaccine could be used everywhere.
- Humans are the only host – there is no reservoir of smallpox virus in other animals or in the natural environment.
- The transmission of the virus from infected to susceptible individuals is relatively infrequent – typically, a person with smallpox infects two to five others (by comparison, a person with measles typically infects 10–20 susceptible contacts), so an outbreak spreads relatively slowly.
- Case finding is relatively easy because symptoms develop soon after infection, the smallpox lesions are immediately visible and characteristic in their appearance (Figure 8), and there is no asymptomatic or carrier state.

The photo shows the girl’s face and upper body covered in large closely spaced dimpled bumps which are the smallpox lesions.
- The smallpox vaccine is heat-stable, so it could be transported without loss of efficacy for mass vaccination campaigns in locations where refrigeration would have been impossible.
- A single vaccination produces long-lasting immunity, so there is no need to locate recipients for repeat vaccinations.
A key aspect of the public health approach to smallpox eradication was the adoption of a case containment policy. Instead of removing smallpox patients to hospitals for treatment, where the disease rapidly spread, most infected people were supported to remain in their own homes. Infected villages were sealed off until the patient recovered or died and all known or suspected contacts had been vaccinated.
4.1.2 The campaign to eradicate polio
Of the three vaccine-preventable diseases on the WHO target list for eradication – polio, measles and neonatal tetanus – the most progress has been made towards eradicating polio, largely because it has some similar characteristics to those already described for smallpox (see Box 3). One difference is that polio is caused by an RNA virus, but it does not generate the high number of variants typical of influenza viruses or HIV.
The global polio vaccination campaign began in 1988, a year in which an estimated 350 000 people – most of them children – developed acute flaccid paralysis (AFP) – the case-defining symptom of polio – as a result of infection with poliovirus. By 2010, the annual number of cases had dropped to 1352 and, in 2012, just three countries reported new cases: Nigeria, Afghanistan and Pakistan (WHO, 2012i). This progress was achieved through systematic mass polio vaccination campaigns (Figure 9) and an increased focus on case finding and case containment.

In this photo the practitioner is using a dropper to deliver drops of the vaccine into the child’s mouth, while holding the cheeks to keep the mouth open.
However, you might wonder why it is taking so long to eradicate polio, given that a 99% reduction in polio cases worldwide had already been achieved by 2001. Since then, the incidence has increased in some locations, particularly in Pakistan where new outbreaks have occurred. Rumours that fuelled opposition to vaccination in some communities have been the main cause of delay in achieving the WHO eradication target, not only for polio but also for measles and neonatal tetanus. But this delay should not overshadow the success of the polio campaign. In the 1980s, before the advent of mass vaccination, polio was paralysing 1000 children every day.
Activity 1 Infectious disease and public health in rural Ethiopia
This is the ideal time to study Video 1, a slidecast entitled ‘Infectious disease and public health in rural Ethiopia’. In addition to illustrating the infectious disease epidemiology of a Sub-Saharan African country, and the principal underlying causes of the high burden of infection, this slidecast will give you an insight into how a routine immunisation programme is organised to reach every child even in remote rural locations. It also serves as an introduction to some key points on non-vaccine interventions to prevent and control infectious disease, which form the focus of the next section of this course.
Transcript: Video 1 Infectious disease and public health in rural Ethiopia
Slide 1 (00:00)
This slide cast will introduce you to the realities of infectious disease in rural Ethiopia and how it is being tackled in every village by local health workers with basic training in disease prevention, diagnosis, treatment and control. My aim in giving you an insight into this astonishingly beautiful and hospitable country is to illustrate infectious disease and public health at local level and the impact it can make on a national scale. But I also hope it will challenge the negative image of Ethiopia often presented in the media.
Slide 2 (00:40)
Ethiopia is in the horn of East Africa. Its largely mountainous terrain can be clearly seen in the aerial view on the right.
Slide 3 (00:54)
Notice the huge expanse of Lake Tana in the north and the chain of lakes that mark the start of the Great Rift Valley, beginning in central Ethiopia – not far from the capital Addis Ababa – and extending south into Kenya.
Slide 4 (01:08)
This slide cast focuses on infectious disease in rural Ethiopia. But before we go there I want to make the point that Ethiopia has several large and expanding cities in addition to the capital Addis Ababa. There are grand buildings, modern hotels, busy traffic and many Orthodox Christian Churches, mosques and other places of worship in this intensely religious country. The shanty settlements in the foreground of this photo are being rapidly replaced by apartment blocks. But Ethiopia remains a largely rural country – only about 20% of the population live in urban conurbations.
Slide 5 (01:52)
Most of Ethiopia’s 83 million people live by farming in distributed rural communities, called kebeles in the Amharic language. The average kebele has about 1000 households and roughly 5000 inhabitants, led by a council of elected representatives. The round thatched houses in this photo are called tukul and are found all over Ethiopia.
Slide 6 (02:22)
As you can see, the Ethiopian countryside can be green and lush in the rainy season, supporting some of the country’s major exports: coffee, cut flowers and leather goods from animal hides. But the soil is poor after decades of subsistence farming and it soon dries out when the long rains end.
Slide 7 (02:45)
Animals are vital to the rural economy, but close proximity to their domestic animals exposes the rural population to infectious diseases with reservoirs in animal hosts, particularly intestinal parasites and the bacteria causing diarrhoeal diseases.
Slide 8 (03:05)
Most farming is done by hand or with simple ploughs pulled by oxen. Here the staple cereal crop, called tef is being harvested. The tiny grains are ground to make Ethiopia’s national dish – a thin pancake called injeera, which is unique to the country. I’ll come back to injeera when I talk about malnutrition in Ethiopia in a moment. First, let’s look more closely at a particular kebele and the infectious diseases that affect its inhabitants.
Slide 9 (03:40)
This is a map of Fura kebele, a rural area with a population of approximately 5000 people in the Southern Nations, Nationalities and Peoples Region of Ethiopia. The households are distributed across a wooded area, roughly five by ten kilometres, but some kebeles are larger than this. The inhabitants of Fura have carved out small fields in which to grow tef and graze their animals.
Slide 10 (04:11)
There are no paved roads, no piped water, and no electricity supply to the houses, so they are dark inside and difficult to photograph. Grass partitions divide the living and sleeping areas and the furniture is simple and stands on the mud floor.
Slide 11 (04:29)
This road in Fura is typical of how people get around in rural kebeles – mostly on foot, walking long distances, sometimes on a bicycle or in a donkey cart. The deep channels in the earth are caused by flood water during the rainy season, when the roads are often impassable, even with a four-wheeled-drive vehicle. The nearest health centre is 15 kilometres down this road, so if people need urgent medical help they may have to be carried there on a stretcher.
Slide 12 (05:03)
Many of the causes of infection in Ethiopia are related to the lack of clean water, which is a constant problem for many rural communities. Only 38% of the population has access to improved drinking water and many of these are in towns and cities – in the countryside, most people get their water from lakes, rivers and streams.
Slide 12 (05:28)
Some rural communities have deep communal wells, like this one in Fura. The water table is a very long way down in the dry season. The bucket is made from an old rubber tyre.
Slide 13 (05:43)
Unsafe drinking water presents a major health hazard to a large proportion of Ethiopia’s population. Here a horse, man and boy drink from the same muddy stream flowing from pasture where cattle were grazing. Shallow streams and pools like these make ideal breeding grounds for malaria mosquitoes and other vectors of infectious diseases such as onchocerciasis and schistosomiasis, as well as harbouring many pathogens causing diarrhoeal diseases.
Slide 14 (06:17)
People and their animals competing for scarce drinking water also increases the risk of water contamination by human and animal urine and faeces.
Slide 15 (06:29)
This chart shows the main causes of death in Ethiopia in children aged under five years. The high rate of diarrhoeal disease is one indication of the lack of access to clean water. As you can see from the four bars on the left, diarrhoeal disease, pneumonia, neonatal sepsis (which is mostly due to tetatnus) and HIV/AIDS account for the majority of these avoidable deaths. The 21% of deaths labelled ‘all other causes’ include many important infections such as measles, malaria and tuberculosis.
Slide 16 (07:11)
An idea of the challenges in rural communities can be gauged from this wall chart from a Health Centre in the small town of Modjo. It shows the top ten causes of serious morbidity (illness) among male children aged under five years who were sent from the surrounding rural kebeles because their condition could not be managed locally. The chart for girls of this age is very similar, but my photo wasn’t as clear. The prevalence of infection among the under fives is striking: the top ten causes of serious illness are non-bloody diarrhoea, pneumonia, acute urinary tract infections, dysentery (that’s bloody diarrhoea), infestation with helminths, infections of the skin and subcutaneous tissue, all other respiratory diseases, malaria, all other skin diseases, and typhoid fever.
Slide 17 (08:18)
Inadequate food hygiene standards and the practice of eating kitfo – raw beef or ox meat – at important festivals is another major source of infection. Beef tapeworm is prevalent and infestation with other intestinal worms is widespread, affecting over 50% of children, with major effects on their growth and development.
