Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Thursday, 25 April 2024, 2:09 AM
Family Planning Module: 4. Natural Family Planning (NFP) Methods
Study Session 4 Natural Family Planning (NFP) Methods
Introduction
In your community you have an important role to play, helping people choose a contraceptive method that is personally and medically appropriate for them. To do this effectively, it’s important to understand the various ways and methods by which unwanted or unplanned pregnancy can be prevented. These contraceptive methods are generally classified into natural and artificial (modern) methods. Natural family planning uses changes in the body to identify when a woman is fertile and could become pregnant. This is also known as a fertility-based awareness method.
In this study session, you will learn about the concepts, types, mechanism of actions, the advantages and disadvantages of each natural family planning method. These include the temperature method, calendar method, cervical mucus method, lactational amenorrhoea method (LAM) and coitus interruptus, or the withdrawal method.
Learning Outcomes for Study Session 4
When you have studied this session, you should be able to:
4.1 Define and use correctly all of the key words printed in bold. (SAQs 4.1 and 4.2)
4.2 Describe the concepts and types of natural family planning methods. (SAQs 4.1, 4.2 and 4.3)
4.3 Describe the mechanism of action of natural family planning methods. (SAQ 4.3)
4.4 Describe the advantages, disadvantages and effectiveness of natural family planning methods. (SAQs 4.1, 4.3 and 4.4)
4.5 Explain the procedures for using each natural family planning method to the people in your community. (SAQ 4.4)
4.1 The concepts of natural family planning methods
Natural family planning (NFP) is the method that uses the body’s natural physiological changes and symptoms to identify the fertile and infertile phases of the menstrual cycle. Such methods are also known as fertility-based awareness methods.
In Study Session 5 of the Antenatal Care Module, you learnt about the physiological processes and observable changes during the menstrual cycle. Once a month an egg is released from one of a woman’s ovaries (ovulation); it can stay alive in the uterus for about 24 hours. Men can always produce sperm cells, and these can stay alive in the female reproductive system for about two to five days after being deposited in the vagina during sexual intercourse. What this means is that from a fertility point of view, women have periods of time during their cycle when they are unlikely to conceive, whereas men have no ‘safe period’.
How is it possible to identify when the woman is in the ‘safe period’ (when pregnancy is not possible) and when she is in the ‘unsafe period’ (when she could get pregnant)?
There are physiological changes during the menstrual period that help to distinguish between the ‘unsafe period’ (when pregnancy is possible) and the ‘safe period’ (when pregnancy is not possible).
In what way can natural family planning methods prevent pregnancy?
Natural family planning methods prevent pregnancy by making it impossible for the egg and sperm to meet.
However, these methods depend on the awareness and ability of the couple to identify the fertile and infertile phase of each menstrual cycle, and also require cooperation between the couple to abstain from, or to have, sexual intercourse, depending on whether they are trying to avoid or achieve pregnancy.
4.1.1 Advantages
Natural family planning methods are generally the preferred contraceptive method for women who do not wish to use artificial methods of contraception for reasons of religion, or who, due to rumours and myths, fear other methods.
4.1.2 Disadvantages
Natural family planning methods are unreliable in preventing unwanted pregnancy. It takes time to practise and use them properly, which adds to their unreliability. Additionally, natural family planning methods do not protect against sexually transmitted infections (STIs), including the human immunodeficiency virus (HIV). You should advise couples to use condoms to protect against STIs.
4.1.3 Effectiveness
The effectiveness of any method of natural family planning can vary from couple to couple, and all these methods are less effective for couples who do not follow the method carefully.
4.2 Types of natural family planning methods
In order to understand the ways that natural family planning methods can prevent pregnancy, it is important for you to know each type and its techniques of use. There are three major classifications of natural family planning methods:
- Periodic abstinence (fertility awareness) method
- Use of breastfeeding or lactational amenorrhoea method (LAM)
- Coitus interruptus (withdrawal or pulling out) method.
4.2.1 Periodic abstinence (fertility awareness) methods
During the menstrual cycle, the female hormones oestrogen and progesterone cause some observable effects and symptoms:
- Oestrogen produces alterations in the cervical mucus, which changes from thick, opaque and sticky to thin, clear and slippery as ovulation approaches.
