Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Friday, 26 April 2024, 9:56 PM
Communicable Diseases Module: 34. Intestinal Protozoa, Ascariasis and Hookworm
Study Session 34 Intestinal Protozoa, Ascariasis and Hookworm
Introduction
In the previous study session, you learned about the most common faeco-oral diseases caused by bacteria or viruses. In this study session, we will describe the main intestinal parasitoses (pronounced ‘para-sit-oh-seez’), i.e. diseases caused by parasites living in the intestines. You will learn about the intestinal protozoa (single-celled organisms) causing amoebiasis and giardiasis, and the intestinal helminths known as ascaris worms and hookworms. There are other, much larger, intestinal parasites in addition to those described here, such as the tapeworms, which you will learn about in Study Session 38.
It is important for you to know about these diseases so that you can treat or refer cases and apply prevention and control measures in your community. The prevention and control measures for these conditions are the same as you have already learned in earlier study sessions in relation to other faeco-oral diseases. However, you will notice that there are significant differences in the symptoms and treatment of the parasitic diseases described here.
Learning Outcomes for Study Session 34
When you have studied this session, you should be able to:
34.1 Define and use correctly all of the key words printed in bold. (SAQs 34.1, 34.2 and 34.3)
34.2 Identify the common causative agents, occurrence and modes of transmission of the common faeco-oral diseases caused by intestinal protozoa and roundworms. (SAQs 34.2, 34.3 and 34.4)
34.3 Explain how you would diagnose and treat cases of amoebiasis, giardiasis, ascariasis and hookworm infection, based on their symptoms and signs, and when and why you would refer them to a higher-level health facility. (SAQs 34.1, 34.2, 34.3 and 34.4)
34.4 Describe how you would apply prevention and control measures against these common intestinal parasitoses. (SAQs 34.2 and 34.5)
34.1 Intestinal protozoal diseases
The two commonest types of faeco-oral diseases caused by intestinal protozoa are ameobiasis (or amoebic dysentery) and giardiasis. Both conditions are also classified as diarrhoeal diseases based on the characteristic symptom of diarrhoea. The prevention and control measures against both diseases are the same as for other faeco-oral diseases described previously (refer back to Study Session 32, Section 32.6). Our focus here will be on the unique features that enable you to suspect cases of these diseases, and refer patients after starting rehydration with oral rehydration salts (ORS).
34.1.1 Amoebiasis
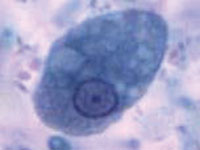
Amoebiasis is a disease resulting from infection of the large intestine (colon) by a protozoan parasite called Entamoeba histolytica.
The distribution of this single-celled parasite is very widespread – the WHO estimates that around 500 million people around the world are infected with these amoebae (Figure 34.1). It is endemic in Ethiopia, and research studies have shown a prevalence of amoeba infection ranging from 4% to 19% in the Ethiopian population.
However, most people with amoebae in their intestines show no symptoms, but they can pass on the amoebae to others and are an important reservoir of infection. Individuals who develop amoebiasis (the plural amoebae is pronounced ‘amm-ee-bee’), experience bloody diarrhoea (so the disease is also known as ameobic dysentery), fever and abdominal cramps, sometimes alternating with periods of constipation. Unlike in cases of bacillary dysentery, the blood and mucus is mixed with solid stool and patients are not usually bedridden. Very rarely, amoebiasis can lead to serious complications, including abscesses in the liver, lungs or brain.
Another difference between dysentery caused by ameobae and dysentery caused by Shigella bacteria is that amoebiasis mainly affects young adults; it rarely occurs below the age of five years. By contrast, dysentery in children under ten years is mainly due to Shigella species. Also, amoebiasis does not usually produce epidemics, so an epidemic of dysentery is most probably due to cases of shigellosis.
Some amoebae in an infected person’s intestines transform and become encased in a round protective membrane called a cyst. The cysts pass out of the body in the faeces. They are highly resistant to damage and can be transmitted by direct and indirect faeco-oral routes, mainly via contaminated food or water. They hatch out in the new person and the protozoa rapidly increase in number by cell division.