Slide 18 (08:40)
Ethiopia is commonly associated with famine, but such deep crises of absolute food insecurity are relatively rare. The more consistent problem is generalised protein energy malnutrition. The staple diet is injeera made from tef, which you saw being harvested earlier. Injeera is typically eaten from a communal plate with a hot lentil sauce and perhaps some stewed vegetables. Meat is only for special occasions in most families. Injeera is highly nutritious, but there often isn’t enough food to go around. Children in particular suffer from a persistent shortage of calories in their diet and a lack of vitamin A and iron because of the scarcity of vegetables.
Slide 19 (09:32)
These data come from the last national survey in Ethiopia conducted in 2005 and published in 2007. At that time, 38% of children under 5 years were underweight and 47% were stunted (short for their age). The extent of iodine and iron deficiency is demonstrated by the high rates of goitre and also of anaemia among young children. These conditions also affect many women of childbearing age. Malnutrition is a major contributor to susceptibility to infectious disease and premature death, and not only among children – over a quarter of women are chronically malnourished, which makes them particularly vulnerable during pregnancy, childbirth and breastfeeding.
Slide 20 (10:30)
Despite its many health problems, some of Ethiopia’s indicators of public health are better than the average for Sub-Saharan Africa, and steady progress is being made towards achieving the Millennium Development Goals for reducing child and maternal deaths. But there is a long way to go. For example, for every 1000 live births in Ethiopia, more than 4 women die from causes related to pregnancy, childbirth, postnatal infection or haemorrhage. This is roughly 50 times higher than the maternal mortality rate in the UK.
Slide 21 (11:11)
Faced with all these challenges to public health, in 2005 the government of Ethiopia began an ambitious programme to bring basic disease prevention and health promotion services to the entire population, now totalling over 83 million people. They have built a small Health Post in every kebele staffed by two full-time Health Extension Workers trained and paid by the Ministry of Health. There are now over 12 500 rural Health Posts like these and over 33 000 Health Extension Workers deployed in rural areas.
Slide 22 (11:55)
Here are two of them – Asafesh on the left and Almaz on the right. The Health Extension Workers are all young women – an innovation in Ethiopia where the majority of nurses and midwives, as well as doctors, are male. Asafesh and Almaz have graduated from the one-year residential training programme and now work in rural Health Posts in different regions of Ethiopia. They each work with another Health Extension Practitioner to take care of the 5000 inhabitants of their communities.
Slide 22 (12:33)
The vital importance of the Health Posts and their Health Extension Workers to the delivery of health services in Ethiopia is well illustrated by the pie chart on the left. Each Health Post is in a ring of five ‘satellite’ Health Posts, at a distance of 10-15 kilometres from the nearest Health Centre, which supplies and supervises the Health Extension Workers. The provision of health services in Ethiopia relies very heavily on this organisation of primary care, partly because of the remoteness of the rural population from the hospitals, which are all in the cities, but also because of the shortage of medical expertise: there are just 20 hospital beds and 2 doctors for every 100 000 population.
Slide 23 (13:26)
So what health services do Asafesh and Almaz provide for their communities? This Health Post wall chart lists the main components. Take a moment to read the list. Click on the ‘Pause’ button while you do this.
How many of the service areas are directly or indirectly concerned with preventing or controlling infectious disease? Immunisation and all of the environmental health and disease prevention and control packages are obvious examples, but infection control is also an important aspect of health care during pregnancy, labour and delivery and the postnatal period. It also figures prominently in many of the health education activities that Health Extension Workers conduct, for example, on handwashing, food hygiene and digging latrines.
Slide 24 (14:34)
Here is some of the basic equipment in Asafesh’s Health Post. It doesn’t have running water or a sink, so Asafesh carries water in a bucket from a nearby well and washes her hands with soap between patients, using a bowl in a corner of the room.
She has a pressure cooker for sterilising instruments, mainly used when she is attending births; there are syringes for giving immunisations and injectable contraception, and a stethoscope and blood pressure cuff.
Slide 25 (15:06)
The scales are for weighing adults (mainly pregnant women attending for antenatal care) and there is a delivery couch in a side room. However, around 90% of rural women choose to give birth in their own homes with a Health Extension Worker present or a traditional birth attendant. Postnatal sepsis and haemorrhage are the main reasons for the high mortality rate: remember it was 4.4 maternal deaths per 1000 live births in the bar chart you saw earlier.
Slide 26 (15:41)
Asafesh also a spirit burner, boxes of disposable syringes, packets of oral rehydration salts to treat diarrhoea, and sachets of PlumpyNut (an energy-rich paste given to malnourished children).
The scales made from a large bowl attached to a spring balance are to check children’s weight and growth rate. There is also a conventional weighing scale for young babies. Identifying children who are underweight is an important responsibility for Health Extension Workers. Supplementing the diet and giving vitamin A capsules help to protect malnourished children from infection.
Slide 27 (16:26)
Health Extension Workers have a very small stock of medicines for the 5000 people they serve. At the Health Post in Fura, Asafesh has only paracetamol syrup for pain, and mebendazole and trimethoprim sulphamethoxazole to treat intestinal worms. She has anti-malaria tablets (Coartem) and contraceptive pills and the injectable contraceptive suspension Depo-Provera.
There are iron and folic acid tablets for anaemia, tetracycline eye ointment for eye infections in newborns – mainly due to chlamydia transmitted from their mother’s birth canal – a first aid kit, cotton wool swabs, antiseptic, a thermometer, a torch and surgical gloves. That’s all.
Slide 28 (17:20)
Every Health Post has a kerosene, gas or electric refrigerator for storing vaccines and an insulated vaccine carrier lined with ice packs. The Health Extension Workers use this to collect their monthly supply of vaccines from the Health Centre 10 to 15 kilometres away. Remember that rutted mud road that Asafesh has to walk along to collect her supplies, unless she can get a lift from someone in a donkey cart. She also uses the vaccine carrier to keep vaccines cold when she provides outreach immunisation sessions in remote parts of the kebele.
Slide 29 (17:59)
Ethiopia follows the World Health Organization’s recommended Expanded Programme on Immunization (or EPI) for low resource countries. A fully immunised infant should receive all the vaccines listed on this slide before its first birthday. BCG vaccine protects them against the most serious forms of tuberculosis. The DPT-HepB-Hib vaccine is also known as pentavalent vaccine because it immunises against the pathogens causing five infectious diseases – diphtheria, pertussis (or whooping cough), tetanus, liver disease caused by hepatitis B viruses, and bacterial pneumonia and meningitis caused by Haemophilus influenzae type b. Ethiopia recently added PCV10 vaccine to the routine immunisation schedule to protect infants against pneumococcal pneumonia. Rotavirus vaccine to prevent the most common cause of diarrhoeal disease becomes routine in 2012.
Slide 30 (19:13)
Inside the Health Post, wall charts help Asafesh to keep track of her public health targets for the local population, including immunisations. The inside of all Health Posts are covered with monitoring charts like these.
Slide 31 (19:28)
This wall chart shows how Almaz has been achieving her targets for childhood immunisation coverage in her kebele, which is called Shera Dibandiba. ‘Protected at birth’ refers to neonatal tetanus protection induced by immunisation of the mother with at least two doses of tetanus toxoid during her childbearing years and one during the pregnancy. Neonatal sepsis is a major cause of newborn deaths; note that less than 80% of newborns in this kebele received this protection. Pentavalent-3 refers to infants receiving all three doses of this combined vaccine to protect them against diphtheria, pertussis, tetanus, hepatitis B virus and Haemophilus influenzae type b bacteria. Measles vaccine is given at 9 months in Ethiopia. Almaz is achieving around 90% coverage with pentavalent-3 and measles vaccines.
Slide 32 (20:36)
Immunisation clinics are mainly held at the Health Post, but all Health Extension Workers spend four out of five days visiting families in the surrounding area and teaching them about disease prevention and health promotion, for example in food preparation, breastfeeding, hand washing, waste disposal and digging latrines.
When Asafesh and her colleague are away from the Health Post they use this cardboard dial to indicate the direction they have gone in that day, so they can be found in an emergency.
Slide 33 (21:11)
One of Asafesh’s most successful campaigns has been to persuade and support the inhabitants of Fura to build a latrine for every household. Until everyone has access to a latrine, open defaecation in the fields remains very common. This is a major transmission source for parasitic worms and for the bacteria and viruses causing diarrhoeal diseases. Fura kebele, where Asafesh works, was the first village in the southern region to be declared ‘open defaecation free’ because every household had its own latrine. This one is in the yard behind the Health Post. Notice the yellow can of water for washing hands.
Slide 34 (21:58)
Handwashing is one of the simplest, cheapest and most effective of all public health measures against infectious diseases. Health Extension Workers have promoted the installation of handwashing sites like this one on latrines all over rural Ethiopia.
A 30% reduction of diarrhoeal diseases can be achieved by washing hands with clean water after defaecation and before food handling. Using soap reduces diarrhoeal illness by over 40%.
