Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Thursday, 18 April 2024, 5:34 AM
Non-Communicable Diseases, Emergency Care and Mental Health Module: 9. Introduction to Mental Health
Study Session 9 Introduction to Mental Health
Introduction
Mental illness is more common than most people realise and in this session you will learn why there is ‘no health without mental health’. We will review what is known about how many people are affected by mental illness in Ethiopia. You will learn that mental illness can lead to a high level of disability and suffering, often over a long period of time. Not only that, but people suffering from mental illness also have poorer general health and higher mortality, and are often victims of stigma, discrimination and abuse. Mental health is also important for achieving many of the Millennium Development Goals.
You will learn that, even though effective treatments are available, few people with mental illness receive the care they need. As a health practitioner, you have an important part to play in helping to reduce this treatment gap. We will describe how mental healthcare fits into all levels of the existing health system and your expected role in the health extension service. Finally, you will learn about the multiple causes of mental illness, the ‘biopsychosocial model’ of mental health and some of the different ways that mental illness is understood within the local culture.
Learning Outcomes for Study Session 9
When you have studied this session, you should be able to:
9.1 Define and use correctly all of the key words printed in bold. (SAQs 9.1, 9.4 and 9.6)
9.2 Estimate the number of people affected by mental illness in your kebele. (SAQ 9.2)
9.3 Explain why mental health is an important public health priority in Ethiopia. (SAQs 9.3 and 9.5)
9.4 State the probable causes of mental illness according to the biopsychosocial model, and describe cultural explanatory models for mental illness. (SAQ 9.4)
9.5 Describe the structure of mental healthcare in Ethiopia. (SAQs 9.1 and 9.4)
9.6 List the ways in which you can help to reduce the treatment gap for mental illness. (SAQ 9.6)
9.1 Mental health as a public health priority in Ethiopia
We will start by defining two terms that will be important for all the mental health study sessions in this module:
Mental health can be defined as ‘a state of well-being in which the individual realises his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community’. (World Health Organization)
Mental illnesses occur in the absence of mental health, and are generally characterised by some combination of abnormal thoughts, emotions, behaviour and relationships with others.
Sometimes people ask the question ‘why is mental health important in Ethiopia when people are dying from illness and poverty?’ or they may say ‘mental health is a luxury for the West’. These attitudes come about from ignorance and the stigma that surrounds mental illness. In the following subsections we will show you why we need to tackle mental illness in Ethiopia.
9.1.1 Mental illness is common
Stop and think for a moment. How common do you think mental illness is in Ethiopia?
From studies that have been carried out in Ethiopia, we know that severe mental illness is present at about the same level that is found in Western countries.
Around 1 to 2% of the adult Ethiopian population, that is around 400,000 to 800,000 people across the country, are affected by psychosis. People with psychosis may believe things that aren’t real, hear things that aren’t there, and have disturbed behaviour. You will learn more about psychosis in Study Session 13 of this Module (see Figure 9.1).
1% means 1 person affected in every 100 persons.

A further 10 to 15% of the adult population (4 to 6 million people) suffer from depression at some point in their lifetime – approximately 5% (2 million) at any one time. In depression, people have an abnormal level of sadness that doesn’t go away. Depression can lead to a person giving up on life and wanting to die. If very severe, somebody with depression may even consider killing themselves (suicide). We don’t know for certain how many people commit suicide in Ethiopia every year, but it is probably at least 4,000 people (10 per 100,000 adults per year). You will learn more about depression in Study Session 12 (see Figure 9.2).

In addition, we estimate that around 5% of the adult population of Ethiopia (around 2 million people) will suffer from an anxiety illness at some point during their lifetime. Anxiety is when a person worries too much about something, for example their health, their problems, or even what will happen in the future. Study Session 16 covers anxiety disorders in more detail (see Figure 9.3).

Added to this large number is the 3 to 5% of the adult population (1.2 to 2 million people) with a serious problem resulting from their excessive use of alcohol or khat. Substance abuse will be covered in more detail in Study Session 14 (see Figure 9.4).