For accurate diagnosis, laboratory identification of the cysts in the patient’s stool is necessary to differentiate it from shigellosis. Therefore, you should start any patient with dysentery on rehydration with ORS and refer them to the nearest higher level health facility for further investigation and specialist treatment. Advise the patient or caregiver that further investigation is needed for diagnosis and that early treatment is important because the disease could lead to serious outcomes.
34.1.2 Giardiasis
Giardiasis is a faeco-oral disease which results from infection of the small intestine by protozoa called Giardia intestinalis, also known as Giardia duodenalis. (Note: the same protozoa are called Giardia lamblia in older textbooks.) Studies have shown the prevalence of Giardia infection in Ethiopia ranges from 2.0% to 11.4% of the population. Like the parasitic amoebae described in the previous section, Giardia form resistant cysts in the person’s intestines (Figure 34.2) that pass out in the faeces. The cysts can be easily transmitted in water contaminated by faeces, from person-to-person through hand-to-mouth transmission and in food. They hatch out in the new person and the protozoa rapidly increase in number by cell division.
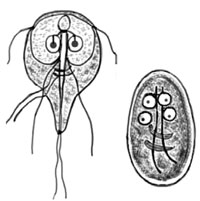
The commonest clinical manifestation of giardiasis is foul-smelling, pale, greasy diarrhoea, without blood or mucus (mucoid). The diarrhoea can be acute and resolve by itself within a few days, or it may be persistent (lasting for more than 14 days). Other symptoms of giardiasis include nausea, vomiting, abdominal cramps and abdominal distension (swelling).
Details of the specific management of children with persistent or severe diarrhoea are taught in the Module on the Integrated Management of Newborn and Childhood Illness.
You should suspect giardiasis in children if the diarrhoea is persistent, but not bloody or mucoid. For children with mild non-bloody or non-mucoid diarrhoea, the management does not require identification of the infectious agent; cases are managed with oral rehydration as already described for simple acute watery diarrhoea (refer back to Section 32.4.2). If a child has persistent or severe diarrhoea, and giardiasis is one of the causes you suspect, treatment is carried out at a higher-level health facility on a case-by-case basis, taking into account the presence of other symptoms and/or malnutrition. Therefore, you should start ORS treatment and refer the child.
In adults, you should suspect a diagnosis of giardiasis in cases with acute or persistent, non-bloody or non-mucoid diarrhoea. However, as other diseases could also have similar manifestations, confirmation of the diagnosis is needed through detection of the parasite in laboratory examination of stool samples. Therefore, start all adult patients on rehydration with ORS and refer them for further diagnosis and treatment.
Amoebiasis and giardiasis both present with diarrhoea. What is the difference in the type of diarrhoea resulting from the two diseases?
The main difference in the type of diarrhoea is that in amoebiasis it is bloody or mucoid (contains mucus), whereas in giardiasis it is pale, greasy and foul smelling.
34.2 Intestinal roundworms
In this section, you will learn about diseases caused by roundworms living in the intestines. Helminths is the collective name given to parasitic worms. They have complicated lifecycles, and some helminths require transmission between humans and other host animals before they mature. There are three main groups of helminths: the roundworms, the tapeworms and the flatworms (or flukes). Here we focus on intestinal roundworms (helminths that are round in cross-section), which live in the person’s intestines and exit from the body in the faeces. The two commonest intestinal roundworms in Ethiopia cause the diseases known as ascariasis and hookworm infection. Neither of these conditions is characterised by diarrhoea, so they are not classified as diarrhoeal diseases.
34.2.1 Ascariasis
Like other faeco-oral diseases, you need to know the main features of ascariasis: its infectious agent, occurrence, modes of transmission, symptoms and signs, diagnosis and treatment. Prevention and control measures are similar to those for other faeco-oral diseases, described in earlier study sessions. However, ascariasis requires specific drug treatment based on its symptoms and signs.