Slide 35 (22:36)
Another of the main activities of Health Extension Workers in malarious areas is to mobilise the community to keep their water tanks covered and to drain water collections where mosquitoes breed, like those on the left of this slide. Only 33% of Ethiopia’s children were sleeping under insecticide-treated nets at night in 2007, but the coverage is rising rapidly, thanks to the distribution of nets to every household by the Health Extension Workers. However, there are still over three million reported cases of malaria in Ethiopia every year. Asafesh and Almaz can diagnose malaria with the rapid test kit shown on the right and treat non-urgent cases themselves with simple drugs. But patients with malaria complications have to be referred to the nearest Health Centre, 10-15 kilometres away, for more specialised treatment.
Slide 36 (23:39)
This is Godino Jitu Health Centre, where Almaz refers patients that she and her colleague can’t manage in the rural community. It serves the surrounding population of 36 700 people and sees up to 300 clients every day. There is no operating theatre and it doesn’t have a fully qualified doctor.
Slide 37 (24:05)
Godino Jitu Health Centre has a staff of about 24 health workers, including 8 Health Officers with a shorter medical training than doctors, 10 nurses and 2 healthcare assistants, 2 laboratory technicians, a pharmacist and a druggist. It also has clerical staff to register patients and keep records.
Slide 38 (24:30)
Health Centres deliver services that cannot be provided at Health Posts, including HIV-testing and prescription of anti-retroviral drugs and medication to treat tuberculosis. The pharmacy at Godino Jitu is well stocked, mainly with drugs to treat infectious diseases.
Slide 39 (24:52)
One of the diagnostic tests that the Health Centre can provide is microscopic examination of blood films from patients with suspected malaria. The sink on the left is where the slides are stained for confirmation of a malaria diagnosis, but more important is the identification of the Plasmodium species so that the correct treatment can be given – for example, to children and pregnant women with acute malaria crises. This is beyond the scope of what Health Extension Workers can currently provide.
Slide 40 (25:27)
However, Health Extension Workers like Almaz and Asafesh are keen to increase their knowledge and skills, so they can offer even more health services to their local communities. The Open University is proud to have been involved in a unique programme to support the upgrading of Ethiopia’s rural Health Extension Workers, as Vice Chancellor Martin Bean saw for himself when he visited Almaz at her Health Post in 2011.
Slide 41 (25:58)
1000 Health Extension Workers began studying 13 upgrading modules in 2011, which were produced by Ethiopian health experts with the support of The Open University’s HEAT (Health Education and Training) team. If you are interested, you can see all the modules on the HEAT website. The focus in the modules is on infectious disease and its prevention, diagnosis, treatment and control, but the curriculum also includes modules on non-communicable diseases and mental health.
Slide 42 (26:34)
There is an increasing focus in many low and middle-income countries on the rising rates of chronic conditions such as hypertension, diabetes and heart disease. Ethiopia is ahead of the curve in planning to train all its rural Health Extension Workers in these new areas of health concern, which The Open University has helped to develop.
Slide 43 (26:58)
But Almaz and Asafesh – like the other 33 000 rural Health Extension Workers – will still be focusing most of their attention on improving the life chances of beautiful children like these, through immunisation, nutritional support and education on domestic and environmental hygiene. Their efforts are steadily raising the health indicators in Ethiopia, despite the challenges of an often harsh environment and a widely distributed rural population. Ethiopia’s local approach to public health provided on a national scale is leading the way in tackling infectious disease in Africa.
Slide 44 (27:42)
Amehseghinalehu – thank you!
If you cannot study the slidecast now, try to do so before you complete this course. Then answer the questions below. There will be other questions on rural Ethiopia later in this course.
- Which infectious diseases are covered by the Expanded Programme on Immunization (EPI) in Ethiopia?
- What percentage of infants was protected by vaccination in the community served by Almaz? Which of these vaccinations protected newborn babies indirectly?
Answer
Question 1
The routine EPI in Ethiopia includes immunisation against diphtheria, pertussis, tetanus, polio, hepatitis B viral diseases, meningitis and pneumonia caused by Haemophilus influenzae and Streptococcus pneumoniae bacteria, and measles; additionally, by 2013, vaccination against diarrhoeal diseases caused by rotaviruses will be added to the EPI.
Question 2
Almaz and her colleague were achieving close to 90% coverage with DTP3 and measles vaccine among the infants in their community. Around 80% protection of newborn babies from neonatal tetanus was achieved indirectly by immunising women with tetanus toxoid in their childbearing years and during pregnancy.
4.2 The importance of hygiene
In public health parlance, hygiene behaviour encompasses the wide range of actions taken by individuals to maintain a standard of cleanliness of their bodies, domestic environments and workplaces to prevent the transmission of infection. It includes all the personal actions associated with excretion and the disposal of human and animal waste and refuse, the washing of persons, clothing, implements and structures (e.g. floors, lavatories and latrines), the handling of domestic animals, and the preparation of food.
When clean water and sanitation were installed in London in the nineteenth century, the epidemics of cholera that had claimed thousands of lives rapidly came under control. However, typhoid fever continued to be a problem for several more decades. The eventual reduction in typhoid was ascribed to the increasing availability of piped water and soap inside domestic households, the safe disposal of waste water from houses, and the increasing social imperative for personal hygiene.
Name another infection that can be controlled by personal hygiene.
You might have thought of typhus, because frequent washing of the body and clothing reduces the frequency of its vector, the human body louse. Washing can also reduce the transmission of the mites causing scabies, an infectious inflammation of the skin.
Personal hygiene can also alleviate some of the suffering caused by secondary infections of inflamed tissues. For example, careful washing and drying reduces the secondary bacterial infections which often colonise the inflamed skin folds of people with elephantiasis resulting from the blockage of lymphatic vessels by filarial worms (Figure 10).

However, although personal hygiene is a matter for the individual, it also requires the provision of certain infrastructures (e.g. covered wells, water mains), the means to purchase certain goods (e.g. soap, domestic cleaning agents) and a culture that is supportive of personal, domestic and public cleanliness. These are all in short supply in the poorest parts of the world.
4.2.1 Hand washing with soap
The importance of the most obvious hygiene behaviour – thorough hand washing with soap – cannot be overestimated. Many intestinal microorganisms and worms are thought of as causing water- or food-borne diseases, and indeed they are often transmitted by these routes. However, they are also transmitted by the faecal–oral route, in which faecal contamination of the hands is transferred directly to the mouth (e.g. when children suck their fingers or people eat with unwashed hands), or indirectly when pathogens on the hands are transferred to food, drinks or utensils. These diseases are also transmitted by flies landing on faeces and then on food.
In most homes in high-income countries, the availability of soap and clean water for washing is taken for granted; but it is a luxury that millions of people elsewhere in the world can rarely afford (Figure 11).

In this photo a small child crouches on the ground while washing his hands with soap in a plastic bowl of water.
Think back to Video 1. What facilities did Asafesh have for washing her hands at her Health Post in rural Ethiopia?
Health Posts don’t have running water, so Health Extension Workers like Asafesh have to wash their hands between patients using a plastic bowl and water carried in a bucket from a nearby well. They are trained always to use soap.
Public health educators have increasingly understood the potential impact of hand washing on the incidence of many infectious diseases, as described in a major review article entitled ‘Hygiene: New Hopes, New Horizons’ (Curtis et al. 2011). According to the evidence reviewed by the authors, very significant reduction in diarrhoeal-disease episodes can be achieved by hand washing, especially if soap is used. They conclude that hand washing reduces diarrhoeal illness by around 30%, and if soap is used, the reduction is 43–47%. This huge reduction at very little cost per person justifies the authors’ conclusion that hand washing with soap may be ‘the single most cost-effective way of reducing the global burden of infectious disease’ (Curtis et al., 2011, p. 312).
In addition to transferring diarrhoeal pathogens and intestinal parasites, can you suggest any other infectious conditions that can be transferred by poor hand hygiene?
You might have thought of neonatal tetanus and sepsis (the pathogens are most often transferred to the cut stump of the umbilical cord), infection of the female reproductive tract during childbirth, and eye infections including trachoma (which can be prevented by thoroughly washing the face as well as the hands).
The article also points to the potential impact of other aspects of personal hygiene that can reduce the risk of infection, one of which was also mentioned in Video 1 (the avoidance of open defaecation in fields and the safe disposal of human faeces in well-constructed latrines). How does this practice reduce the risk of diarrhoeal diseases?
The safe disposal of faeces reduces the risk of certain pathogens being transmitted by flies, contaminating food crops or being washed by rain into sources of drinking water.
Another setting in which the importance of hand hygiene has been widely publicised relates to the prevention of infection transmitted between patients and staff in hospitals and other healthcare institutions. It illustrates how relatively simple public health interventions can have a significant impact on an important source of infection, even in high-income countries. This idea is explored in the next section.
4.2.2 Institutional hygiene and healthcare-associated infections (HCAIs)
In the first five years of the twenty-first century, the news media in the UK reported increasing alarm over rising numbers of cases of two bacterial infections believed to have been acquired by patients in hospitals, nursing and residential care homes and rehabilitation centres. The conditions are methicillin-resistant Staphylococcus aureus (MRSA) (Figure 12), which is resistant to the antibiotic methicillin, and ‘C.diff’ or Clostridium difficile infection (CDI). (Note that the antibiotic generally referred to as ‘meticillin’ in the UK, is known as ‘methicillin’ in most other parts of the world.)
