Death and medicine: Postponement and promise
Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Friday, 26 April 2024, 8:08 AM
Death and medicine: Postponement and promise
Introduction
This course helps you to explore the extent to which death and dying in western societies are medical events and what aspects of death and dying might be neglected as a consequence. The course covers the ways in which medical care provides the context of the experiences associated with the end of life.
This OpenLearn course provides a sample of level 2 study in Health & Social Care. If you find this course interesting, take a look at the Open University course K220 Death, Dying and Bereavement. Alternatively, you can explore the related OpenLearn course, An introduction to death, dying and grief.
Learning outcomes
After completing this course, you should be able to:
evaluate end-of-life care approaches in the UK and challenges to care delivery
evaluate the usefulness of theoretical models of death, dying and bereavement
recognise the relevance of critical social perspectives associated with death, dying and bereavement
critically reflect on policy and practice in order to promote the interests of dying and bereaved people.
1 Expectations and administrative pressures
The medical prognoses and diagnoses of dying raise expectations of what will actually happen to the dying person. For example, someone is diagnosed with terminal lung cancer, they may be given a forecast that covers the estimated length of time before death, any likely symptoms, the development of the illness, and possible treatment(s). Of course, these types of medical expectations are not unique to death and dying: they are found in all treatments of illness, and no doubt you will have had similar experiences of having an illness diagnosed by a GP and being told what to expect.

This is a photograph of a woman talking to a GP.
In dying, however, prognoses such as these are problematic because of the levels of certainty they assume and how they affect professionals’ behaviour towards the dying person. Glaser and Strauss, in their study of dying patterns, point this out in considering how nurses behave around patients:
Nurses’ definitions of the patient’s illness status – that is, their expectations – affect their behaviour towards him. Therefore, the moment when their expectations change is significant. For example, even when the physician’s cues imply that the patient is doomed, as when he stops blood transfusions, the nurses may still not be absolutely sure that the implied prediction is accurate. They may not lower their levels of alertness or reduce their effort to save the patient.
This resonated with one person, who commented on how this echoed her own past experience of expectation and prognosis, which had not been a particularly positive one:
As my grandfather lay in a hospital bed for six weeks, at some point (I cannot recall when) a ‘Do not resuscitate’ card appeared at the foot of his bed. This card, which came out of the blue and had not been discussed with my family, signalled to me and everyone else on the ward that my grandfather had been identified by the medical personnel as someone who they were not willing to ‘work on’ anymore. From that moment on it appeared that the clinical staff's behaviour around my grandfather changed, as if he was doomed in some way.
Although a ‘do not resuscitate’ form – also known as a DNACPR for do not attempt cardiopulmonary resuscitation – does not mean there has been a decision to stop other treatments or care, it can be symbolically interpreted as such, both by patients and their families or by professionals. Because of this, clinicians in the UK are encouraged to think about ‘treatment escalation plans’ that indicate a range of treatment decisions and encourage those caring for the patient to continue routine care as appropriate.
The sociologist, Kellehear (2007) points out that dying does not take place in a social and physical vacuum. For example, it has implications for the way in which medicalised dying is managed. When dying takes place in a public, (relatively) open and visible space such as a hospital, or a section of a hospital such as the intensive care setting, an individual’s experience becomes a communal issue and a public administrative matter. For example, there may be enormous pressure on beds in a ward where someone is dying – the pressure for the administrators of the hospital is to have a high turnover of patients to ensure that targets for treatment are met. One result of this is that people who exceed the medical expectations of their prognoses become problematic. The following example is taken from the system of health care in the USA; nonetheless, it provides a vivid illustration of the tension between medical predictability, administrative efficiency and providing appropriate and suitable end-of-life care.
A patient expected to die on time, but who suddenly begins to recover slightly or to linger – the short-term reprieve pattern – can cause problems for nurses, family, physicians, and hospital administrators. Here is an example: one patient who was expected to die within four hours had no money, but needed a special machine during his last days. A private hospital, at which he had been a frequent paying patient for thirty years, agreed to receive him as a charity patient. He did not die immediately but started to linger indefinitely, even to the point where there was some hope he might live. The money problem, however, created much concern among both his family members and the hospital administrators. Paradoxically, the doctor had continually to reassure both parties that this patient, who actually lasted six weeks, would soon die; that is, to try to change their expectations back to ‘certain to die on time’.
This can have repercussions on several practical levels. When death is so unpredictable and there is a high premium on being with someone at the end of life, such tensions can cause distress. This is no different for those who are medically diagnosed as dying, as you can see from Glaser and Strauss’s example. Someone who ‘lingers’ – itself a problematic term as it implies that the lingering person is a nuisance – creates difficulties for the family, who are also left in an indeterminate state. In this example, the authors did not elaborate on what the family did, but one can imagine the difficulty in negotiating compassionate leave from work over a period of six weeks. A team member recounted how when her father was dying (he was given a six-month prognosis but lived for 14 months) she had been saving her leave to help to care for him in the last few weeks of his life, but ended up losing her leave because she had not been able to carry any forward to the next year, leaving her exhausted. The medicalisation of the dying process, therefore, cannot be assessed and examined separately from the practical and policy context within which it takes place.
