Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Friday, 19 April 2024, 12:41 PM
Labour Delivery and Care Module: 1. Recognition of Normal Labour
Study Session 1 Recognition of Normal Labour
Introduction
Ideally the same health professional will look after the pregnant woman and her baby from the first antenatal visit until the end of the postnatal period. This is known as the continuum of care. You have already studied the Module on Antenatal Care. Now you are moving on to learn about Labour and Delivery Care. Labour is the term for the changes in anatomy and physiology in the female reproductive tract that prepare the fetus and the placenta for delivery. In the majority of cases, this happens when the baby is fully developed at full term, between 37-40 weeks gestation. Labour heralds the end of the baby’s time in the uterus and the beginning of adaptation to life outside the mother.
This first study session serves as an introduction to the Labour and Delivery Care Module. The emphasis is on helping you make the diagnosis of true labour and distinguishing it from false labour, and recognising the signs of the four stages of labour. This session will help you to understand the labour and delivery process, so that you can make accurate decisions and feel confident when you attend births. You will also learn how to prepare the pregnant woman to become aware of the changes in her body that indicate labour will start soon, and how to recognise the onset of true labour, so she can send for you to come in good time.
Learning Outcomes for Study Session 1
When you have studied this session, you should be able to:
1.1 Define and use correctly all of the key terms printed in bold. (SAQ 1.1, 1.2, 1.3 and 1.4)
1.2 Describe the signs of true labour and distinguish between true and false labour. (SAQs 1.2 and 1.3)
1.3 Explain to the mother how to recognise the onset of true labour. (SAQ 1.2)
1.4 Describe the characteristic features and mechanisms of the four stages of labour. (SAQ 1.4)
1.5 Describe the seven cardinal movements made by the baby as it descends the birth canal in a normal labour. (SAQ 1.4)
1.1 The indefinite nature of labour
You need to be aware that labour may start at any time. This is one of its ‘indefinite’ features, so you should always be ready to take appropriate action. Despite much advancement of maternal and fetal health sciences, so far nobody knows exactly:
- When is labour going to start?
That is why even the normal onset of labour is anticipated in a wide range of weeks (at Health Post level 37–40 weeks is considered the normal ‘window’; at hospital level, it can be at 37–42 weeks with close follow up using ultrasound scanning). Although it is good to calculate the expected date of delivery as 40 weeks from the mother’s last normal menstrual period (LNMP), if she knows the date (many mothers do not), tell her that she is probably not going to deliver on the expected date. Only about 2% of deliveries occur on the expected date even among women who know their LNMP date exactly. The other major indefinite features of labour are:
- What initiates/stimulates labour to begin? Is it factors in the fetus, the mother or both?
- Why do some women develop preterm labour?
- Why do unpredicted labour abnormalities occur?
We have to leave these questions unanswered, and focus on the normal labour occurring at term.
1.1.1 Normal labour
A normal labour has the following characteristics:
- Spontaneous onset (it begins on its own, without medical intervention)
- Rhythmic and regular uterine contractions
- Vertex presentation (the ‘crown’ of the baby’s head is presented to the opening cervix, as you learned in Study Session 6 of the Antenatal Care Module)
- Vaginal delivery occurs without active intervention in less than 12 hours for a multigravida mother and less than 18 hours for a primigravida (first birth)
- No maternal or fetal complications.
Any type of labour that deviates from these conditions is considered abnormal, and usually requires referral for specialist care. You will learn how to deal with different types of abnormal labour later in this Module in Study Sessions 8-11. Next, we describe the signs that tell you and the mother that true labour has begun.
1.2 How do you know that true labour has begun?
True labour is characterised by regular, rhythmic and strong uterine contractions that will increase progressively and cannot be abolished by anti-pain medication. Pain symptoms may be relieved a little if the woman takes painkilling drugs, but true labour will still progress.
1.2.1 What is adequate uterine contraction?
If true labour is progressing, there will be adequate uterine contraction, evaluated on the basis of three features — the frequency, the duration and the intensity of the contractions:
- The frequency of uterine contractions will be 3-5 times in every 10 minute period.
- Each contraction lasts 40–60 seconds; this is known as the duration of contractions.
- The woman tells you that her contractions feel strong; this is the intensity of contractions.