The photo shows a small area of the culture plate. There are many small dark blue colonies and also many small white colonies, clearly contrasted against the pale brown agar.
MRSA and CDI are not the only healthcare-associated infections (HCAIs), but they are responsible for the most serious, sometimes fatal, cases in the UK. Often overlooked in media reports of HCAIs is the increasing transmission of methicillin-susceptible S. aureus (MSSA) and some other pathogens.
Why are staphylococcal infections a significant problem in healthcare settings, particularly in surgical wounds?
Staphylococci are normal commensal bacteria found in the upper respiratory tract, on the skin and the lining of the large intestine and vagina. Although they are endogenous on these external surfaces, they are easily transferred into wounds, where they cause tissue-damaging infections.
C. difficile is also found naturally in the large intestine, but only in about 3% of adults in the UK, where it is normally kept in check by competition with commensal gut bacteria. However, C. difficile can ‘overgrow’ in elderly or frail patients who are taking broad-spectrum antibiotics, which destroy competing bacterial species. It is easily spread as spores, which may be hard to eradicate from healthcare institutions where susceptible patients are most at risk of becoming infected. CDI results in severe ulceration of the large intestine (a condition known as pseudomembranous colitis), with painful, copious diarrhoea (NHS Choices, 2012).
The blame for outbreaks of HCAIs is attributed to poor institutional hygiene, including inadequate hand washing by staff in contact with patients. A vigorous campaign to reduce the transmission of HCAIs was initiated in UK hospitals and other healthcare institutions in the late 1990s, and has had significant success. But these infections still cost the NHS an estimated £1 billion per year, in addition to the pain and suffering of patients who acquire an HCAI (DH, 2012).
Surveillance
Surveillance has played a key role in tackling the problems posed by HCAIs.
Mandatory surveillance in England began in 2001 for MRSA and in 2005 for CDI, and all cases in English NHS hospitals have been reported to the Health Protection Agency since April 2007 via a web-based Surveillance Data Sheet. So-called ‘lab returns’ on the number of positive blood cultures (MRSA bacteraemia), and CDI-infected stool samples, are collected from each location.
Patients are now routinely screened for nasal carriage of MRSA before and at admission to NHS hospitals, and all stool samples received from people aged over 65 years with diarrhoea are tested for CDI, including samples sent in by general practitioners or GPs (family doctors in the UK).
Strict surveillance has enabled outbreaks of HCAIs to be tackled quickly by isolating patients, initiating ‘deep cleaning’ regimes of wards and equipment, and installing numerous alcohol-based hand-rub dispensers for use by staff and visitors (Figure 13).
Beside the compression-activated dispenser is a red and white sign which reads; Stop. Important Notice for all Visitors. Please sanitise your hands when ENTERING or LEAVING this area.
Infection Prevention and Control (IPC) service
Every NHS hospital now has an Infection Prevention and Control (IPC) service responsible for the prevention, surveillance, investigation and control of infection. This is achieved through mandatory education and the development and implementation of effective policies and procedures. Data on the rates of MRSA and CDI cases and the standards achieved by the IPC service are regularly reviewed by quality standards bodies in the four UK nations, for example the Care Quality Commission (CQC) in England.
Patients and staff are interviewed on their assessment of cleanliness in the environment, staff hygiene and on the availability of the equipment and services necessary to achieve the prevention and control of infections. If there is a cause for concern, the CQC makes unannounced inspections to ensure that appropriate guidelines are in place and being observed by staff.
Figure 14 illustrates the steady success in reducing the rates of MRSA and CDI in recent years, through the systematic application of two traditional public health measures – hygiene and surveillance.
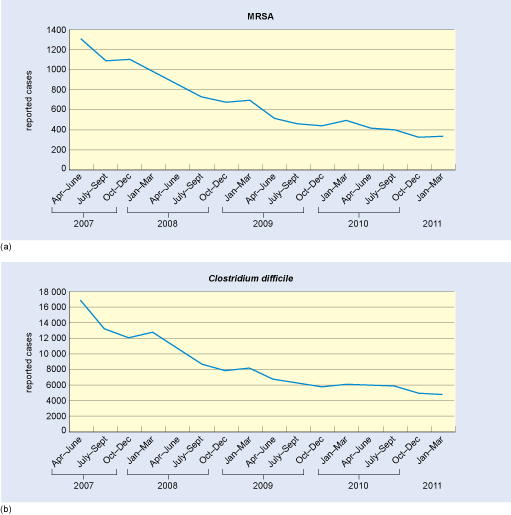
The graphs show the decline in reported cases of (a) MRSA bacteraemia and (b) Clostridium difficile infection over the four-year period. In both parts of the figure, the horizontal time axis is marked in quarters (3-month periods) from April–June 2007 until January–March 2011. The vertical axes are labelled reported cases: in (a), the axis is marked from zero to 1400 at intervals of 200; and in (b), the axis is marked from zero to 18 000 at intervals of 2000. The decline in reported cases of both infections was greatest between 2007 and 2009, with a smaller rate of decline between 2009 and 2011. MRSA cases fell from 1300 in April–June 2007 to 500 in April–June 2009 and then to 350 in Jan–March 2011. Clostridium difficile cases fell from 17 000 in April–June 2007 to 7000 in April–June 2009 and then to just under 5000 in Jan–March 2011.
4.3 Community action against infectious diseases
Raising the standards of public health is not simply a matter of training more doctors and nurses, building more hospitals and providing more funding for vaccines and treatments – although all of these make substantial contributions. As the earlier examples of mass vaccination campaigns and the promotion of hand washing with soap illustrate, much of the work involved in delivering effective public health strategies against infectious disease occurs in the community, outside the formal healthcare system.
As the famous definition of public health by Winslow (1920) states, ‘organized community effort’ is an essential element of successful strategies against infectious disease. The success of public health strategies all over the world, but especially in low-resource economies, and more particularly in rural areas and slum or shanty settlements, relies crucially on community action, mobilised and directed by community health workers like the Health Extension Workers in Ethiopia (Video 1), often with minimal training. For example, the malaria-screening service shown earlier in Figure 6 is run by a community health worker with basic training and rudimentary equipment.
Give an example of community action in rural Ethiopia based on your study of Video 1.
You might have thought of the campaign by Asafesh to persuade households in the Fura community to build latrines and ban open defaecation in the fields. Fura was the first kebele in Southern Ethiopia to become 100% free of open defaecation (Figure 15). (Remember that a kebele is the smallest administrative unit in Ethiopia, covering about 1000 households distributed among several small communities.)
 ©© Basiro DaveyFigure 15 The award given to Fura ‘in acknowledgement of the communities’ dedication in spearheading Hygiene and Sanitation in Ethiopia’Show description|Hide descriptionFigure 15 The award given to Fura ‘in acknowledgement of the communities’ dedication in spearheading Hygiene and Sanitation in Ethiopia’...
©© Basiro DaveyFigure 15 The award given to Fura ‘in acknowledgement of the communities’ dedication in spearheading Hygiene and Sanitation in Ethiopia’Show description|Hide descriptionFigure 15 The award given to Fura ‘in acknowledgement of the communities’ dedication in spearheading Hygiene and Sanitation in Ethiopia’...This is a photo of a plaque awarded to the Fura Communities in December 2008.
However, it is sobering to note that, globally, more than 1.2 billion people still lack basic sanitation and have no alternative but to defaecate in fields and on rubbish heaps and waste ground.
4.3.1 Oral rehydration salts
The importance of community participation in the success of national campaigns to reduce the impact of diarrhoeal diseases is also illustrated by the use of oral rehydration salts (ORS) by parents all over the world to prevent dehydration in children with diarrhoea.
Many low-income countries have established national ‘Control of Diarrhoeal Diseases’ campaigns promoting the use of pre-prepared ORS sachets (over 500 million are distributed free every year), or home-made ‘water with salt and sugar’ rehydration solutions. Bangladesh was the first country to scale up oral rehydration therapy through a national programme to distribute ORS sachets to all affected households. Now many countries give parents the training and confidence as well as the ORS sachets they need to treat diarrhoea in their children (Figure 16).
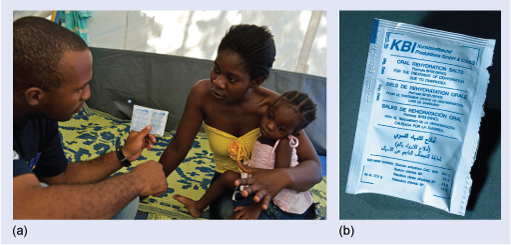
In this photo, the mother has her infant daughter on her knee and the healthworker is talking to her with an ORS sachet in his hand.
However, only one-third of children with diarrhoea in LMICs receive ORS treatment when they need it. This partly explains why diarrhoea is still the second most prevalent worldwide cause of death among young children, killing about 1.4 million every year, most of them under two years of age.
Which infectious disease kills more children under five years than any other? (You may need to look back at Figure 1.)