2 Terminology: patients or people?
In this course ‘the patient’ has been referred to on several occasions. One reason is the universal usage of the term and the ease with which it is understood. To identify someone as a patient immediately situates them as someone in receipt of medical treatment. However, the term itself is not without difficulty, as sociologists critical of medicine have been quick to point out, since it carries associations of power and authority.
Labelling theory is a useful concept that assesses how an individual acts and behaves once they have been identified or categorised by society. It is a popular concept in criminology, particularly in studying how people become repeat offenders once they have been labelled ‘a criminal’. This principal of labelling can apply to what happens when a person is identified as ‘a patient’.
The connotations of being medically defined and labelled as a patient are especially potentially harmful when a person is dying, as it suggests that the dying person is the passive partner in the patient–practitioner relationship and therefore dependent on clinicians.
The hospice movement has tried to distance itself from the unequal doctor–patient relationship, focusing instead on autonomous patient-centred care and services. In this alternative model of health care delivery, the dying person is actively encouraged to be the primary decision maker. However, the extent to which dying people can unilaterally decide on such things as length of stay is limited.
3 Problems with quantification
One of the main problems with the medicalisation of death and dying is the idea that science has all the answers. Illness and dying carry the same degree of unpredictability and uncertainty as all everyday life events. So when service providers draw on medical knowledge and experience to offer some certainty and in one way to quantify the dying experience, it can be difficult to challenge. Indeed, there is a tension between wanting certainty and hoping for things to be different. Campaigner and mother of three Jane Tomlinson was diagnosed with terminal cancer in 2000 and told she had approximately 12 months to live. However, over the next seven years she completed various marathons and long-distance runs, undertook triathlons and cycled across the USA, until her death in September 2007. Astounding the medical professionals who had delivered the terminal diagnosis, her individual achievements stand as a well-known example of the unpredictability of medical prognosis and the dying period. Another example comes from our researchers’ experience of conducting research on end-of-life care, where only 10% of the people in a study died within the year of the study, despite all being identified as likely to be in their last year of life (Borgstrom, 2014).

This is a photograph of Jane Tomlinson
In addition, human beings are not machines that respond in predictable, impartial ways to their situation and environment(s), so what of the unquantifiable elements of being human? In particular, what account is taken of the emotional component and how it plays a significant part in the experience of health, illness and dying? When someone is dying, the relationship between the health care professional(s) and the dying person is extremely important, in terms of not only the control of bodily death, but also emotional responses. This is especially the case if the dying person is in a public setting such as a hospital, where extreme emotional displays could be distressing for other patients, visitors and staff. The control of emotion by professionals as part of their role is sometimes called emotional labour, a term first used by Arlie Hochschild (1983) in her study of the way airline crews had to present a pleasant manner to their customers no matter how they felt.
Furthermore, when undertaking emotional labour, not only do professionals need to control their own emotional reactions, they also have to manage other people's, which Hochschild called emotion work. Emotion work has been criticised in professional contexts for controlling the customer/patient/client's visible response to their experience. In the context of this course, the emotion work that is undertaken by medical professionals is an example of the application of medical authority in dying. In the most extreme cases, dying people can be sedated to quieten, even to silence, their strong emotional reactions to dying, such as those described by the sociologist Julia Lawton (2000) in her ethnography of death in a hospice. This upholds one view that death should be a peaceful and controlled event, reminiscent of the concept of the good and ‘tamed’ death.
Taking a more policy-orientated view of quantifying the dying process, however, boundaries for treatment need to be drawn somewhere to ensure that there is equality and efficiency in access to and provision of health care services. When this course was first written in 2008, the problem of limits and cut-off points for treatment has been most commonly seen in discussions about access to drugs, such as the National Institute for Health and Clinical Excellence (2007) guidelines on access to donepezil, galantamine, rivastigmine and memantine for people suffering from moderate Alzheimer's disease. When this course was updated in 2020 during the COVID-19 pandemic, there were public discussions around how clinicians decide who can and will be admitted to intensive care units and a wide-scale engagement to sign DNACPRs. These reflect the medicalised tension of balancing the needs of the individual against the fair distribution of resources to the collective dying community.
This dilemma of the individual versus the collective is reflected in the UK in health institutions, such as hospitals, that have to be overtly accountable to the electorate. Hospices, although usually funded through a combination of the state and charity, also have to be able to provide a fair and equal service to all. This is the case from the ideological basis of the health care setting through to the everyday activity on the ward. When someone is dying, therefore, it can be an extremely challenging act of negotiation between the dying person, the medical professionals, the administrative staff of the facility and the family. Medical intervention can take control away from the dying person and control their dying.
