Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Wednesday, 24 April 2024, 10:47 AM
Hygiene and Environmental Health Module: 23. Healthcare Waste Management
Session 23 Healthcare Waste Management
Introduction
Improper handling and disposal of healthcare wastes (also sometimes called medical waste) puts the health worker, the patient and the community at large at risk through transmission of pathogens via blood or body fluids, contaminated medical equipment, or sharp instruments. In this study session, you will learn to identify the types and sources of healthcare waste. The session also describes the components of waste management and the disposal methods for these wastes. Recognising the health risks involved in poor healthcare waste management and practising proper medical waste disposal will help protect everyone from the hazards of healthcare waste.
Learning Outcomes for Study Session 23
When you have studied this session, you should be able to:
23.1 Define and use correctly all of the key words printed in bold. (SAQ 23.1)
23.2 Distinguish between the types, and identify the risks, of medical waste. (SAQ 23.2)
23.3 Describe the handling and disposal requirements for healthcare waste. (SAQs 23.3 and 23.4)
23.4 Describe the health risks to health workers or patients related to sharps injuries. (SAQ 23.4)
23.1 Sources and classification of healthcare waste
Healthcare waste can be defined as any waste produced by healthcare activities. It may also be known as medical waste, hospital waste or infectious waste. The major sources include hospitals, Health Posts, emergency medical care services, healthcare centres and dispensaries, obstetric and maternity clinics, outpatient clinics, and the like. Other sources are dental clinics, psychiatric hospitals, cosmetic ear-piercing and tattoo parlours, and illegal drug users. Healthcare waste can be put into one of two broad categories; non-hazardous ‘general waste’ and hazardous ‘healthcare risk waste’.
Between 75% and 90% of the waste produced in healthcare establishments is general waste. This includes papers, packaging materials, dust and the like. This can be disposed of in the same way as other non-hazardous wastes, but only if is not contaminated by contact with hazardous wastes. The remaining 10–25% of waste is hazardous and could be composed of sharps (needles, lancets, etc.), syringes, blood or body fluid, contaminated surgical instruments, delivery bowls, used gauzes and gloves, plasters, etc. It may also contain expired drugs, lab reagents and other chemicals. Your main concern here should be on managing the hazardous wastes in a safe way. However, you should not ignore non-hazardous wastes, because poor handling and segregation can lead to them being contaminated with hazardous materials.
You can categorise hazardous healthcare waste into:
- Infectious waste: waste that may contain pathogens. This includes used dressings, swabs and other materials or equipment that have been in contact with infected patients or excreta. It also includes liquid waste such as faeces, urine, blood and other body secretions.
- Pathological waste: human tissues including placentas, body parts, blood and fetuses. Anatomical waste is a sub-group of pathological waste and consists of recognisable body parts.
- Sharps: needles, infusion sets, scalpels, blades and broken glass.
- Pharmaceutical waste: expired or no longer needed pharmaceuticals; items contaminated by or containing pharmaceuticals (bottles, boxes).
- Genotoxic waste: substances with genotoxic properties (meaning they can cause genetic damage) such as certain drugs and genotoxic chemicals.
- Chemical waste: wastes containing chemical substances such as laboratory reagents, film developer, disinfectants that are expired or no longer needed, and solvents.
- Waste with high content of heavy metals: includes batteries, broken thermometers, blood-pressure gauges, etc.
- Pressurised containers: gas cylinders, gas cartridges and aerosol cans.
- Radioactive waste: containing radioactive substances from radiotherapy or laboratory research.
You should note that the last five on the list may not necessarily apply at Health Post level; however, you should be aware of these hazards in case you encounter them elsewhere.
Note also that infectious waste and pathological waste are overlapping categories. Blood, for example, is in both categories. All pathological waste should be considered as potentially infectious. Following the precautionary principle, pathological waste must be handled and disposed of as if it were infectious.
What is the precautionary principle?
In Study Session 2, you learned that if you follow the precautionary principle, this means you take precautions to avoid environmental damage, even if you are not certain that damage will result.
23.2 Public health importance of healthcare waste
Healthcare waste is varied in type and the amount produced is increasing each year. Moreover, if there is little or no segregation of non-hazardous and hazardous waste, it is inevitable that the general waste component will become contaminated and must then be regarded as hazardous.