Pneumonia is the largest killer of young children globally, causing an estimated 1.5 million deaths annually – more than HIV/AIDS, TB and malaria combined in this age group.
In the next section, many of the themes of this course are combined to illustrate the importance of community participation and low-cost interventions to the success of a major public health campaign to eliminate – and ultimately eradicate – guinea worm disease.
5 The guinea worm eradication campaign
Guinea worm disease, or dracunculiasis, is caused by the nematode worm Dracunculus medinensis – literally the ‘little dragon of Medina’. It is the largest tissue parasite to affect humans and the only exclusively waterborne pathogen. Note that the terms ‘guinea worm disease’ and ‘dracunculiasis’ are used interchangeably in the literature on this condition; you will also find ‘Guinea worm’ capitalised in some sources.
The association of the worm with a dragon may be due to the fiery, burning pain experienced at the site where the worm emerges from the body, most often in the lower leg or foot. Like smallpox, it has been known since antiquity and evidence of guinea worms has been found in Egyptian mummies.
The practice of ‘winding’ the emerging worms onto a stick (Figure 17), which has been practised for at least 2000 years, may even have given rise to the symbolic emblem of the medical profession – a staff entwined by two serpents.

The photo shows the three white worms emerging from the top of the foot near the toes. Each worm is wound onto a small narrow stick which is resting on top of the foot.
The campaign to eradicate guinea worms from the world has been chosen as the final example in this course because it illustrates many of the key features of the public health approach to controlling infectious disease – but particularly the importance of community action and the power of low-cost interventions.
5.1 The human cost of guinea worm disease
Dracunculiasis was once endemic in many parts of the world but, by the 1950s, the provision of piped water in towns and cities had eradicated it from North Africa, Egypt, Iraq, Brazil, the West Indies and Uzbekistan. At that time it was confined to rural areas of the Indian subcontinent, Yemen, Iran and parts of Sub-Saharan Africa, but over 50 million people still suffered its effects each year.
Until the 1980s, international health agencies attached a low priority to this ‘forgotten disease of forgotten people’, partly because it is rarely fatal and permanent disability is unusual; infected people generally recover within a few weeks of the worm’s emergence.
However, attitudes gradually changed as a number of research studies evaluated the human cost of a disease with a global burden estimated in 1986 to be affecting at least 3.3 million people. Although the case fatality rate is less than 0.1% (death is usually caused by a secondary tetanus infection) and permanent disability is rare, many microbes can infect the lesion caused where the worm emerges and they can penetrate deep into the tissues along the track of the worm (Figure 18).

The photo shows the white guinea worm track just under the skin on the inside of the ankle; the area around the site where the worm is emerging is red and very inflamed.
Around half of all cases become infected, which greatly increases the disabling effects of the parasite, in terms of both pain in the affected limb, which can reduce mobility for several weeks, and the fever, nausea and debility associated with an acute inflammatory reaction against secondary bacterial infection. More serious complications occur in about 1% of cases and include worms emerging into joints and triggering severe arthritis, or emerging from the breast, genitals, tongue or eye.
How could guinea worm infection have a serious impact on life in rural communities in endemic countries?
An immobilising condition impacts heavily on rural economies where people earn their livelihoods from working on the land. They often walk long distances to reach their fields, herd livestock, collect firewood and drinking water, and – in the case of children – attend school.
The loss of agricultural productivity in affected communities can be seen in terms of ‘stunted’ growth among children whose diet was impoverished as a result of endemic infection. In Mali, the local name for dracunculiasis is ‘the disease of the empty granary’. The economic impact is particularly severe because the highest rates of infection occur in the rural working population (i.e. people aged 15–45).
5.2 Falling trends in guinea worm disease
Recognition of the seriousness of the guinea worm problem led the Indian government to initiate the first national dracunculiasis-elimination programme in 1982.
Similar programmes began later in Pakistan, Cameroon, Ghana and Nigeria, and in 1989 the WHO launched the global eradication campaign. The features of the campaigns will be described shortly but, for the moment, we will concentrate on the evidence of their success. The reduction in transmission of guinea worm disease in the first decade of the global campaign is illustrated by Figure 19.
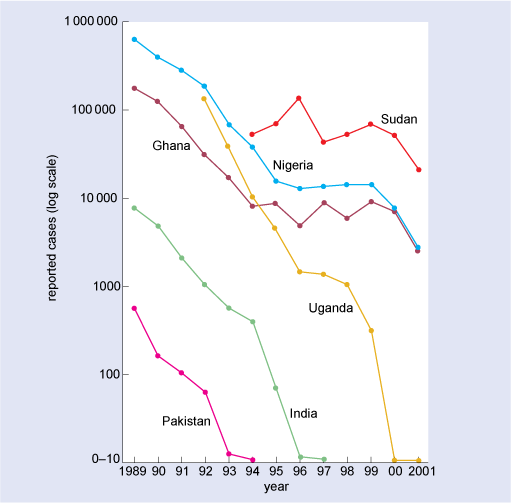
Data are plotted for six countries in which guinea worm disease is endemic: Sudan, Nigeria, Ghana, Uganda, India and Pakistan. The horizontal axis is labelled year and marked from 1989 to 2001 at one-year intervals. The vertical axis is labelled reported case and is marked on a log scale from 0–10 up to 1 000 000. Both Nigeria and Ghana had several hundred thousand reported cases in 1989, and by 2001 case numbers in both countries had fallen to the thousands. Uganda had 100 000 cases in 1992 but by the year 2000, case numbers had dropped to below 10. Both Pakistan and India had relatively small numbers of reported cases in 1989, of the order of 1000 and 10 000 respectively; and in both counties case numbers fell to below 10 in the 1990s: by 1993 in Pakistan, and by 1996 in India. In contrast, numbers of reported cases in Sudan did not decline appreciably over the period of measurement: numbers fluctuated around 100 000 until 1999, and in 2001 were still many tens of thousands.
Eradication in Pakistan was certified by the WHO in 1993, and India followed in 1996. It took several more years before it was eradicated in Uganda (2003), Nigeria (2008) and Ghana (2010) – bringing the total to 187 previously endemic regions and territories certified as free of dracunculiasis by the end of 2010.
In the whole of 2010 there were 1797 reported cases of the disease worldwide, and the number fell to just 1058 cases in the whole of 2011 in only four countries – Chad, Ethiopia, Mali and South Sudan (WHO, 2012j).
The community actions that have interrupted guinea worm transmission so successfully can only be understood by first describing its complex life cycle.
5.3 The guinea worm transmission cycle
Dracunculiasis is the only human disease in which the causative agent is transmitted exclusively in drinking water.
The life cycle of D. medinensis involves a larval maturation stage in an intermediate host – microscopic freshwater crustaceans referred to in the infectious disease literature as ‘cyclops’. (Until recently, all the species that transmit guinea worm larvae were classified in a single genus, Cyclops, which has since been subdivided, but for simplicity the traditional term will be used.) People become infected when they drink water contaminated with cyclops containing infective Dracunculus larvae. The larvae are released in the drinker’s stomach, where the cyclops are killed by the acid environment.
Life cycle
Each cycle occurs over a period of about one year and the main sequence of events can be summarised as follows (see also Figure 20).
- Over a period of about three months, the ingested larvae migrate out of the human host’s gut into the chest cavity, and mature into sexually differentiated male and female worms a few centimetres long.
- There they mate and the male worms die, but the females continue growing for the next 8–12 months, reaching 0.5–1.0 m in length.
- The female worms migrate along muscle fascia towards the surface of the body, usually somewhere in the lower limbs (often on the ankles or feet), where they slowly emerge during a predictable seasonal period lasting two to three months.
- As a female worm nears the surface of the human tissue from which it is about to emerge, it releases a burst of larvae just under the host’s skin. A mature female worm carries over 3 million immature larvae.
- The larvae are strongly immunogenic and provoke a rapid inflammatory response, which erupts in an intensely painful, fluid-filled ulcer, usually somewhere on the lower limbs.
- A natural response to the burning pain of the ulcer is to cool it by standing in cold water – and in rural communities this is most commonly a village pond, or a shallow ‘step well’ where people step down into the water to fill drinking pots.
- The sudden cooling stimulates the worm to emerge by a few millimetres and release several thousand immature larvae into the water.
- Over the next six weeks, the worm emerges slowly from the host’s skin, releasing another shower of larvae every time it is exposed to cool water.
- The worm larvae are free swimming and can survive for several days in still ponds and shallow wells, which are also ideal habitats for cyclops.
- The immature larvae are eaten by cyclops, initiating another cycle of infection.