- Progesterone produces a slight rise in basal body temperature (temperature at rest) after ovulation. Otherwise, the function of progesterone on the cervical mucus is just the opposite effect of oestrogen — it makes the cervical mucus thick, opaque and sticky.
Observation of these changes provides a basis for periodic abstinence methods. There are three common techniques used in periodic abstinence methods, namely:
- Rhythm (calendar) method
- Basal body temperature (BBT) method
- Cervical mucus (ovulation) method.
Calendar or rhythm method
This method is the most widely used of the periodic abstinence techniques. The calendar method is a calculation-based approach where previous menstrual cycles are used to predict the first and the last fertile day in future menstrual cycles. This method requires a good understanding of the fertile and infertile phases of the woman’s menstrual cycle. It is based on the regularity of the menstrual cycle and the fact that an ovum (egg) can only be fertilised within 24 hours of ovulation.
What do you know about the regular and irregular menstrual cycle of a woman?
A regular menstrual cycle is when monthly bleeding happens every month or 28 days.
An irregular menstrual cycle is when monthly bleeding is variable from month to month, for example it can vary from 25 to 32 days in some women.
It is important for you to know that before relying on this method a woman needs to record the number of days in each of her menstrual cycles for a period of at least 6–8 months (remembering that the first day of menstrual bleeding is always counted as day 1). See Box 4.1 on how to advise women using the calendar method.
Box 4.1 Advice to women using the calendar method
For irregular cycles, identify the longest and the shortest cycles recorded over six to eight cycles.
- Subtract 18 from the shortest cycle (gives the first day of the fertile phase).
- Subtract 11 from the longest cycle (gives the last day of her fertile time).
- Avoid sex, use a barrier method, or use withdrawal during the fertile phase calculated.
Example 1
A woman’s last six menstrual cycles were 28, 26, 29, 27, 29 and 27 days. Using this information, calculate and instruct her about how to use the calendar method to prevent pregnancy.
- Her shortest cycle is 26 days.
- Her longest cycle is 29 days.
- First day of her fertile phase is 26 - 18 = 8.
- Last day of her fertile phase is 29 - 11 = 18.
Therefore, the fertile period of this client is between the 8th–18th days, so she should avoid sex during this period to prevent pregnancy.
However, if the client’s menstrual cycle is regular and comes every 28 days or close to it, ovulation should occur about 14 days before the next period. For this reason, the woman should count backwards 14 days from her next period to calculate the day she will ovulate. Consequently, she should avoid sex from about seven days before that day until about two days after ovulation is expected.
Example 2
A client comes to you and asks about using the calendar method to prevent pregnancy. When you ask her about the history of her menstrual cycle over the last six months, she tells you it comes regularly every 30 days. Calculate the fertile period of your client and advise her when to avoid sex in order to prevent pregnancy.
Regular cycle 30 - 14 = 16 First day of fertile phase 16 - 7 = 9 Last day of fertile phase 16 + 2 = 18 Therefore, her fertile period is between the 9th and 18th days, and she should avoid sex between these days of the cycle.
Advantages of the calendar or rhythm method
This method does not require daily monitoring of fertility indicators.
Disadvantages of the calendar or rhythm method
It is associated with a high failure rate and can be difficult to use in the case of irregular menstrual cycles. It also takes a long time to learn and use it properly.
Effectiveness of the calendar or rhythm method
This method is about 95% effective if a woman uses it correctly (Family Planning: A Global Handbook for Providers, World Health Organization (WHO), 2007).
What can a couple do if they are not confident about using this method?
The couple should be advised to use additional methods, like condoms or other barrier methods, to prevent unwanted pregnancy. You should provide them with the necessary resources.
Basal body temperature (BBT) method
The basal body temperature method is based on the slight increase in the body temperature of women at rest by about 0.3–0.5°C during and after ovulation, due to the action of an increased level of progesterone secreted by the corpus luteum. The rise in body temperature sustained for three consecutive days indicates that ovulation has occurred, and it remains at this increased level until the start of the next menstrual cycle. In this section you will learn about when the rise in body temperature occurs, and what women need to know in order to use this method properly.