Ascariasis results from infection of the small intestine with a helminth parasite called Ascaris lumbricoides. It is the largest of the intestinal roundworms; mature worms can measure 15–35 cm in length (Figure 34.3). It is the commonest of all the faeco-oral diseases caused by parasitic helminths. It mainly affects children, particularly between three to eight years of age. In Ethiopia, around 37% of the population is estimated to be infected with Ascaris lumbricoides.

The complicated lifecycle of ascaris worms is shown in Figure 34.4 and is essential for their full development into egg-laying adults. In the descriptions that follow, the numbers relate to the numbers on each stage shown in Figure 34.4. Adult Ascaris lumbricoides worms in the intestines (1) lay eggs which pass out with the faeces (2). The eggs are transmitted faeco-orally by ingestion of contaminated food, water, etc. (stages 2 to 4). The eggs hatch and develop into larvae (immature stage) in the intestines (5). The larvae are carried in the bloodstream to the lungs, where they develop further (6). They migrate upwards from the lungs into the throat (7), where they are swallowed – returning once again to the person’s intestines. Male and female worms mate and the females lay eggs in the intestines (1), which pass out in the faeces (2), and are ingested by new hosts – beginning the lifecycle all over again.

Cases of ascariasis manifest with abdominal discomfort, and live worms may be seen in the stools, vomit or occasionally emerging from the nose. You can make a clinical diagnosis of ascariasis if the patient or the caregiver of a child tells you that long worms have passed with the stool or vomit, or if you are able to see the worms yourself. Eggs in the faeces are too small to see with your eyes, and although they can be identified by laboratory diagnosis of stool samples, there is no need to send samples for investigation or refer the patient – unless there are obvious signs of anaemia (see Box 34.1 in the discussion of hookworm infection later in this study session). You can treat mild cases yourself, and you should also give all children aged between two to five years routine treatment to kill intestinal worms, as described next.
Treatment for ascariasis and routine deworming
If you diagnose ascariasis, the treatment schedule is as given in Table 34.1. There are two drugs (albendazole and mebendazole), both available in either liquid or tablet form. However, even if there are no signs of worm infection, routine deworming is recommended for all children aged 24 months or older who have not been treated in the previous six months. Give every child that you see in this category the appropriate dose of albendazole or mebendazole every six months to treat intestinal worms. Chewable deworming tablets that taste good are available. For children who find swallowing a tablet difficult, you can crush it between two spoons and mix it with a little water to help them to take the dose. This regimen kills hookworms as well as ascaris worms.
![]() Do not give either albendazole or mebendazole to pregnant women who are in their first 14 weeks of pregnancy.
Do not give either albendazole or mebendazole to pregnant women who are in their first 14 weeks of pregnancy.
| Drug | Age 0 to 2 years | Age 2 to 5 years |
|---|---|---|
| Albendazole (400 mg tablet) | None | 1 tablet (400 mg) |
| Medendazole (100 mg or 500 mg tablets) | None | 1 x 500 mg tablet (or 5 x 100 mg tablets) |
| Mebendazole oral suspension (Figure 34.5) | 2.5 teaspoons (250 mg) | None |

34.2.2 Hookworm infection
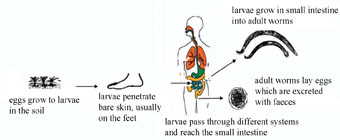
Hookworm infection is transmitted via contact with faeces, but it is not actually a faeco-oral disease, because the infection does not enter through the mouth, as you will see below in our discussion of its transmission process. However, it is appropriate to discuss hookworm infection with other faeco-oral diseases because the infectious agents exit from the body in the faeces, the routine deworming regimen is the same as for ascariasis (Table 34.1 above), and prevention and control includes the measures already described for other faeco-oral diseases (see Study Sessions 32 and 33).
Hookworms live in the small intestine and suck blood from blood vessels in the intestinal walls. The main infectious agents are called Necator americanus and Ancylostoma duodenale. Hookworm infection is endemic in Ethiopia, especially in areas where people walk barefooted and sanitary conditions allow faeces to contaminate the soil. In Ethiopia the prevalence of hookworm infection is estimated to be around 16% of the population.