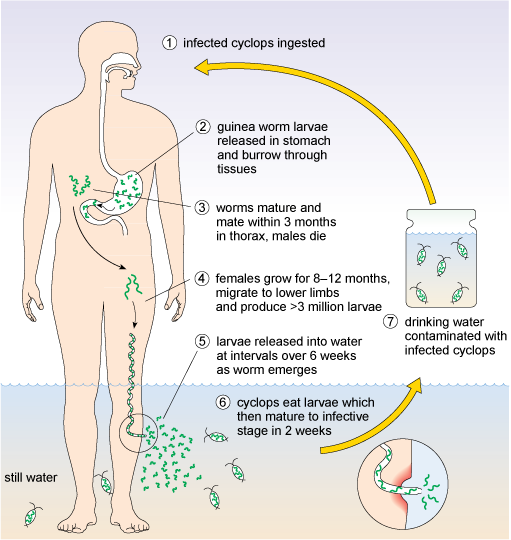
The diagram shows the transmission cycle as a series of seven numbered stages, beginning, in stage 1, with ingestion of the infected cyclops by drinking contaminated water. In stage 2, guinea worm larvae are released in the stomach and then burrow through the tissues. In stage 3, the worms matures and mates within 3 months in the host’s thorax; then the males die. In stage 4, the females grow for 8–12 months and migrate to the lower limbs where they produce more than 3 million larvae. In stage 5, the larvae are released from the female worm into still water (e.g. a lake) at intervals over a period of 6 weeks as the worm is emerging from the limb to the exterior. In stage 6, cyclops present in the water eat the larvae, which mature inside them, reaching the infective stage in 2 weeks. Finally, in stage 7, drinking water contaminated with the infected cyclops is taken from the lake.
Treatment and control
None of the drugs used in the treatment of other parasitic worms has any therapeutic effect against guinea worms. At best, antibiotics or antibacterial ointment rubbed into the worm eruption site may reduce the risk of secondary bacterial infections.
No vaccine has yet been developed to protect people who ingest the larvae, and infected people do not develop a protective immune response to the adult worms, so they can be infected again and again.
Thus, attempts to control dracunculiasis have had to rely entirely on community action and low-cost interventions rather than on medical treatment.
5.4 Eradication through community action
Several features of dracunculiasis suggested that a global eradication campaign would be feasible, despite the lack of drugs to kill the worms in the body or a protective vaccine (Box 4). Note the similarity between the first two features and the factors contributing to the global eradication of smallpox – a viral disease with a totally different transmission pattern (see Box 3).
Box 4 Reasons why the global eradication of dracunculiasis is feasible
- Although Dracunculus species are known to infect reptiles and large mammals in areas where guinea worm disease is endemic in humans, there is no evidence that these animals have ever acted as a reservoir for parasites in the human population.
- No other human parasite behaves like D. medinensis, so there is no ambiguity about the diagnosis at the point where the worm erupts from the skin. This makes case finding and case containment relatively straightforward.
- The period in which an infected person poses a risk to others is relatively short (about six weeks while the worm emerges) and the worm larvae are shed seasonally, over a predictable period of 2–3 months, so interventions can be focused intensively at certain times of the year.
- The intermediate host (cyclops) is restricted to still water in shallow pools and step wells, so it cannot easily extend its range (in contrast to an insect vector).
- Transmission to humans is exclusively in drinking water, so if local water sources are protected from contamination by worm larvae, the infection cycle will be broken.
5.4.1 Protection of water sources
The features listed in Box 4 underlie the strategies that have succeeded in eradicating guinea worms from most countries and greatly reducing their incidence in the few remaining endemic areas. The eradication campaign illustrates several features of the public health approach to the control of infectious diseases, particularly in remote regions with high levels of poverty and low literacy rates. It has relied primarily on three simple, low-technology strategies, operated within the affected communities by local people: the protection of drinking-water sources from reinfection; the routine filtering of water at the point of use; and the case containment of infected people.
Protection of drinking water sources from reinfection
Drinking water sources can be protected from reinfection by persuading people with emerging worms not to enter the water until the lesion has healed. In some countries, ‘pond caretakers’ (usually elderly men) are paid a small fee to guard local ponds and step wells during the season of worm emergence.
Routine filtering of water at the point of use
A second important control measure is the routine filtering of water at the point of use, just before drinking it, to remove the infected cyclops. This initiative has been supported by the donation of hundreds of thousands of square metres of fine mesh nylon cloth.
- Squares of cloth are placed over the neck of containers when water is poured for drinking; it is long lasting and easily washed, which has helped greatly in popularising the use of these simple filters.
- Short pieces of small diameter plastic pipe with one end covered in fine cloth are also supplied as drinking straws. A string attached at the open end enables the straw to be hung around the neck, so workers can take it with them to the fields to use when they drink from shallow pools during the day.
Case containment
Case containment has also been practised in the later stages of a campaign (it is too labour intensive to be used on a large scale). It involves the controlled release of worm larvae by plunging the affected limb into a bucket of cold water, followed by simple palliative treatment (e.g. painkillers, antibiotic ointment), and bandaging of the worm-emergence site. The infected person agrees not to remove the bandage or enter sources of drinking water, and the procedure is repeated every few days until the worm has completely emerged.
5.4.2 Community participation in the eradication programme
The important health education messages have largely been delivered by one or two volunteers from each village. They are each given basic training and provided with a few educational aids, e.g. posters, leaflets and slogans on T-shirts (Figure 21), to raise awareness and promote understanding of how the guinea worm larvae are transmitted and how to prevent the transmission of infection.
Community participation in the eradication programme is central to its success – without it, no progress would have been made. It demonstrates that combined community action can persuade individuals to change behaviour that damages their health. The success of this low-cost approach has been striking, not only in reducing the number of cases to the threshold of eradication, but also in empowering local people and reducing poverty and the loss of education due to the disabling effects of guinea worm disease.
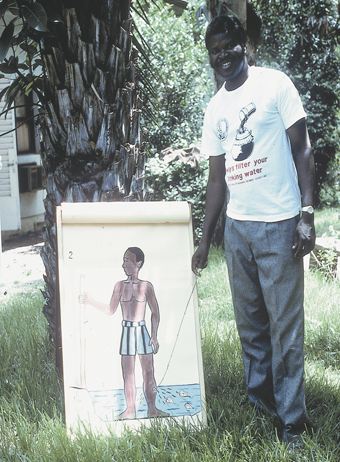
In this photo, Dr Bugri is beside the flip chart which shows a picture of a boy standing bare-legged in water that is nearly up to his knees. Dr Bugri is using a pointer to draw attention to the larvae emerging into the water from the boy’s lower leg. Dr Bugri is wearing a T-shirt on which is written: Always filter your drinking water. Above the message is printed a drawing of a simple water filter.
5.4.3 Surveillance and case mapping
Surveillance and case mapping have also played a huge part in reducing guinea worm disease to such a low incidence and they are crucial to the ‘final push’ to eradicate it worldwide. The main steps are as follows.
- The community health workers in endemic countries report cases to their national registry, which collates all the data and then reports to the WHO.
- Cases are mapped accurately using GPS location finding to ensure that contaminated water sources are identified and local people are alerted to the risks.
- This technology has enabled data to be combined on a visual display, which maps the exact locations of at-risk populations, natural water sources, relevant infrastructures (e.g. wells, boreholes, health clinics, schools), and the number of trained health workers committed to guinea worm eradication projects.
- The maps allow the swift identification of places where resources need to be targeted more effectively, and where cases are being imported from neighbouring areas.
The dracunculiasis maps have also proved to be highly effective advocacy tools, both for informing governments of the progress of the campaign and for persuading commercial donors and aid agencies to support it.
Subsequently, the public health mapping project has been extended to support other eradication and disease control programmes, including the Polio Eradication Campaign and ‘Roll Back Malaria’. In 2003, the system was extended to HIV and other sexually transmitted infections, tuberculosis, and complex emergencies involving infectious diseases such as SARS.
5.4.4 Other interventions to support guinea worm eradication
Of course, the most effective way to eradicate guinea worms would be to provide safe drinking water, which would also reduce the risk of many other important infectious diseases that are also endemic in the same geographical areas. Attempts have been made to achieve this aim using both mechanical and chemical means, although both strategies have drawbacks.
Installation of hand-pumps
In the early years of the global eradication campaign, considerable emphasis was placed on improving water quality by drilling boreholes and installing a hand-pump in villages in endemic areas. However, the cost (about US$10 000 each) was unsustainable from government funds, even with aid donations. Also, the pumps need regular maintenance and many have fallen into disuse.
Temephos, a water-treatment chemical
In the 1990s, some additional help in the final stages of an elimination campaign came from the donation of a water-treatment chemical (temephos). This can be added safely to drinking water to kill infected cyclops, provided the volume of water can be accurately measured. At the correct concentration, temephos is harmless to fish and humans, but its application is labour intensive and accurate dosing is a major problem.
Figure 22 illustrates the difficulty of dosing a natural pond effectively, when the water volume can change rapidly with the seasons and the chemical treatment must be repeated at least once a month.

In this photo, temephos solution is being poured from a bucket into the pond. Here the level of water is low; a higher water level would require a higher dosage in order to eliminate the infected cyclops.
5.4.5 A final thought about dracunculiasis eradication
To conclude Section 5, you should consider the following ethical problem that may indeed have already occurred to you.
As the deliberately targeted extinction of D. medinensis approaches, there are concerns about the inadequate biological characterisation of a species that will soon be extinct. Very few female worms have been collected in a suitable condition for research and no males have ever been recovered from humans. The fourth meeting of the International Commission for the Certification of Dracunculiasis Eradication (WHO, 2000) recommended that strenuous efforts be made to collect intact specimens and send them to European laboratories for genome sequence analysis and the preservation of a D. medinensis gene library before it is too late.