This natural family planning method may be selected if the woman is not willing to touch her genitalia to check her cervical secretions (as in the cervical mucus method), but is willing to abstain from sexual intercourse with her spouse for long periods of time. It is difficult for a woman to use natural family planning methods if her menstrual cycle is irregular, as it may disturb the subtle changes in body temperature and cervical secretions, as a result of hormonal effects.
Advantages and disadvantages of BBT
The advantages and disadvantages of BBT are summarised in Table 4.1 below.
Advantages | Disadvantages |
|---|---|
No side-effects for this method. Encourages discussion about family planning between couples. | High failure rate if the couple do not clearly understand the method. Requires several days of abstinence. Needs a longer duration to practice, understand and use properly. False interpretation or indications in the case of fever, as this may mislead the result of BBT. A special thermometer may be required. |
Effectiveness of BBT
BBT is about 98% effective if the woman uses the method correctly (Family Planning: A Global Handbook for Providers, WHO, 2007). But it’s still important to realise that of 100 women using this method in any one year, two will become pregnant. Its effectiveness will decrease dramatically to 80% if the woman does not use the method correctly. Effectiveness is greatest when the couple limits unprotected sexual intercourse to the period after ovulation.
Method of BBT
To use the basal body temperature method effectively, you need to know and teach women how to read a thermometer and record the results on a special chart or graph paper. Figure 4.1 shows the period of time when a couple must avoid sexual intercourse or use other protective methods.
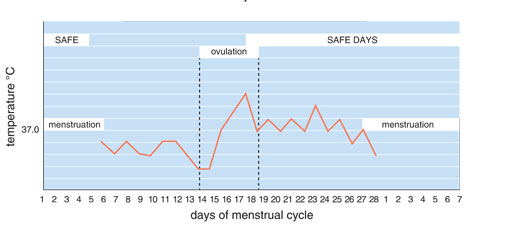
In Figure 4.1, on which days of the woman’s menstrual cycle does her temperature show a three-day rise?
It rises on days 15, 16 and 17. This indicates that ovulation has happened and passed.
If the temperature falls on or below the woman’s normal basal temperature during the three day count, that may indicate ovulation has not yet occurred. To avoid pregnancy, wait until three consecutive temperatures are recorded above the normal basal temperature.
After the beginning of the infertile phase (the third day of a rise in temperature or ‘peak day’), it is not necessary to take the temperature and it is possible to continue sexual intercourse until the first day of the next menstrual cycle.
In this regard, you should explain that the women needs to do the following:
- Place the temperature chart and thermometer at her bedside and decide initially whether to take her temperature either orally, vaginally or rectally, and use that same method all the time.
- Take the temperature immediately after waking up and before getting up from the bed in the morning, and before doing anything like drinking tea or coffee.
- Shake the thermometer to lower the mercury below 35ºC and place it either rectally or vaginally for about three minutes, or orally for four to five minutes to measure her body temperature. The rectal and vaginal routes are more consistent, but the oral route is adequate if it is used consistently.
- Read the thermometer after the required time and record the temperature; interpret whether there has been a rise in the temperature. Near ovulation, she will notice a rise of 0.3ºC‒0.5ºC.
- Abstain from (avoid) sexual intercourse from the first day of menstrual bleeding until the temperature has risen above the regular temperature and stays up for three full days.
- Know that after the third day (peak day) it is safe to have unprotected sexual intercourse, until the next menstrual bleeding begins.
How long does the ovum remain viable?
The ovum remains viable for at least 24 hours. It is important to note that because the woman cannot be sure exactly when she ovulated, she should be cautious about resuming sexual intercourse.
There is a lot of information in this section. You may wish to go through the basal body temperature method several times so that you are confident that you can explain it to couples who wish to practise this method. They will be more likely to follow the procedure carefully if they understand what is happening in the woman’s body.