Everyone in the community is potentially at risk from exposure to healthcare waste, including people within the healthcare establishment and those who may be exposed to it as a result of poor management of the waste.
List all the people who could be at risk from healthcare waste produced at a village Health Post.
Your answer will depend on where your Health Post is and on the local conditions, but your list might include yourself as the Health Extension Practitioner; your patients and people accompanying them; anyone who takes the waste away for disposal; anyone who lives or works close to the disposal place; children who may play in the area and pick up contaminated items.
23.2.1 Hazards from infectious waste
Infectious wastes may contain a variety of pathogenic microorganisms. The route of entry into the body for microorganisms may be through a puncture, abrasion or cut in the skin, possibly caused by sharps contaminated with pathogens. Entry may also be through the mucous membranes (such as eye, mouth or nose), by inhalation, or by ingestion.
There is a particular concern about infection with human immunodeficiency virus (HIV) and hepatitis viruses B (HBV) and C via healthcare waste. These viruses are generally transmitted through needlestick injuries contaminated by human blood. Needlestick injuries are piercing wounds usually caused by the point of a needle but also by other sharp objects. To avoid the risk of HBV, it is recommended that all personnel handling healthcare waste should be immunized. Unfortunately, no vaccine is yet available against hepatitis C.
23.3 Management of hazardous healthcare waste
The aim of healthcare waste management is to contain infectious waste and reduce risks to public health. The steps to achieve this goal include waste minimisation, identification and segregation, recycling, adequate packaging, handling and storage, and proper treatment and disposal.
22.3.1 Waste handling
There are a number of basic guidelines for waste handling. All healthcare waste should be segregated and placed into waste bins by the person generating the waste at the point where waste is generated. All specific healthcare waste segregation, packaging and labelling needs to be explained to the medical and supporting staff. Information should be displayed in charts on the walls of each room. Carts and recyclable containers used for transport of healthcare waste should be disinfected after each use. Sanitary staff and sweepers must wear proper protective clothing at all times when handling infectious waste including face masks, aprons, boots, and heavy duty gloves, as required.
23.3.2 Waste minimisation
Waste minimisation is the first and most important step in any waste management plan. Minimising the amount of waste produced will help the environment by reducing the amount of waste to be disposed of or burned in incinerators, and consequently reduces air pollution. For effective waste minimisation, you should always bear in mind that the materials and supplies purchased should create no or minimal waste. However, it is important to note that minimising waste should never be carried out if it compromises patient care or creates any other risk of infection.
23.3.3 Segregation of healthcare waste
Segregation is the process of separating different categories of waste. Healthcare waste is usually segregated into colour-coded waste bags or bins. This should take place at the source (when the waste is created). You should follow the guidelines for segregation of waste so that the different types of waste are kept separate and each can be handled safely and economically.
Healthcare facilities should provide coloured waste receptacles specifically for each category of waste. The colour-coding system aims to ensure immediate, easy and unambiguous (clear) identification and segregation of the waste which you are handling or going to treat. Based on the type of hazards involved, a different colour code and type of container is assigned and should be used as follows:
- Black: all bins or bags containing non-hazardous healthcare waste.
- Yellow: any kind of container filled with any type of infectious healthcare waste, including yellow safety boxes for sharps.
- Red: any kind of container filled with heavy metal or effluent.
- White: any container or bin filled with drug vials, ampoules or glass bottles for glass recycling or reuse.
You should also note that in a resource-limited Health Post, red containers can be omitted and heavy metals and other effluents can be handled as any other infectious waste using yellow containers. However, please don’t forget that heavy metals and other effluents should not be incinerated (burned) in final disposal sites. The Ethiopian Food, Medicine, Health Professionals Control and Regulatory Authority guidelines should be referred to about the disposal of pharmaceutical wastes. You should be able to obtain these guidelines from your supervisor or district health office.
23.3.4 Recycling and reuse of healthcare waste
What is the difference between reuse and recycling of waste?
Reuse means using the same item again and again without changing its physical form or appearance. Recycling of waste requires processing of some sort, usually in another location, to create a new and different product.