You can assess the strength of uterine contractions for yourself by palpating the woman’s abdomen in the area of the fundus (top) of the uterus. In between contractions, when the uterus is relaxed and the muscular wall is soft, you will be able to palpate the fetal parts. But when a strong contraction comes, you will not be able to feel the fetal parts, because the abdominal wall over the uterus is very tense and very painful if you apply deep pressure with your fingers.
In Study Session 4, you will learn how to record the frequency, duration and intensity of contractions on a chart called the partograph.

1.2.2 Show and leakage of amniotic fluid
During most of the pregnancy, the tiny opening in the cervix is plugged with mucus. In the last few days of pregnancy, the cervix may begin to open. Sometimes the mucus and a little bit of blood drip out of the vagina. This is called show. It may come out all at once, like a plug, or it may leak slowly for several days. When you see the show, you know that the cervix is softening, thinning and beginning to efface (open). Be careful not to confuse the show with the normal discharge (wetness from the vagina) that many women have in the two weeks before labour begins. That discharge is mostly clear mucus and is not coloured a little bit red with blood.
True labour may be spontaneously established with or without show and with or without leakage of amniotic fluid (the waters in the fetal membranes surrounding the baby). In many parts of Ethiopia, people think that labour is not progressing if they don’t see leakage of amniotic fluid either before or after labour begins. This is not true. You should be clear that show and leakage of amniotic fluid are not required for labour to begin or progress.
![]() If labour has not started or not progressed much within 6 hours after the waters break, refer the woman to a higher health facility as soon as possible.
If labour has not started or not progressed much within 6 hours after the waters break, refer the woman to a higher health facility as soon as possible.
When the bag of waters breaks (fetal membranes rupture), there can be a big gush of amniotic fluid from the vagina, or a slow leak. In most women, the bag of waters normally breaks during early labour. If the fetal membranes rupture before labour begins, there should only be a few hours delay before labour starts. If labour does not start within 6 hours after the bag of waters breaks, there is a risk of infection entering the uterus, which gets stronger the more time that goes by after the membranes rupture. You learned about premature rupture of membranes (or PROM) in Study Session 17 of the Antenatal Care Module. Remember that ‘premature’ refers to the fetal membranes rupturing ‘early’ (before labour starts) – not to the gestational age of the baby, which may be preterm, term or post-term when the waters break.
However, even if the fetal membranes break after labour begins, as is normally the case, there are some risks associated with the leakage of amniotic fluid that you should be aware of.
Think back to what you already learned about PROM. Can you suggest what risks might occur if the waters break while the woman is already in labour?
Potential complications of rupture of fetal membranes during labour are:
- Infection: Since the ‘door’ to the uterus is open and you are going to do pelvic examinations with your gloved fingers to assess the progress of labour, there is a risk of transferring infection into the uterus unless you are very careful about hygiene (as you will learn in later study sessions of this Module). This risk gets bigger if the labour is prolonged.
- The umbilical cord may prolapse (be pushed out ahead of the baby as the waters gush out through the cervix), or the cord may become trapped against the endometrial wall by the baby which is no longer kept ‘floating’ by the amniotic fluid. If the cord is compressed, the baby can develop hypoxia (low oxygen levels) because the blood flow is restricted in the cord, and it may die or be brain damaged.
1.2.3 Distinguishing true labour from false labour
There is a condition termed false labour, which may be felt one or two weeks ahead of true labour. It is characterised by irregular contractions which are less painful than in true labour and they don’t progress. Table 1.1 contrasts the characteristics of true and false labour. When a woman has a false labour, she should not be discouraged. Tell her that although she is not yet in true labour, the signs she is experiencing mean that her labour will start soon. Advise her on the signs of true labour (Table 1.1 and the next section) and tell her to call you or to come to the Health Post when the signs of true labour appear.
| Characteristics | True labour | False labour |
|---|---|---|
| Uterine contractions | Contractions occur at regular intervals, but the interval between each contraction gradually becomes shorter | Contractions occur at irregular intervals |
| Duration of each contraction gradually increases | Duration remains unchanged — either long or short | |
| Intensity of contractions becomes stronger and stronger | Intensity remains unchanged | |
| Cervical dilation | Cervix progressively dilates | Cervix does not dilate, remains less than 2 cm |
| Pain | Discomfort at the back in the abdomen, cannot be stopped by strong anti-pain medication | Discomfort is non-specific (has no particular location) and is usually relieved by strong anti-pain medication or by walking |
1.2.4 Helping the mother recognise a true labour

There is no way to be sure when a woman’s labour will begin, but there are some signs that it will start soon. Babies often drop lower in the mother’s belly about 2 weeks before birth, which is known as lightening; commonly, mothers feel that the baby is no longer lying ‘high’ in the abdomen, and not pushing her stomach upwards. If she has had babies before, this baby may not drop until labour begins.