6 The Millennium Development Goals, infectious disease and public health
While there have been enormous strides in improving public health in all countries worldwide during the twentieth century, through the approaches described and illustrated in this course, there is still a huge gap between the health of the poorest people and the rest.
In this century, public health approaches, including slum clearance, are central to achieving the Millennium Development Goals (MDGs) adopted by the United Nations at its Millennium Summit in 2000 (Box 5).
Box 5 United Nations Millennium Declaration
The United Nations’ 2000 Millennium Development Goals resolution on development and poverty eradication is summarised as follows.
Resolved, by the year 2015: to halve the proportion of the world’s people whose income is less than one dollar a day and the proportion of people who suffer from hunger; to halve the proportion of people who are unable to reach or to afford safe drinking water; to ensure that children everywhere, boys and girls alike, will be able to complete a full course of primary schooling and that girls and boys will have equal access to all levels of education; to reduce maternal mortality by three quarters, and under-five child mortality by two thirds, of their current rates; to have halted and begun to reverse the spread of HIV/AIDS, the scourge of malaria and other major diseases that afflict humanity; to provide special assistance to children orphaned by HIV/AIDS.
Resolved, by 2020: to have achieved a significant improvement in the lives of at least 100 million slum dwellers.
Note that the MDGs summarised in Box 5 cannot be separated into those that relate to infectious disease and those that do not. People who live in poverty in urban slums and shanty towns cannot protect themselves from sources of infection; children who are frequently ill cannot complete their schooling.
6.1 The persistent effects of poverty on health
The World Bank (2009) estimated that there were 1.4 billion people in 2008 with an income of less than US$1.25 per day. In 2010, this estimate was confirmed as still the most accurate measure of the number considered to be living in absolute poverty. Aside from the obvious threats to health that poverty entails, the lack of the means of subsistence drives impoverished rural populations into already overcrowded cities. The movement of rural populations into urban slums (Figure 23) is increasing faster than the ability of most LMICs to provide adequate housing, sanitation, drinking water, education and health services.

However, the outlook is not without hope: the advances in infrastructure, communication and organisation at local, national and international levels that delivered such large improvements in public health in the ‘developed’ world in the twentieth century are being applied now in LMICs with substantial success – as several of the examples in this course have demonstrated.
6.2 Other challenges to achieving the MDGs for public health
Despite the undoubted progress of recent decades, the prospects for meeting the MDG targets in relation to infectious disease and public health are constrained by many factors in addition to poverty. They include:
- the biological adaptability of many of the most important pathogens infecting humans, which enables the rapid evolution of resistance to chemical controls
- the lack of finance in heavily indebted countries for installing sanitation and piped water, or providing vaccination programmes, soap, mosquito nets and other preventive strategies
- the shortage of essential skills, scientific and technological knowledge, trained personnel and equipment
- difficult circumstances of geology and climate and the risks posed by major natural disasters – drought, flooding, earthquakes, etc.
- the level of illiteracy and gender inequality in a population, which can limit the effectiveness of health education initiatives
- the extent to which political will, social stability and community action can be harnessed for the public good; individuals and communities may be highly resistant to behavioural change; cultural practices and attitudes may oppose interventions such as vaccination.
Conclusion
- Public health strategies aim to prevent disease or reduce its impact by taking actions to protect or promote the health and wellbeing of the population as a whole, in contrast to medical strategies for treating disease in its individual members.
- The global burden of infectious disease remains a significant threat to health, economic development and equity of opportunity, particularly (but not exclusively) in low- and middle-income countries and disproportionately among young children.
- A systematic and evidence-based approach to addressing threats to public health began with the sanitarian movement in England in the nineteenth century and remains the basis for public health strategies today.
- Public health approaches to infectious diseases focus on one or a combination of:
- screening, surveillance, monitoring and reporting of disease outbreaks
- community education to promote health-related behaviour change
- increasing the resistance of the human host to infection, e.g. through vaccination and nutritional support
- community mobilisation to tackle sources of infection in the environment
- case finding, case containment and (where necessary) isolation of infectious individuals.
Vaccination, the provision of clean drinking water and improved sanitation, the promotion of personal and institutional hygiene (particularly the importance of handwashing with soap), and the organisation of surveillance and response strategies to detect and control disease outbreaks are integral to the public health approach. Raising sustainable living standards, improving the quality of housing, nutrition and education, and promoting gender equality and personal security are also important public health goals.
- International health regulations (IHRs), including trade and travel agreements, and the work of international organisations (e.g. the WHO) contribute at a global level to public health approaches to infectious disease.
- Three levels of prevention of infectious diseases can be identified in a public health context. Primary prevention aims to prevent new cases from occurring; secondary prevention aims to treat the disease at the earliest stage to prevent it from spreading; and tertiary prevention aims to alleviate the worst effects of an established disease in an individual, which may indirectly benefit the rest of the community.
Community participation and community health workers with minimal training and equipment are central to the success of infection-control campaigns in many parts of the world, and particularly in low- and middle-income countries.
The importance of community action is illustrated by the success of the rural Health Extension Programme in Ethiopia (Video 1), the reduction in healthcare-associated infections (HCAIs) in the UK, and the worldwide eradication campaigns against smallpox, polio and guinea worm disease.
Despite the undoubted progress of recent decades, the prospects for meeting international targets in relation to infectious disease and public health are constrained by many factors. In addition to poverty, poor housing and food insecurity, they include:
- the biological adaptability of infectious agents, which enables the rapid evolution of new more virulent strains and resistance to chemical controls
- the lack of finance for basic infrastructure to provide sanitation and piped water, vaccination, soap, bed-nets and other preventive measures
- the shortage of essential skills, scientific and technological knowledge, trained personnel and equipment
- difficult circumstances of geology and climate and the risks posed by major natural disasters – drought, flooding, earthquakes, etc.
- the level of illiteracy and gender inequality in a population, which can limit the effectiveness of health education initiatives
- the extent to which political will, social stability and community action can be harnessed to promote health and overcome resistance to behavioural change.
However, there are hopeful signs: the advances that delivered such large improvements in public health in high-income countries in the twentieth century are being applied in low- and middle-income countries with substantial success, as several of the examples in this course have demonstrated.
Questions for the course
The following questions allow you to assess your understanding of the content of this course. Each one relates to one or more of the intended learning outcomes of the study.
If you are unable to answer a question, or do not understand the answer given, then reread the relevant section(s) of the course and try the question again.
Question 1
(This question relates to course learning outcomes (LOs) 1–4.)
Suggest at least one example of a public health measure that can be taken to control malaria at each of the primary, secondary and tertiary levels of prevention.
Answer
Primary prevention strategies against malaria include:
- chemoprophylaxis – taking drugs to protect against infection with malaria parasites before going into an endemic area, or at high-risk periods (e.g. during pregnancy)
- keeping skin covered, particularly from dusk to dawn
- use of insect-repellent chemicals on exposed skin
- routine use of insecticide-treated nets (ITNs) when sleeping
- spraying houses with insecticides against adult and larval mosquitoes
- use of curtains across doors and windows
- environmental engineering to prevent or destroy mosquito breeding sites
- putting surfactant on the surface of pools used by mosquitoes for breeding
- keeping water tanks covered.
Secondary prevention includes:
- providing education about the early signs of malaria and the need to seek treatment as soon as possible
- surveillance, screening and case finding of infected individuals in communities in endemic regions (e.g. by blood testing)
- administration of drugs to treat early cases of malaria.
Tertiary prevention refers to treatment of the life-threatening complications of malaria (e.g. cerebral malaria), usually with intravenously administered drugs and fluids.
Question 2
(This question relates to course LOs 1–5 and the DOTS programme (directly observed treatment, short course: see Section 3.4) for the treatment of tuberculosis (TB). )
- a.In what ways does the DOTS programme illustrate the importance of community action in the prevention and control of tuberculosis?
- b.What is the main limitation of the DOTS approach as a strategy for preventing the transmission of TB?
Answer
- a.Even though the prime purpose of the DOTS programme is to ensure compliance with the drug regimen, it also supports individuals within their communities and involves many agencies (including community volunteers) in its delivery.
- b.The main limitation of the DOTS approach in terms of TB prevention is that it cannot tackle the socio-economic conditions (e.g. poverty, lack of housing, poor nutrition) that increase the spread of TB.
Question 3
(This question relates to course LOs 1, 3 and 5.)
Identify two similarities in the strategies used to control the spread of diarrhoeal diseases in the rural Health Extension Programme in Ethiopia (see Video 1) and C. difficile infection in English hospitals.
Answer
You might have thought first of the common approach to increasing awareness of hand hygiene in both locations. The Ethiopian programme has promoted the installation of yellow plastic canisters of clean water near latrines to facilitate hand washing (ideally with soap); this is similar to the programme in English hospitals to install alcohol-based hand-hygiene stations in all wards and corridors.
Secondly, both of these initiatives require community mobilisation and the full participation of staff, patients and community members in order to reduce the incidence of infectious agents transmitted on the hands.