Reuse of some healthcare waste such as glassware is possible but only after cleaning and disinfection. Items should be immersed in a 0.5% chlorine solution for 10 minutes and carefully washed with a brush and soap, rinsed and dried before use. During the disinfection process, you should always protect your hands with appropriate gloves. It is also recommended that you autoclave the glassware at 121oC for at least 30 minutes after washing to ensure complete sterilisation/disinfection (see Section 23.4.1). Only unbroken glassware should be reused; if it is broken it will be sharp waste and must be disposed of.
Materials such as non-contaminated glass and plastic items can be recycled. Recycling may increase the segregation criteria and require more effort on your part because separate containers are needed for materials to be recycled.
23.3.5 Use of safety boxes
You should always collect sharp wastes immediately after use in a safety box. This helps you avoid injuries.
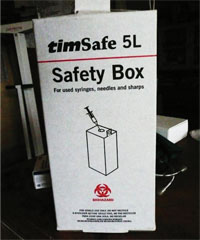
A safety box is used only for sharps (Figure 23.1). It is designed as a puncture- and leak-resistant container for their collection and disposal. The advantage is it confines all sharps in one place and helps prevent reuse. The correct use of safety boxes can prevent needlestick injuries to you and the community. The role of health workers (you) and waste handlers in proper use of safety boxes, starting from assembly through to final disposal, is critical. You should follow these guidelines for effective use of safety boxes:
- Follow the instructions printed on the box.
- Keep safety boxes within your reach at each place where you give injections.
- Dispose of the used syringes into the safety box immediately after use.
- Do not recap and do not collect syringes for future disposal.
- Never place fingers inside the box.
- Stop using the box and close the flap (cover) when it reaches three-quarters full; do not overfill.
- When handling the safety box, always wear gloves.
- Once a safety box contains any sharps, it should be stored in a locked room or cupboard to prevent the public from coming into contact with it.
- Finally, do not forget to wash your hands using antiseptic or hand rub and dry them after using the safety box.
- When the safety box is three-quarters full it should be incinerated (see Section 23.4.2 for further details) and the remains disposed of in a sharps pit (see Section 23.4.4).
23.3.6 Packing healthcare wastes before disposal
Some healthcare wastes need to be placed into special containers or packed up in a particular way before they are transported or disposed of. A safety box for sharps is one example. Liquid infectious wastes need to be placed in capped or tightly stoppered bottles or flasks; large quantities would need a containment tank. Solid or semi-solid wastes should be packed in durable, tear-resistant plastic bags. Special packaging is required for items to be incinerated. These need to be put in combustible containers. Similarly items to be sterilised by steam need containers that allow the passage of steam and air. Clean clothes can be used to wrap items that need to be autoclaved or sterilised.
23.3.7 Waste storage
Some waste may need to be stored carefully onsite until such time as it can be disposed of appropriately. The guidelines for healthcare waste storage that you should follow are:

- A specified place in each room where waste is generated for placing bags, bins or containers.
- Separate central storage facilities for yellow bags should be provided with clear indication that no other materials be stored there.
- No waste shall be stored for more than two days before being treated or disposed of. (This does not include safety boxes, where filled boxes can be kept locked up for up to one week if no onsite incinerator is available.)
- The universal biological hazard symbol (Figure 23.2) should be posted on the storage door and on waste containers.
23.4 Methods of healthcare waste treatment and disposal
23.4.1 Steam sterilisation (autoclaving)
Steam sterilisation is one of the most common methods of treatment of waste. It uses saturated steam within a pressurised vessel called an autoclave (see Figure 23.3) at a temperature that is high enough to kill pathogenic microorganisms. Contaminated items or waste should be sterilised for 30 minutes at 121oC at a pressure of 106 kPa. You should note carefully that the timing should start only after it has reached the necessary temperature and pressure.
kPa is the abbreviation of kiloPascal, a unit of pressure.

23.4.2 Incineration
Incinerators convert combustible materials into ashes or residues. Gases are ventilated through the chimney stack into the outer air. If the incinerator is properly designed, maintained and operated, it serves the purpose of destroying infectious microorganisms in the waste.
You may remember from Study Session 22 that, in the context of waste management, incineration means more than just burning. It means controlled and managed burning, usually at high temperature. A waste incinerator needs to reach very high temperatures in order to completely destroy needles and syringes. This type of high temperature incinerator is unlikely to be available to you but other options for burning can be used at Health Post level. With the help of others in your community, you may be able to build a low temperature incinerator, also known as a protected hearth, like the one shown in Figure 23.4.