Cervical mucus method (CMM)
The cervical mucus method (or Billings method) is based on the recognition and interpretation of changes in cervical mucus and sensations in the vagina, due to the effect of changes in oestrogen levels during the menstrual cycle. This method is also an ovulation method used by women trying to get pregnant and have a child.
Mechanism of action of CMM
You may remember from the description of natural family planning methods, that the rise in the level of oestrogen during the menstrual cycle influences the cervical gland to secrete mucus that changes from a sensation of dryness in the vagina (characterised by thick, viscous and sticky mucus), to a sensation of wetness in the vulva (characterised by thin, white, slippery and stretchy thread-like, transparent strands — similar to uncooked egg white), during ovulation.
Using this method, these are the times when it is safe to have sexual intercourse:
- After menstruation ends the dry days (absence of cervical secretions) will start, and during these days it is safe to have sexual intercourse every other night until a woman starts to feel wet in her vagina. Every other night is suggested, as it will help women from confusing semen with cervical mucus.
- It is also safe from the evening of the fourth day after the peak day, to the beginning of the next menstruation. Once a woman has ovulated, her cervical mucus will begin to dry up, so the peak day is the last day of cervical or vaginal wetness.
Effectiveness of CMM
The effectiveness of the cervical mucus method is about 97% if women use it correctly (Family Planning: A Global Handbook for Providers, WHO, 2007). The conditions which can affect correct use are summarised in Box 4.2.
Box 4.2 Conditions affecting the cervical mucus pattern in women
- If a woman has a vaginal or cervical infection.
- If a woman has recently had sexual stimulation (which will increase vaginal secretions).
- If a woman is currently taking drugs for colds or sinusitis, which may dry up mucus secretions.
- If a woman is in physical or emotional stress.
- If a woman is currently breastfeeding.
Advantages of CMM
The advantages of this method are similar to those associated with the use of the basal body temperature method.
Disadvantages of CMM
CMM has a high failure rate because it needs several days of abstinence and a lot of experience in using the method to be effective. It is also difficult to use this method in the case of vaginal infections, as the cervical mucus secretions may be misleading.
Method of CMM
You will need to carefully instruct women to be able to:
- Use a chart to record their mucus pattern.
- Look at their cervical mucus in the morning, and every time after using the toilet, using a clean cloth or tissue paper to determine the colour and consistency of the mucus.
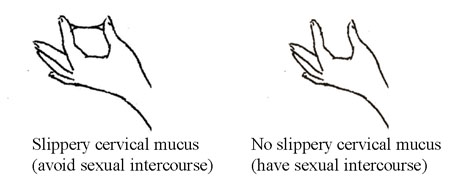
- Touch the secretion to determine its stretchiness and slipperiness (see Figure 4.2).
- Feel how wet the sensation is in their genitalia when they are walking.
- Abstain from sexual intercourse on the day when mucus appears, regardless of its consistency, until the third evening after the ‘peak day’ (see Table 4.2).
| Approximate day of menstrual cycle (phase) | How to identify | Intercourse allowed? |
|---|---|---|
| 1‒5: Menstruation* | Bleeding | No |
| 6‒9: Dry days | Absence of cervical mucus | On alternate nights only, to avoid confusion between mucus and sperm |
| 10: Fertile day | Onset of sticky mucus secretions (gradually becoming slippery over the following days) | No |
| 16: Peak fertile day | Last day on which slippery mucus (resembling raw egg white) is observed | No |
| 20: Fertile period ends | Evening of the fourth day after the peak day | After fertile period ends |
| 21‒29: Safe period (dry days) | From end of fertile period until onset of bleeding | Yes |
Footnotes
* The cycle begins on the day of menstruation.4.2.2 Lactational amenorrhoea method (LAM)
The lactational amenorrhoea method (LAM) is the use of breastfeeding as a contraceptive method. Lactational means breastfeeding and amenorrhoea means not having monthly bleeding. In this case, there is a delay in ovulation caused by the action of prolactin hormone from the effect of lactation or breastfeeding. An infant’s suckling of the nipple sends neural signals to the mother’s hypothalamus (part of the brain), which influences the anterior pituitary gland to secrete prolactin to stimulate the breast for milk production. This, in turn, inhibits the secretion of follicle stimulating hormone (FSH) and luteinizing hormone (LH), and as a result ovulation does not occur. While women are exclusively breastfeeding, prolactin continues to be secreted and pregnancy is unlikely. When prolactin levels decrease, the woman’s monthly bleeding may return, and if she continues to have unprotected sexual intercourse she may get pregnant.