Other signs may happen only a day or two before labour starts. The mother’s stool may change, or a little show (bloody mucus) may come out of the vagina. Sometimes, the bag of waters leaks or breaks (premature rupture of fetal membranes — PROM) before labour begins.
Recognising true labour isn’t an easy task for the mother, particularly if this is her first baby. She may come repeatedly to the Health Post or call for you, assuming that minor complaints are the start of true labour. Counselling the mother and her family on birth preparedness is part of focused antenatal care (as you learned in Study Session 13 of the Antenatal Care Module). When you counsel her on how to recognise true labour and what actions to take, make sure you use simple and easily understandable language and clearly demonstrate what she will feel on her abdomen. Your role is very important, first to minimise the mother’s anxiety about the labour, and second to reduce her unnecessary costs and time spent visiting the health facility for false labour or minor complaints.
Tell her that true labour is:
- Regularly and progressively increasing pushing-down pain, which happens about 3–5 times in every 10 minutes. (Check whether she knows or can estimate how long 10 minutes is).
- Characterised by a pushing down pain, which is usually felt first in her lower back and moving around to the front in the lower abdomen below her belly button.
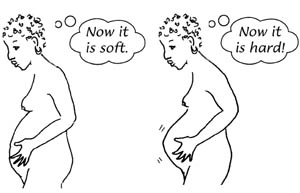
Demonstrate on her abdomen:
- What will happen due to lightening
- Where she will feel the abdomen is hard during contractions
- Where she will feel the maximum pushing-down pain.
1.3 Stages of labour
In this section, you will learn some basic introductory information about the stages of labour and birth. Each stage will be discussed in more detail in subsequent study sessions in this Module. Labour is traditionally divided into four stages:
- The first stage of labour (the cervical opening stage)
- The second stage of labour (the pushing stage, ending in the birth of the baby)
- The third stage of labour (the birth of the placenta)
- The fourth stage of labour (the first 4 hours after birth).
1.3.1 First stage of labour
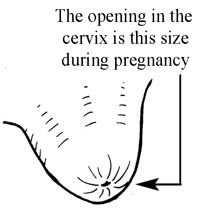
The first stage of labour is characterised by progressive opening of the cervix, which dilates enough to let the baby out of the uterus. For most of the pregnancy, nothing can get in or out of the cervix, because the tiny opening in it is plugged with mucus.
During pregnancy the cervix is long and firm, like a big toe (see Figure 1.1a), but the immediate effect of uterine contraction is to dilate the cervix and shorten the lower segment of the uterus, so the edges of the cervix are gradually drawn back and are taken up. This process is called effacement (Figure 1.1b and c).

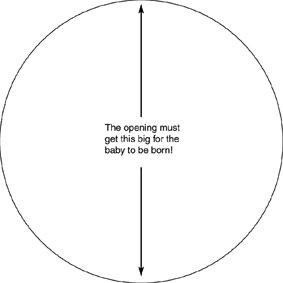
The cervix then dilates (the diameter gradually increases) – this is known as cervical dilatation. Each time the uterus contracts, it pulls a little bit of the cervix up and open. Between contractions, the cervix relaxes. The first stage is divided into two phases: the latent and the active phase, based on how much the cervix has dilated.
Latent phase
The latent phase is the period between the start of regular rhythmic contractions up to cervical dilatation of 4 cm. During this phase, contractions may or may not be very painful, and the cervix dilates very slowly. The latent phase ends when the rate at which the cervix is dilating speeds up (it dilates more quickly). This signals the start of the active phase.
Active phase

The active phase is said to be when the cervix is greater than 4 cm dilated. Contractions become regular, frequent and usually painful. The rate of cervical dilation becomes faster and it may increase in diameter by as much as 1.2 to 1.5 cm per hour, but the minimum dilation rate should be at least 1 cm per hour. You should start to plot data on the partograph at this stage, as you will learn to do in Study Session 4 of this Module.