If a brick-built incinerator is not available, you may be able to burn the waste in a converted metal drum or barrel. To do this, you will need a metal drum with both ends removed to make a cylindrical container. You will also need four bricks and two rigid metal screens that are large enough to cover the open ends of the drum. You will need to place the drum in a fenced area away from the Health Post buildings. Place the bricks on the ground, with spaces between them and a metal screen or grate on top. Place the open base of the drum on the metal screen and put another screen on top. The metal screens are to allow air to flow around the burning waste so the fire gets hotter, and to reduce the amount of ashes flying out of the top. Put the safety box or other waste with some paper, dry leaves, or small sticks into the drum and sprinkle them with a small amount of kerosene (if available). Put paper under the drum, between the bricks, and set light to it so the flames rise through the metal screen.
If there are no incinerators, then open pit burning is also possible, and frequently used in rural Health Posts (Figure 23.5). The pit must be protected with a fence to prevent people or animals from gaining access to it. It is advisable to watch the fire until everything is burned to be sure that no waste is blown around by the wind or left unburned. The ash or residue must be buried for final disposal.

23.4.3 Chemical or high-level disinfection (HLD)
Chemical disinfection, also known as high-level disinfection (HLD), is the preferred treatment for liquid infectious wastes. It can also be used for solid infectious waste treatment. The chemical disinfectants are hazardous to skin and mucous membranes, and it should not be applied without wearing gloves and goggles. Chlorine and glutaraldehyde are the best chemical disinfectants; the most appropriate being 0.5% chlorine solution for 10 minutes. The ultimate disposal of chemical waste must safeguard users, the community and the environment. It should be disposed of into a seepage pit and the bottom of the pit should be not less than 3 m from the water table in order to prevent contamination of the groundwater.
Training on handling techniques of chemical disinfection should be provided for persons involved in healthcare waste treatment to minimise personal exposure of hazards and handling of sterilised materials.
23.4.4 Final disposal: burial pits
Burial pits are acceptable for some wastes but ideally, there should be separate pits for general healthcare wastes and for hazardous healthcare waste. The general waste could be transported to community refuse pits, if there are any. Burial pits for hazardous waste should be properly fenced to prevent access by people or animals. They should not be used, however, in areas with a high groundwater table. The bottom of the pit should be at least 1.5 m higher than the groundwater table for disposal of solid waste. You should make sure that the final disposal of hazardous waste by reputable waste handlers is performed according to applicable federal and local regulations.
Sharps pit
A sharps pit is a particular type of burial pit that should be used only for the final disposal of needles and other sharps. Safety boxes should be incinerated to sterilise the contents before carefully collecting the residue for disposal in the sharps pit. A properly constructed sharps pit should have a cover at the surface and be lined with cement to make it watertight in order to avoid contamination of groundwater and soil. It must have a fence around it. For a Health Post, the pit need not be large and can take many years to fill.
23.4.5 Anatomical waste and placentas
The visual impact of anatomical wastes (especially for observable body parts) is very sensitive and may alarm the general public. The wastes are also a health hazard. Therefore, it is mandatory to properly contain anatomical wastes based on the local custom or cultures of your society. Special care and sensitivity is needed when considering the appropriate disposal of fetuses from stillbirths. You should make sure, while considering the local contexts, that the method you choose should not contaminate the environment.
Anatomical waste and placentas need a special placenta pit. The placenta pit should also be used for blood, vomit and other bodily secretions. This burial pit should be sited inside the Health Post compound and dug down to at least 1 m deep. The pit should be fenced and locked. The waste should be collected in a plastic or galvanised metal container with a tight-fitting cover and immediately transported to the pit using dedicated trolleys or carts. The waste should be covered with a layer of soil immediately after disposal into the pit.
Due to cultural conditions, and the low temperature incinerators present in Health Posts, you should avoid using incinerators for anatomical waste. You should wear heavy-duty gloves while handling and transporting the waste. Wash and dry the gloves after use.