During the transmission process (Figure 34.6), immature parasites (larvae) in the soil enter the body by penetrating the skin, usually through bare feet. The larvae then migrate to the small intestine, after passing through different body systems. In the small intestine, the adult worms mate and the females lay eggs which are excreted with the faeces. The eggs develop in the soil into larvae, which can then be transmitted to new individuals through the skin.
What preventive measure should you advise people in your community to apply to protect themselves from hookworms?
In addition to all the measures involving personal hygiene after defaecation, before food preparation and when eating etc., you should specifically educate your community to interrupt the transmission of hookworms by:
- Wearing shoes to prevent the parasites from entering through skin while walking barefooted.
- Using latrines, disposing of faeces safely and stopping open defaecation in fields, to prevent contamination of soil with the parasites.
Diagnosis and treatment of hookworm infections
Cases of chronic hookworm infection manifest with abdominal pain and the symptoms and signs of anaemia (see Box 34.1), due to blood loss caused by the blood-sucking worms. It is very important that you treat worm infestations routinely in children aged from two to five years, because persistent hookworm infections (like ascariasis) causes a significant loss of micronutrients (minerals and vitamins) from the body. Infected individuals may develop anaemia, which can be life-threatening. Anaemic children fail to grow properly and their school performance will be negatively affected.
Box 34.1 Anaemia: a common sign of ascariasis or hookworm infection
Anaemia refers to a deficiency of haemoglobin in the blood. Haemoglobin is the red, iron-rich protein that gives red blood cells their colour and enables them to pick up oxygen and transport it around the body. Symptoms and signs of anaemia include becoming easily tired; pallor (paleness) inside the eyelids, gums, nails and palms of the hands (Figure 34.7); shortness of breath; and a fast pulse rate, which an anaemic person may notice as their heart beating fast even when they are quietly resting. Therefore, routine deworming of children aged between two to five years, every six months, according to the dosages given in Table 34.1 earlier, is essential to kill hookworms as well as ascaris worms.

In the next study session, we turn to the largest single cause of mortality among children under the age of five years: acute respiratory tract infections.
Summary of Study Session 34
In Study Session 34, you have learned that:
- Parasitic infection of the intestines could be due to protozoa or helminths.
- Common types of intestinal protozoal infections in Ethiopia include ameobiasis and giardiasis.
- Ameobiasis presents with dysentery (stools containing blood and mucus). Amoebic dysentery is rare in children, in contrast to shigellosis (bacillary dysentery) which mainly affects young children. Suspected cases of amoebiasis should be started on rehydration with ORS and then referred for laboratory diagnosis and treatment.
- Giardiasis presents with pale, greasy and foul-smelling diarrhoea. For children with mild cases, treat as for acute watery diarrhoea, by rehydrating with ORS. For persistent or severe cases in children, and all adults with suspected giardiasis, start rehydration and then refer them for laboratory diagnosis and treatment.
- Common diseases caused by intestinal helminths in Ethiopia include ascariasis and hookworm infection.
- Ascariasis is the commonest intestinal helminth infection in children. Cases present with abdominal discomfort and you may see the passage of live worms with the faeces or vomit. Treat cases with albendazole or mebendazole according to the schedule in Table 34.1.
- Hookworm infection is a common cause of anaemia in areas where walking barefooted is common and sanitary conditions are poor. Refer suspect cases for laboratory confirmation and educate the community on shoe wearing, use of latrines and proper disposal of faeces.
- All children aged between two to five years should be routinely dewormed every six months, using the dosages in Table 34.1, to kill ascaris and hookworms.
Self-Assessment Questions (SAQs) for Study Session 34
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the questions below. Some questions also test some Learning Outcomes of Study Sessions 32 or 33. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 34.1 (test Learning Outcomes 33.1, 33.4, 34.1 and 34.3)
Suppose a 30-year-old man came to you complaining of diarrhoea. You asked about the type of diarrhoea and the patient described it to you. Which diseases do you suspect, if he describes the diarrhoea as:
- a.Bloody with mucus?