Question 4
(This question relates to course LOs 1 and 6.)
Explain why the type of water source available is a key factor in determining the areas where guinea worms are endemic and the areas where they have spontaneously disappeared.
Answer
Even in endemic countries, dracunculiasis does not occur in urban areas where piped water is supplied, and it is rare in rural communities where the principal sources of drinking water are fast-running streams or deep wells, because the intermediate host (cyclops) cannot survive in these environments. It inhabits still, shallow water, such as natural pools and step wells, where people are most likely to stand as they draw water, or seek relief from the burning pain of a guinea worm as it emerges.
Glossary
- acute respiratory infections (ARIs)
- Bacterial or viral infections of the respiratory tract, including pneumonia and influenza, lasting less than 14 days. ARIs cause a larger total number of deaths than TB, HIV/AIDS and malaria combined, with the highest mortality among children under five years of age.
- Care Quality Commission (CQC)
- Independent regulatory authority inspecting all health and social care services in England to ensure they meet set quality standards.
- case containment
- A public health approach to infectious disease outbreaks, in which infected people (cases) are prevented from transmitting the pathogen, e.g. they may be ‘contained’ at home or in a special healthcare course. In extreme cases (e.g. smallpox, dengue fever) infected communities may be sealed off until all patients recover or die, all known or suspected contacts have been vaccinated (if a vaccine exists), or the disease incidence has fallen to zero.
- Clostridium difficile infection (CDI)
- Symptomatic infection with Clostridium difficile bacteria. CDI occurs mainly in hospitals and nursing homes in people over 65 years after treatment with broad-spectrum antibiotics, which destroy commensal gut bacteria, allowing C. difficile to proliferate in the large intestine. CDI causes severe ulceration of the gut lining, pain and persistent diarrhoea.
- combined (or combination) vaccines
- Vaccines containing the antigens of more than one type of pathogen, so immunisation protects against more than one infectious disease (e.g. the MMR vaccine against measles, mumps and rubella).
- dracunculiasis
- See guinea worm disease.
- DTP3 coverage
- The percentage of infants (i.e. in the first year of life) vaccinated with three spaced injections of a combined vaccine to protect them from diphtheria, tetanus and pertussis. This percentage is taken as one measure of the effectiveness of routine vaccination campaigns, particularly in low- and middle-income countries. NB: some sources refer to ‘DPT3’ (the terms are interchangeable).
- eradication
- Reduction of the number of infections to zero, with no known source of reinfection. Eradication of specific infectious diseases is confirmed by the World Health Organization (WHO) initially for a country, then for all countries in a WHO Region, and ultimately (as in the case of smallpox) for the whole world.
- Global Outbreak Alert and Response Network
- The main coordinating body of the World Health Organization’s infectious disease surveillance and response system. See also International Health Regulations (IHRs).
- guinea worm disease
- A disease caused by a nematode worm, Dracunculus medinensis, the largest tissue parasite to affect humans and the only exclusively waterborne pathogen. The worm larvae are ingested by aquatic Cyclops, consumed by humans in drinking water and, after a complex maturation cycle, emerge as adult worms usually from the person’s lower leg, causing pain and inflammation. (Also known as ‘dracunculiasis’.)
- healthcare-associated infections (HCAIs)
- Infections that develop as a direct result of medical or surgical treatment or contact in a healthcare setting, such as a hospital, residential care home or nursing home.
- health-related behaviour modification
- Long-lasting changes in behaviour that result in health gains, reduction in health risks or an increase in disease prevention.
- herd immunity level
- The herd immunity level is reached in a population when the ratio of immune (vaccinated or recovered) individuals to non-immune (susceptible) individuals is high enough to stop the infection circulating in the population; the pathogen ceases to circulate because there are too few susceptible individuals to sustain its numbers.
- hygiene behaviour
- The wide range of actions taken by individuals to maintain a standard of cleanliness of their bodies, domestic environments and workplaces, which prevents or reduces the risk of transmitting infectious agents to others.
- incidence
- The number of new cases of a disease arising in a given period, usually a year, expressed as a proportion of the population at risk (the incidence rate).
- International Health Regulations (IHRs)
- The IHRs (updated in 2005) aim to ensure early warning and prompt action to contain any public health emergency of international concern. The obligations on member states include national disease prevention, surveillance, control and response systems, public health security in travel and transport, particularly at designated airports, sea ports and ground crossings, and ‘real time’ reporting of disease outbreaks to WHO via round-the-clock communication channels.
- methicillin-resistant Staphylococcus aureus (MRSA)
- Strains of Staphylococcus aureus bacteria that resist treatment with methicillin (or meticillin in the UK), the antibiotic generally used to treat staphylococcal infections. MRSA commonly causes infection of surgical sites and the bloodstream. VRSA strains have also been identified that are resistant to another antibiotic, vancomycin.
- Millennium Development Goals (MDGs)
- The United Nations (UN) Millennium Development Goals were adopted by world leaders at a UN summit meeting in September 2000. The initiative includes the following targets, to be achieved by 2015: halving extreme poverty and hunger; providing productive employment and access to primary education for all; eliminating gender disparity in education; reducing the under-five mortality rate by two-thirds and the maternal mortality rate by three-quarters; achieving universal access to reproductive health; halting the spread of HIV/AIDS, malaria and tuberculosis and providing universal access to prevention and treatment; ensuring environmental sustainability and reducing biodiversity loss; halving the proportion of people without access to improved water and sanitation; achieving significant improvement in the lives of at least 100 million slum dwellers; and developing global partnerships for development, debt reduction, access to affordable drugs and the benefits of new technologies. (Source: United Nations (UN) (2010) ‘Millennium Development Goals (MDGs)’ [online], http://www.un.org/ millenniumgoals/ (accessed 22 October 2012).)
- prevalence
- The proportion of the population with a particular infection or disease at a particular point in time, or during a given period.
- primary prevention
- Public health strategies that seek to prevent new cases of infection from occurring, e.g. vaccination, promotion of personal hygiene, food safety legislation, installation of infrastructures that reduce infection risks, such as sewerage and piped water supplies.
- quarantine
- A period of enforced isolation, or restriction of travel or activity, in order to prevent the spread of an infectious disease.
- reference laboratories
- Designated laboratories in countries around the world that collect and analyse infectious agents (e.g. influenza viruses) sent by detection centres to give early warning of new variants that could pose a major risk to global health.
- screening programmes
- The systematic application of a test or investigation to large numbers of individuals to identify those at risk of developing a particular disease, or (in the case of infectious disease) those who are already infected.
- secondary prevention
- Public health strategies that aim to detect new cases of infectious disease at the earliest possible stage and intervene in ways that prevent or reduce the risk of infection from spreading further in the population.
- tertiary prevention
- Medical treatment to prevent the worst outcomes of a disease in an individual.
References
Acknowledgements
This course was written by Dr Basiro Davey MBE.
Except for third party materials and otherwise stated (see terms and conditions), this content is made available under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 Licence.
The material acknowledged below is Proprietary and used under licence (not subject to Creative Commons Licence). Grateful acknowledgement is made to the following sources for permission to reproduce material in this course:
Course image: Dave Bloggs in Flickr made available under Creative Commons Attribution 2.0 Licence.
Figure 1: data from United Nations, 2011, The Millennium Development Goals Report: Addendum on Goal 4 ‘Reduce child mortality’
Figures 2, and 12: © Basiro Davey
Figures 3 and 9: © WHO/P.Virot
Figures 4a, 5 and 7: © WHO/TDR/Crump
Figure 4b: © WHO
Figure 6: © WHO/TDR/Martel
Figure 8: © CDC/James Hicks
Figure 10: Andy Crump, TDR, WHO/Science Photo Library
Figure 11: © HDPTCAR http://www.hdptcar.net/
Figure 13: photograph © Basiro Bavey
Figure 14a: data from: ‘Summary Points on Meticillin Resistant Staphylococcus aureus (MRSA) Bacteraemia’, Health Protection Agnecy
Figure 14b: based on data from these Heath Protection Agency document: Summary Points on Clostridium difficile Infection (CDI)
Figure 16a: © UNICEF/NYHQ2010-0184/Noorani
Figure 16b: courtesy of Echo International Health Services Ltd.
Figure 17: courtesy Dr. A. Tayeh
Figures 18, 21 and 22: courtesy of Ralph Muller
Figure 19: Cairncross, S. et al. ‘Dracunculiasis (Guinea Worm Disease) and the eradication initiative’, Clinical Microbiology Reviews, April 2002, American Society for Microbiology
Figure 23: © Justin DeNormandie and Janette Sunita, population Services International (PSI) Delhi, India/WHO.
Video 1: all photos courtesy of Basiro Davey/Open University, unless otherwise stated in the video.
Every effort has been made to contact copyright holders. If any have been inadvertently overlooked the publishers will be pleased to make the necessary arrangements at the first opportunity.
Don't miss out:
If reading this text has inspired you to learn more, you may be interested in joining the millions of people who discover our free learning resources and qualifications by visiting The Open University - www.open.edu/ openlearn/ free-courses
Copyright © 2016 The Open University