Cervical dilatation continues until the cervix is completely open: a diameter of 10 cm is called fully dilated. This is wide enough for the baby to pass through (Figure 1.2). At this diameter, you would not feel the cervix over the fetal head when you make a vaginal examination with your gloved fingers. (We will describe how to do this later in this Module and you will be shown how to do it in your practical training sessions.)
1.3.2 Second stage of labour
The second stage begins when the cervix is fully dilated (10 cm) and is completed when the baby is completely born. After the cervix is fully dilated, the mother typically has the urge to push. Her efforts in ‘bearing down’ with the contractions of the uterus move the baby out through the cervix and down the vagina. This is known as fetal descent. The rate of fetal descent is an important indicator of the progress of labour, which will be described in more detail later. The average duration of second stage is 1 hour and usually not longer than 2 hours. Table 1.2 summarises the symptoms and signs during the first and second stages of normal labour.
| Symptoms and signs | Stage | Phase |
|---|---|---|
Cervix not dilated Uterine contractions not regular or strong | False labour/Not in labour | |
Regular uterine contraction but not very strong Cervix dilated less than 4 cm | First | Latent |
Regular and strong uterine contractions Cervix dilated 4–9 cm Rate of dilatation typically 1 cm per hour or faster Fetal descent begins | First | Active |
Cervix fully dilated (10 cm) Fetal descent continues Mother has no urge to push | Second | Early (non-expulsive) |
Cervix fully dilated (10 cm) Presenting part of fetus reaches pelvic floor Mother has the urge to push | Second | Late (expulsive) |
The delivery of the baby marks the end of the second stage.
1.3.3 Third stage of labour
The third stage of labour is the delivery of the placenta and membranes after the baby has been born. The duration is usually a maximum of 30 minutes. (You will learn more about this stage in Study Session 6 of this Module.)
1.3.4 Fourth stage of labour
The first four hours immediately following placental delivery are critical, and have been designated by some experts as the fourth stage of labour. This is because after the delivery of the placenta, the woman can have torrential vaginal bleeding due to failure of uterine contractions to close off the torn blood vessels where the placenta detached from the uterine wall. Therefore, you should be vigilant to detect revealed or concealed postpartum haemorrhage and manage it accordingly. (You will learn about this in detail in Study Session 11 of this Module).
The placenta, membranes and umbilical cord should be examined for completeness and for abnormalities (Study Session 6 covers this). Maternal blood pressure and pulse should be recorded immediately after delivery and every 15 minutes for the first four hours. Normally, after the delivery of the placenta, the uterus will become firm due to sustained contraction, so the woman might feel strong contractions after the birth. Reassure her that these contractions are healthy, and help to stop the bleeding.
1.4 Mechanisms of normal labour
The seven cardinal movements are the series of positional changes made by the baby which assist its passage through the birth canal. (Cardinal means ‘fundamentally important’.) The position before the movements begin is shown in Figure 1.3 (diagram 1) and the seven movements are in diagrams 2 to 8. As you read the descriptions that follow, keep looking at Figure 1.3.

The positional changes made by the baby are specific, deliberate and precise. They allow the smallest diameter of the baby to pass through the mother's pelvic cavity. Neither you nor the mother is responsible for these positional changes. The baby has the responsibility for the seven cardinal movements.
1.4.1 Engagement
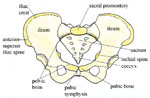
Engagement is when the fetal head enters into the pelvic inlet (Figure 1.3, diagram 2). The head is said to be engaged when the biparietal diameter (measuring ear tip to ear tip across the top of the babys head, see Figure 1.4 below) descends into the pelvic inlet, and the occiput is at the level of the ischial spines in the mother’s pelvis (see Figure 1.5).

1.4.2 Descent
The term fetal descent is used to describe the progressive downward movement of the fetal presenting part (commonly the head) through the pelvis. When there is regular and strong uterine contraction, and the size of the babys’ head and the size of the mother’s pelvic cavity are in proportion so the baby can pass through, there will be continuous fetal descent deep into the pelvic cavity. Since the pelvic cavity is enclosed with pelvic bones, when the uterus is strongly pushing down, occasionally the fetal scalp bones undergo overlapping at the suture lines in order to allow the head to pass through the narrow space. This overlapping is called moulding. The commonest types of moulding include one parietal bone overlapping over the other parietal bone along the sagittal suture (Figure 1.4), the occipital bone overlapping the temporal bone, and the frontal bone overlapping the parietal bones.