- b.Watery?
- c.Pale and greasy?
How should you manage the patient in each of the above cases?
Answer
- a.The diseases that you should suspect as causes of bloody diarrhoea are shigellosis (bacillary dysentery) and amoebiasis (amoebic dysentery).
- b.The diseases that you should suspect as causes of watery diarrhoea include cholera or a viral diarrhoeal disease (although rotavirus infection is not common in adults).
- c.If the patient describes his condition as greasy diarrhoea, you should suspect giardiasis.
Irrespective of the type of diarrhoea, the adult patient should be started on rehydration with ORS and referred to a higher level health facility for laboratory investigation and treatment.
SAQ 34.2 (test Learning Outcomes 34.1, 34.2, 34.3 and 34.4)
A mother brought her five-year-old child complaining of long round worms coming out with the child’s stool.
- a.What is your diagnosis and how should you manage the child’s condition?
- b.What measures do you undertake at community level to decrease such infections?
Answer
- a.Your diagnosis is infection with ascaris worms (ascariasis). You should treat the five-year-old child with 1 tablet of albendazole (400 mg) or 1 tablet of mebendazole (500 mg) to be taken orally.
- b.You should also give health education to the mother and the community on measures to interrupt faeco-oral transmission via hand-to-mouth transfer of the ascaris eggs from the soil, and prevention of transmission in contaminated water and food. Using latrines, safe disposal of faeces, and avoiding open defaecation in fields prevents contamination of soils with faeces containing the worm eggs.
SAQ 34.3 (test Learning Outcomes 34.1, 34.2 and 34.3)
Abebe is a farmer who came to you with symptoms of anaemia.
- a.What possible causes of anaemia do you consider?
- b.What evidence would suggest hookworm infection?
- c.How do you manage Abebe’s illness?
Answer
- a.The common causes of anaemia to be considered include malaria, malnutrition, a recent history of bleeding, and hookworm infection.
- b.The evidence that suggests hookworm infections is the absence of other obvious causes (e.g. if malaria is not locally endemic, or the malaria rapid diagnostic test is negative), and the presence of risk factors for hookworm – walking barefooted in areas where faeces contaminate the soil.
- c.Whatever the cause, refer Abebe to a higher level health facility for laboratory diagnosis and treatment if he has hookworms, or diagnosis of another cause, and treatment for his anaemia.
SAQ 34.4 (tests Learning Outcomes 33.3, 33.4, 34.2 and 34.3)
List the main differences between amoebiasis and shigellosis in terms of their occurrence, symptoms and signs.
Answer
Some differences between amoebiasis and shigellosis are:
- Amoebiasis is more common in young adults, but shigellosis is more common in children below ten years
- Amoebiasis is an endemic disease that rarely causes an epidemic, whereas shigellosis (though also endemic) can rapidly spread and cause an epidemic
- The bloody diarrhoea in amoebiasis contains some formed stools, but in shigellosis only blood and mucus comes out when the patient strains to defaecate
- A patient with amoebiasis is rarely ill enough to remain in bed, whereas someone with shigellosis may be bedridden due to severe dehydration.
SAQ 34.5 (tests Learning Outcome 34.4)
How are the prevention and control measures for ascariasis and hookworm infection:
- a.the same?
- b.different?
Answer
- a.The route of exit for the eggs of ascaris worms and hookworms is the same – with the faeces. Prevention and control measures that are common to both diseases are use of latrines, safe disposal of faeces, and avoiding open defaecation in fields. This prevents contamination of soils with infected faeces. Another similarity is that routine deworming of children aged two to five years every six months with albendazole or mebendazole reduces the reservoir of both diseases in the community.
- b.The difference is that the route of entry for ascariasis is through the mouth, while for hookworm infection it is through the skin, usually on bare feet. Prevention and control measures for ascariasis involve prevention of hand-to-mouth transmission of the infectious agents, and avoiding contamination of food and drinking water. In addition, to the measures described in (a), prevention and control measures for hookworm include wearing shoes.