All of these hormones were introduced, with their functions, in the Antenatal Care Module.
But the duration of suppression of ovulation is quite variable, depending on the breastfeeding status of the mother and the condition of the infant. To be fully effective the following three conditions must be met:
- The woman’s menstrual period must not have returned.
- The baby must be exclusively breastfed frequently, day and night. Exclusive breastfeeding, means the infant receives no food or fluids other than breastmilk.
- The baby must be less than six months old. This is because from six months onwards the baby needs to begin receiving complementary foods while continuing to be breastfed. The reduction in the amount of suckling at the breast may affect the hormonal mechanism, resulting in ovulation and menstruation returning, indicating a return of the woman’s fertility.
If any one of these three criteria changes, another contraceptive must be started immediately to prevent an unwanted pregnancy, and to ensure healthy birth spacing of at least three years.
Factors affecting LAM
Any factor that causes a decrease in suckling can result in the return of ovulation and decreased milk production. These factors include supplemental feeding of the infant, reduction in the number of breastfeeds or long intervals between breastfeeds, maternal stress and maternal/child illness. In these cases, the client should not rely on LAM.
Advantages and disadvantages of LAM
The advantages and disadvantages of LAM are summarised in Table 4.3.
Advantages | Disadvantages |
|---|---|
Effectively prevents pregnancy for at least six months. Encourages the best breastfeeding pattern. Can be used immediately after birth. Does not interfere with sexual intercourse. No hormonal side-effects. | Not a suitable method if the mother is working outside the home. No protection against STIs including HIV. If the mother has HIV, there is a small chance she may pass it to her baby in breastmilk. Not effective after six months. |
Effectiveness of LAM
If the woman follows the method correctly — it is 98–99% effective (Family Planning: A Global Handbook for Providers, WHO, 2007).
Important points about LAM
Women should use both breasts to breastfeed their babies on demand, with no more than a four hour interval between breastfeeds during the daytime, and no more than a six hour interval between breastfeeds during the night-time. If they are unable to fulfil these conditions, you should advise and provide them with a complementary family planning method. If a woman has any risk of STI/HIV infection, you should advise her to use condoms.
All these contraceptive methods are fully described in later study sessions in this Module.
If a woman wants to continue using LAM as a contraceptive method, but she fails to fulfill the LAM criteria, you should offer her advice on a complementary contraceptive method. In this case, the best choice would be a non-hormonal contraceptive (condoms, spermicides, diaphragms, IUCDs, and voluntary surgical contraception), because they don’t enter into the blood stream and interfere with breastmilk. If these non-hormonal contraceptives are not available, the next best choice would be to provide a progestin-only method, such as progestin-only pills, a DMPA injectable, or implants, as these do not interfere with breastmilk production. Note that contraceptive methods containing oestrogen reduce the production of breastmilk and generally are not recommended for lactating women.
4.2.3 Coitus interruptus (withdrawal or pulling out) method
Coitus interruptus or withdrawal is a traditional family planning method in which the man withdraws or pulls out his penis from his partner’s vagina and ejaculates outside, keeping his semen away from her genitalia.
Mechanism of action of withdrawal method
Coitus interruptus prevents fertilisation by stopping contact between spermatozoa in the sperm and the ovum or egg.
Advantages of withdrawal method
It is important for you to teach this method as part of natural family planning methods. It costs nothing and requires no devices or chemicals. It is available in any situation and can be used as a back-up method of contraception.
Disadvantages of withdrawal method
It has several disadvantages. Interruption of the excitement of sexual intercourse may result in the incorrect or inconsistent use of this method, as well as decreasing sexual pleasure for both partners. A high failure rate may be due to a lack of self-control, and semen containing sperm may leak into the vagina before the person ejaculates. There is a further possibility of premature ejaculation by the man. In addition, the couple is not protected from STIs, including HIV.