1.4.3 Flexion
The movement known as flexion occurs during descent and is brought about by the resistance felt by the baby’s head against the soft tissues and bones of the mother’s pelvis. The resistance brings about a flexion in the baby’s head so that the chin meets the chest (Figure 1.3, diagram 2). The smallest diameter of the baby’s head presents into the pelvis.
1.4.4 Internal rotation
You can see the diameters of the pelvic inlet and outlet if you look back to Figures 6.3 and 6.4 in the Antenatal Care Module, Part 1.
As the head reaches the pelvic floor, it typically rotates to accommodate the change in diameters of the pelvis (Figure 1.3, diagram 3). At the pelvic inlet, the diameter of the pelvis is widest from right to left. At the pelvic outlet, the diameter is widest from front to back. So the baby must rotate from lying sideways to turning its face towards the mother’s backbone (Figure 1.3, diagram 4). When the rotation is complete, the back of the baby’s head is against the front of the mother’s pelvis). The sagittal suture in the fetal skull is no longer at an angle, but points straight down towards the mother’s backbone. This movement is called internal rotation because it occurs while the baby is still completely inside the mother.
1.4.5 Extension
After internal rotation is complete, the baby’s head passes through the pelvis and a short rest occurs when the baby’s neck is under the mother’s pubic arch. Then extension of the baby’s head and neck occur – the neck extends, so the chin is no longer pressed against the baby’s chest, and the top of the head, face and chin are born (Figure 1.3, diagrams 4 and 5).
1.4.6 External rotation (restitution)
After the head of the baby is born, there is a slight pause in the action of labour. During this pause, the baby must rotate so that his/her face moves from facing the mother’s backbone to facing either of her inner thighs (Figure 1.3, diagram 6). This movement is called external rotation because part of the baby is already outside the mother (it is also called restitution). The rotation is necessary as the baby’s shoulders must fit around and under the mother’s pubic bone.
1.4.7 Expulsion
Almost immediately after external rotation, the anterior (foremost) shoulder moves out from under the pubic bone (Figure 1.3, diagram 7). The mother’s perineum becomes distended by the posterior (second) shoulder, which is then also born (Figure 1.3, diagram 8). The rest of the baby’s body is then born (expulsion), with an upward motion of the baby’s body assisted by the care provider.
1.4.8 In conclusion
Note that at every stage of labour there is descent. To be specific, after the fetal head undergoes flexion, there is descent; after internal rotation, there is descent; after extension, there is descent and so on. In the next study session, we will describe the progress of a normal labour in more detail.
Summary of Study Session 1
In Study Session 1 you have learned that:
- True labour is a natural process characterised by regular, rhythmic and strong uterine contractions that will increase progressively and produce cervical effacement and dilatation.
- True labour can begin without a show and without the waters breaking (rupture of fetal membranes).
- A woman in a state of false labour has uterine contraction of irregular intervals and intensity that can be relieved by anti-pain medication.
- The woman herself can recognise true labour if you let her know that it is manifested by pushing down pains occurring 3–5 times in every 10 minutes, each contraction lasting 40–60 seconds.
- There are four stages of labour:
- The first stage starts with true labour and ends with full cervical dilatation (10 cm); it is divided into latent and active phases.
- The second stage is from full cervical dilatation to delivery of the baby.
- The third stage is from the delivery of the baby to delivery of the placenta.
- The fourth stage is the first 4 hours after placental delivery when you need to follow the mother as closely as during labour and delivery.
- In a normally progressing labour, the baby performs seven cardinal movements as it passes down the birth canal: engagement - descent - flexion - internal rotation - extension - external rotation/restitution - expulsion.
- There is fetal descent during every cardinal movement.
- Moulding of the baby’s skull may occur as it passes through the mother’s pelvis, under pressure from the contractions pushing it through the narrow space.
Self-Assessment Questions (SAQs) for Study Session 1
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the questions below. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 1.1 (tests Learning Outcome 1.1)
Write each of the bold terms listed below on a small piece of paper. Roll up each piece and put them in a small basket or bowl.