23.5 Prevention and control of risks to healthcare workers
All healthcare workers, including the waste handlers and maintenance workers, should be instructed to use personal protective equipment (PPE) such as gloves while working in contaminated areas and with contaminated materials, and to wash their hands thoroughly after removing the gloves. The workers should be aware of the fact that other people may not have followed the correct procedures while disposing of gloves, blades or needles; therefore, they need to be careful when handling all healthcare waste bags and containers.
People working in healthcare facilities may get accidental injuries because they are in a hurry to help their patients, or in an emergency, or simply due to ignorance or not being able to practise what they know. The following guidelines should be followed for the prevention and control of risks to healthcare workers:
- Keep desks and countertops free from sharps.
- Discard needles and other sharps into safety boxes, never into waste bins or plastic bags.
- Never try to recap needles (i.e. use once and dispose of immediately).
- Regularly review the rules for safe disposal and collection of sharps or other hazardous materials.
- You (or any healthcare worker) should always examine and handle soiled linens and similar items as if they were hazardous.
- Workers should receive periodic instruction at least once a year to keep them aware of the specific hazards of healthcare waste.
- Workers should take appropriate measures to limit further contagion from waste by practising universal precautions of self-protection from exposure to infectious wastes.
23.6 Planning and monitoring healthcare waste management
Managing the safe and proper disposal of healthcare waste is an essential part of infection protection and control for you (the healthcare worker), your clients/patients and the general public. In addition to meeting national and local guidelines on infection prevention, it helps you prevent nosocomial infections (i.e. healthcare facility/hospital acquired diseases).
Planning and preparation for proper waste disposal will help you ensure the availability and correct functioning of infection control facilities in the Health Post, including sanitising materials and hazardous healthcare waste management and disposal equipment. Forward planning can also help reduce the likelihood of accidents; for example, the chance of needlestick injury will be reduced if you always think ahead and have the sharps box close to you when you give an injection.
Table 23.1 is a template for waste management planning in the Health Post. It lists various waste management activities and indicates how often they should be done, the materials and equipment needed and who is responsible. You may wish to adapt this for your own Health Post and draw up your own management plan. Having a plan similar to this will help to ensure that waste is managed correctly.
| Activity | When? | Equipment/materials needed | Who? | Comments |
|---|---|---|---|---|
| Handwashing | R, BP and AP | Water, soap, disinfectant/alcohol | Health Extension Practitioner | Sullage should be disposed of into a seepage pit |
| Disposing of sharps | R (when the safety box gets ¾ filled), AP | Safety box, incinerator, sharps pit | Health Extension Practitioner | Avoid needle recapping |
| Disposing general waste and solid infectious waste | R | Waste bin, incinerator, gloves, matches, burial pit | Health Extension Practitioner and others | Incinerate in a brick incinerator, or metal drum or burn in an open pit |
| Inspecting waste disposal facilities | O | Heavy-duty gloves, protective clothes | Health Extension Practitioner | |
| Sterilisation of instruments/materials | AP | Autoclave, indicator | Health Extension Practitioner | An indicator is a strip or tape that changes colour when the material/equipment reaches sterilising temperature |
| Disposal of liquid/semi-liquid infectious waste | AP | Placenta pit | Health Extension Practitioner | Pit should be fenced and locked |
| Disposal of expired drugs | O | List of drugs expired, reporting, disposal pit | Committee from district office, kebele and Health Extension Practitioner | You need to notify the committee if you have drugs that need to be disposed of |
| Cleaning the Health Post | R | Water, detergents, disinfectants, gloves, protective clothing, broom, mops, dustbin, etc. | Health Extension Practitioner and others |
You can monitor the management of healthcare waste at your Health Post and identify possible improvements that you could make by checking your current practices. For example:
Could you reduce the amount of waste produced in your Health Post (waste minimisation)?
Do you separate infectious from non-infectious waste?
Is infectious waste packaged before disposal to reduce contact and exposure?
Do you have adequate supplies of gloves, colour-coded bins and other waste management supplies?
Is everyone at the Health Post properly trained in correct healthcare waste management procedures?
There may be other questions you can think of to include on your checklist.
Concluding note
We have now reached the end of the Hygiene and Environmental Health Module. In these 23 study sessions, you have been learning about personal and environmental hygiene, how to keep food hygienic, about the provision, use and treatment of safe water, and how to manage wastes in the household, community and healthcare facility.