Effectiveness of withdrawal method
It is the least effective method because it depends on the man’s ability to withdraw before he ejaculates. However, it is about 73% effective if used correctly (Family Planning: A Global Handbook for Providers, WHO, 2007).
Summary of Study Session 4
In Study Session 4, you have learned that:
- To understand natural family planning methods it is important to remember that the egg is released from the ovary once a month and can stay alive in the uterus for about 24 hours. Men produce sperm cells which can stay alive in the female reproductive system for about 2–5 days after being deposited in the vagina during sexual intercourse.
- Knowledge of physiological changes during the menstrual period help to distinguish between the ‘unsafe period’ (when pregnancy is possible) and ‘safe period’ (when pregnancy is not possible).
- Natural family planning methods depend on the awareness and ability of the couple to identify the fertile and infertile phases of each menstrual cycle.
- The basal body temperature method is based on a slight three-day increase in the body temperature of women at rest by about 0.3‒0.5ºC during and after ovulation, which is caused by the action of a rise in the level of progesterone.
- The cervical mucus method is based on the recognition of changes in cervical mucus and on sensations in the vagina, due to the effect of oestrogen which changes the cervical mucus from dry or thick, viscous and sticky, to wet and thin, white, slippery and stretchy (similar to raw egg white) during ovulation.
- The calendar or rhythm method is based on calculations to predict the first and the last fertile day in future menstrual cycles.
- The lactational amenorrhoea method (LAM) is the traditional and most widely used method, based on the use of breastfeeding as a contraceptive method. To be effective as a method of contraception, three criteria should be fulfilled: menstruation should not have returned, the infant should not be more than 6 months old, and the baby should be exclusively breastfed.
- Coitus interruptus or withdrawal is another traditional family planning method in which the man withdraws or pulls out his penis and ejaculates outside the vagina, thus preventing his sperm reaching the woman’s egg and fertilising it.
Self-Assessment Questions (SAQs) for Study Session 4
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 4.1 (tests Learning Outcomes 4.1, 4.2 and 4.4)
Give reasons why natural family planning methods may be preferred by some women. What should couples be prepared to do in order to use natural family planning methods effectively?
Answer
Natural family planning methods are preferred by women who do not wish to use artificial methods of contraception or who, for reasons of religion, rumours or myths, fear using other methods. Couples with lower levels of education can use natural family planning methods effectively, providing the couple are highly motivated and have been well trained in the method. They should be prepared to avoid sex, or use withdrawal or a barrier method during the woman’s fertile period.
SAQ 4.2 (tests Learning Outcome 4.2)
How reliable are natural family planning or fertility awareness-based methods of contraception?
Answer
For many women who know their fertile period and have used a fertility awareness-based method consistently for a long period of time, the method can be reliable. However, the failure rate is higher when compared with other contraceptive methods.
SAQ 4.3 (tests Learning Outcomes (4.2, 4.3, and 4.4)
List the criteria that have to be fulfilled for the effectiveness of LAM in preventing pregnancy.
Answer
The criteria are:
- The woman’s period must not have returned.
- The baby must be exclusively breastfed day and night.
- The baby must be less than six months old.
SAQ 4.4 (tests Learning Outcomes 4.4 and 4.5)
W/ro Abebech is three months postpartum and using LAM for contraception. Her baby has just started sleeping for more than six hours during the night.
- a.Can she continue using LAM as a reliable contraception? State your reasons.
- b.If not, what would be her first choice of contraceptive method?
- c.What would be her second best choice of contraceptive method?
Answer
- a.No. If the infant takes more than a six-hour interval between feeds during the night, the mother is advised to start a complementary family planning method.
- b.The first choice would be a non-hormonal contraceptive, such as condoms, spermicides, diaphragms, IUCDs, or voluntary surgical contraception. This is because these methods do not enter the bloodstream and interfere with the production of breastmilk.
- c.The second choice would be to provide progestin-only methods, such as progestin-only pills, a DMPA injectable or implants. These methods do not interfere with breastmilk production.