Pick one at a time and try to define the term. Write your answers in your Study Diary. Finally, compare your answers with the definitions in this study session. You can repeat the exercise until you are familiar with all of the words.
true labour, effacement , dilatation, presenting part, show, rupture of fetal membranes, engagement, descent, first stage, second stage, third stage, fourth stage
Answer
Check your definitions of the bold terms by finding each of them in Study Session 1 and comparing what you have written in your Study Diary with our definition in this session. If any of your definitions were different from ours, try Activity 1.1 again until you get all of them right.
Read Case Study 1.1 and then answer the questions that follow it.
Case Study 1.1 Mrs Abeba
Mrs. Abeba is 30 years of age and is having her first baby. She has come to the Health Post because she began to get regular pushing-down pains about 3 hours ago. She says that the pains start in her back and move forward to the front of her abdomen, each pain lasts about 40 seconds, and they occur 2–3 times in every 8 minutes. When you examine her, you find that her cervix is fully effaced and the diameter is 4 cm. Mrs Abeba’s mother-in-law has told her she isn’t in labour because she hasn’t had a ‘show’.
SAQ 1.2 (tests Learning Outcomes 1.2 and 1.3)
- a.What are the signs suggesting true labour from Mrs Abeba’s description and the physical examination?
- b.What stage of labour has she reached and how do you know this?
- c.What will you say to Mrs Abeba to help her recognise that she is really in labour?
Answer
- a.Mrs Abeba is in true labour because her pains are signs of adequate uterine contractions: they are regular, frequent (2-3 every 8 minutes), and the duration is about 40 seconds, which is expected in true labour. Her cervix is effaced and dilated to 4 cm after 3 hours of contractions.
- b.She is in the first stage of labour, at the cross-over point between the latent phase and the active phase, which occurs when the cervix is dilated to 4 cm.
- c.Reassure Mrs Abeba that labour can begin normally without a ‘show’. Her contractions have been coming for 3 hours without stopping, and their strength and regularity are as expecedt in a normal labour.
SAQ 1.3 (tests Learning Outcomes 1.2)
Table 1.3 summarises the difference between true and false labour. Fill in the empty boxes with appropriate descriptions.
| True labour | False labour |
|---|---|
| Contractions occur at regular intervals | |
| Duration of each contraction gradually increases | |
| Intensity of contractions is unchanged | |
| cervix progressively dilates | |
| Discomfort usually relieved by anti-pain medication or with walking |
Answer
The completed version of Table 1.3 is shown below.
| True labour | False labour |
|---|---|
| Contractions occur at regular intervals | Contractions occur at irregular intervals. |
| Duration of each contraction gradually increases | Duration remains unchanged – either long or short |
| Intensity of contractions becomes stronger and stronger | Intensity remains unchanged |
| Cervix progressively dilates | Cervix does not dilate |
| Discomfort cannot be stopped by strong anti-pain medication | Discomfort usually relieved by anti-pain medication or by walking |
SAQ 1.4 (tests Learning Outcomes 1.1, 1.4 and 1.5)
Which of the following statements is false? In each case, explain what is incorrect.
A Lightening is when the baby floats higher in the abdomen shortly before labour begins.
B The second stage of labour ends with the expulsion of the baby from the birth canal.
C The fourth stage of labour lasts for 4 hours and begins when the placenta and fetal membranes have been expelled.
D The overlapping of fetal skull bones during the descent through the mother’s pelvis is called flexion.
E The fetal head is engaged when the occiput of the fetal skull reaches the level of the ischial spines in the mother’s pelvis.
F During a normal birth, both the baby’s shoulders are born at the same time.
Answer
A is false. Lightening is when the baby drops lower in the abdomen before labour begins.
B is true. The second stage of labour ends with the expulsion of the baby from the birth canal.
C is true. The fourth stage of labour lasts for 4 hours and begins when the placenta and fetal membranes have been expelled.
D is false. The overlapping of fetal skull bones during the descent through the mother’s pelvis is called moulding (not flexion).
E is true. The fetal head is engaged when the occiput of the fetal skull reaches the level of the ischial spines in the mother’s pelvis.
F is false. During a normal birth, one of the baby’s shoulders is born first, followed by the other shoulder.