4 Power: the medical gaze and the management of risk
Power is an essential feature of the debate about the medicalisation of death, as western societies value knowledge and expertise and allocate authority accordingly. As highly trained professionals, medical and clinical practitioners fall into some of the most highly esteemed positions of authority in society. The philosopher, Foucault highlights the relationship between power and knowledge. He connects them to the extent that:
[P]ower and knowledge directly imply one another; … there is no power relation without the correlative constitution of a field of knowledge, nor any knowledge that does not presuppose and constitute at the same time power relations.
In claiming that in modern societies power is knowledge, Foucault argues that there are more subtle forms of control than coercion and force. For him, power is everywhere and no one can be outside its influence. Power, according to his theorising, is not possessed but instead is something that can be understood as relational. He sees this relational feature as embedded in social organisations, expressed through hierarchies and determined through discourses.
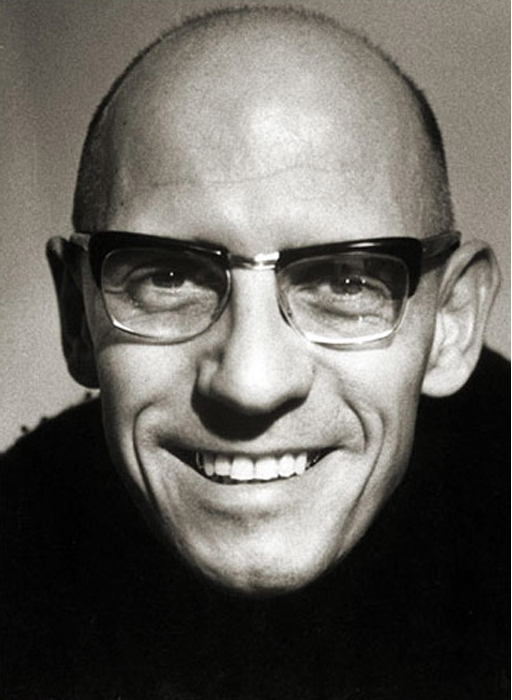
This is a photograph of Michel Foucault
One of the main criticisms of Foucault’s work is his failure to acknowledge the power of resistance. In their review of professional power, medical sociologists Simon Williams and Michael Calnan suggest that the traditional systems of medical knowledge are being challenged by developments such as mass media, greater access to information and alternative forms of health (and death). They conclude:
In this world of uncertain times, one thing remains clear: namely, that lay people are not simply passive or active, dependent or independent, believers or sceptics. Rather, they are a complex mixture of all of these things (and much more besides).
Challenges to medical power as forms of resistance (i.e. not ‘fitting’ the medical view) might include such things as the use of complementary and alternative medicine; seeking different opinions, including the use of the internet; or refusing to take medical advice. These are all problematic in that they depend on ‘other’ forms of power, many of which can be located within the broad realm of medical knowledge. Foucault’s arguments that discourses shape and produce people's identity do not take people out of the realm of being defined as ‘dying’. Thus resistance here is not convincing. The course authors would therefore argue that the notion of resistance can be viewed as much more subtle. The medical profession might be part of the force that is defining illness and wellness, but individual doctors are not necessarily consciously setting out to do so. Likewise, resistance can be viewed differently. Both dying unexpectedly and not dying when a terminal diagnosis has been given have been seen as forms of resistance. This is not necessarily a matter of conscious choice, but of the inappropriateness or lack of usefulness of the medical diagnosis. On one level, medical definitions of death and dying are literally being resisted. An OU academic has argued that care home staff try to manage the period of dying, despite the reality that the bodies of ageing and frail residents are in a gradual but highly uneven decline into death and resistant to being categorised as either living or dying (Komaromy, 2001). Furthermore, regardless of any definition that might be made about their status, their bodies will continue to deteriorate.
Conclusion
This free course provided an introduction to studying Health and Social Care. It took you through a series of exercises designed to develop your approach to study and learning at a distance and helped to improve your confidence as an independent learner.
This OpenLearn course provides a sample of level 2 study in Health & Social Care. If you find this course interesting, take a look at the Open University course K220 Death, Dying and Bereavement. Alternatively, you can explore the related OpenLearn course, An introduction to death, dying and grief.
References
Acknowledgements
This course was first published in 2008 and updated in 2020.
Grateful acknowledgement is made to the following sources for permission to reproduce material in this course:
Course image: Val D'Aquila in Flickr made available under Creative Commons Attribution-NonCommercial-ShareAlike 2.0 Licence.
The content acknowledged below is Proprietary and used under licence (not subject to Creative Commons licence). See Terms and Conditions.
Figure 1 © JupiterImages/Banana Stock/Alamy;
Figure 2 © Gary Calton/Alamy;
Figure 3 © Spa Press/Rex Features.
Don't miss out:
If reading this text has inspired you to learn more, you may be interested in joining the millions of people who discover our free learning resources and qualifications by visiting The Open University - www.open.edu/ openlearn/ free-courses
This free course is adapted from a former Open University course called 'Death and dying (K260).'
Copyright © 2016 The Open University