As you know, poor hygienic and environmental health conditions are the major cause of illness and death in Ethiopia and other developing countries. It is our sincere hope that this Module, along with other Modules in this curriculum, will enable you to understand the concepts and principles of hygiene and environmental health. By putting these concepts and principles into practice, your community disease profile will improve significantly to a level that common infectious diseases that arise due to poor hygiene and environmental health, such as diarrhoea, intestinal parasites, malaria, pneumonia and TB, will not be major causes of morbidity or mortality in your area. Moreover, as well as learning about the protection of human health, you have also learned how to keep our environment safe.
Summary of Study Session 23
In Study Session 23, you have learned that:
- Healthcare waste is any waste produced in a healthcare facilty and is also known as medical waste, hospital waste or infectious waste. It includes hazardous and non-hazardous waste.
- Health hazards from pathogens are the major concern in waste from Health Posts.
- Waste minimisation is the first and most important step in healthcare waste management.
- Healthcare waste must be segregated into different categories and colour-coded containers used for storage.
- Safety boxes are important devices for safe collection of sharps. A sharps pit is also required for final disposal.
- Personnel involved in handling and storage of healthcare waste should be trained in correct procedures and provided with the necessary PPE to protect their health.
- Autoclaving, incineration, placenta/burial pit and HLD using chemicals are the most commonly used final disposal methods.
Self-Assessment Questions (SAQs) for Study Session 23
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 23.1 (tests Learning Outcome 23.1)
Which of the following statements is false? In each case, explain why it is incorrect.
A Healthcare waste contains hazardous and non-hazardous waste.
B Infectious healthcare waste is kept in red containers.
C Chemical disinfection involves treating waste with 0.5% chlorine solution for 10 minutes by immersing in an autoclave.
Answer
A is true. Healthcare waste does contain both hazardous and non-hazardous waste,
B is false. Infectious waste should be stored in a yellow container.
C is false. Chemical disinfection does involve treatment with chlorine solution of 0.5% concentration for 10 minutes but an autoclave is a steam sterilising device that relies on temperature to disinfect.
SAQ 23.2 (tests Learning Outcome 23.2)
Which items in the list below are classed as pathological waste?
Syringes, used swab, placenta, used gauze, expired drugs, body parts, paper packaging, blood.
Answer
Placenta, body parts and blood are all pathological wastes.
SAQ 23.3 (tests Learning Outcomes 23.3)
Gadissa, a local farmer, had an accident last week while working in his fields and cut his leg. He came to the Health Post immediately afterwards and you treated the wound with a dressing and bandage. Today he is returning to the Health Post to have the dressing changed. What should you do before examining his wound? What should you do with the used dressing?
Answer
You should wash your hands thoroughly before removing the old bandage. You may also want to put on gloves. Pick up a sterilised set of instruments, such as scissors, to remove the dressing. You may find the used dressing is blood-stained. It should be handled in the same way as infectious waste because, although Gadissa may be perfectly healthy, all waste that has been in contact with body fluids should be considered to be potentially infectious. You should immediately place the used dressing in a yellow waste container or bag. Keep the container tightly closed. At the end of the day, you should dispose of the container in an incinerator, if available, or burn it in the refuse pit before you leave the Health Post.
Read Case Study 23.1 and then answer the questions that follow it.
Case Study 23.1 A story of a busy rural Health Post
Hirut, a Health Extension Practitioner in Robit rural kebele, is working in a Health Post. One busy day, the Health Post was full of clients for family planning, children who need immunization, and children having diarrhoeal problems. Hirut started her day by giving health education for mothers on the importance of family planning, hygiene and environmental sanitation. Her workmate, Almaz, was preparing the schedule for their subsequent activities. Because of the workload, the Health Extension Practitioners could not go home for lunch on time. They were too exhausted. At this time, Hirut was giving an injection of Dipo Provera to a woman. She accidentally pricked her finger with the used needle while trying to recap it.
SAQ 23.4 (tests Learning Outcome 23.3 and 23.4)
What did Hirut do that was procedurally wrong? What should she have done?
Answer
Hirut should not have tried to recap the needle. She should have put it in to the safety box immediately.