Children can also suffer from mental illness. In Ethiopian studies, around 1 in 10 children seem to have mental health problems (see Study Session 17).
In summary, without including childhood disorders, we estimate that at least 1 in 6 Ethiopians will suffer from a mental illness that needs treatment during their lifetime (Figure 9.5). Is this more common than you expected?
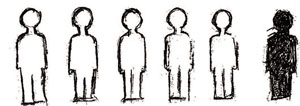
Table 9.1 summarises the frequency of the major types of mental illness in Ethiopia in terms of the percentage of the population who are affected.
| Mental illness | Estimated % of Ethiopian population affected |
|---|---|
| Psychosis | 1–2% |
| Depression | 10–15% |
| Anxiety disorders | 5% |
| Alcohol and khat abuse | 3–5% |
9.1.2 The burden of mental illness
Every illness produces a burden for the person who is affected. Illnesses that cause people to die young (premature mortality) or affect them badly so that they can’t live a normal life (see Box 9.1) are said to have a high burden.
Disability is present when a person has a health condition (in this case, mental illness) which impairs their day-to-day functioning in some way. The level of disability experienced depends partly on the seriousness of the impairment, and partly on the social exclusion that further disables people with mental health problems.
Box 9.1 Disability and mental health problems
Mental health problems may lead to difficulty in one or more of the following areas:
- Understanding and communicating
- Getting around
- Self-care
- Getting along with people
- Working (including housework)
- Participating in society, e.g. attending a funeral or coffee ceremony.
From studies in Ethiopia, we know that:
- People with severe mental illness are about three times more likely to die young.
- People with mental illness have high levels of disability.
- Mental illness often starts early in life and, in some people, can recur (come back again and again), or become chronic (persist over a longtime). So mental illness can affect people over a long period of time.
These three factors mean that the burden of mental illness (in terms of mortality and disability) is high.
In a study from Butajira (south-central Ethiopia), researchers found that if you added together the burden from all the illnesses people experience (including infectious disease, maternal disorders and undernutrition), mental illness was responsible for 11.5% of the total burden. Put another way, more than 10% of the burden of all illness in Ethiopia is likely to be due to mental illness.
Mental illness also causes a burden on the family. Family members may have to stop working in order to care for the mentally ill person. They may also worry a lot about the ill person, which puts them at risk of developing mental illness themselves unless they have good support.
9.1.3 No health without mental health
It is not possible for a person to be healthy unless they have good mental health. Often mental health and general health (‘physical’ health) affect one another. Here are some examples of how mental illness is linked to other health conditions that are important in Ethiopia:
- Millennium Development Goal 4: Child health In Ethiopia, children have an increased risk of diarrhoea if their mother suffers from undetected mental illness. Other studies have shown that the children of mothers with mental illness also have poorer development.
- Millennium Development Goal 5: Maternal health In Ethiopia, women who suffer from mental illness are more likely to have a prolonged labour and delivery. In women with complications during pregnancy or childbirth, the risk of mental illness after the birth is increased.
- Millennium Development Goal 6: HIV/AIDS In Ethiopia we know that people with HIV/AIDS are at increased risk of developing mental illness. People with HIV/AIDS who also have a mental illness are more likely to get worse faster and die earlier than people in good mental health.
Box 9.2 Millennium Development Goals (MDGs)
By 2015 all countries in the world are committed to achieving the following goals:
MDG 1 End poverty and hunger
MDG 2 Universal education
MDG 3 Gender equality
MDG 4 Child health (reducing under-five mortality by two-thirds)
MDG 5 Maternal health (reducing maternal mortality by three-quarters)
MDG 6 Combat HIV/AIDS
MDG 7 Environmental sustainability
MDG 8 Global partnership.
9.1.4 Mental health and poverty (Millennium Development Goal 1)
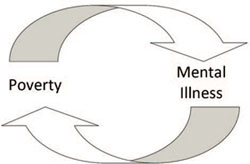
Poverty and mental illness are closely linked. The stresses of poverty can lead to mental illness, and mental illness can make a person poorer (see Figure 9.6). When a person is affected by a severe mental illness, they are more likely to be jobless and may not be able to do their work properly, e.g. plough the fields, sell things in the market. The person with mental illness, and their family, may suffer terrible economic hardship.
9.1.5 Stigma, discrimination and abuse
In addition to the burden of their illness, people with mental illness and their families are highly stigmatised – that is, they suffer from the effects of stigma. Stigma refers to the way in which a characteristic, e.g. mental illness, marks the person out as different and leads to negative attitudes (prejudice) and behaviour (discrimination) from other people. This stigma increases the burden of illness further. People with mental illness may also experience abuse, e.g. being chained up inside a house, especially if the family doesn’t know any other way of coping with the disturbed behaviour (Figure 9.7).

- The stigma of mental illness means that people often hide away and don’t get the help they need.
- Discrimination against people with mental illness may mean that their family is treated unfairly, that the affected person doesn’t have as many work opportunities as he or she should do, or that he or she is excluded from community activities. Discrimination makes mental illness worse and it can delay or prevent recovery.
Later in this Module you will learn about ways to tackle stigma, discrimination and abuse against mentally ill people in the communities where you live and work. Next, we would like you to complete Activity 9.1.
Activity 9.1 What is it like to live with mental illness?
Is there somebody in your kebele who has severe mental illness? Try to find somebody who has received treatment in a psychiatric centre. If they are willing, ask them about their experience of being ill. What was it like? How did other people treat them? What help did they get? What would have helped them more?
Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting.
9.2 What causes mental illness?
9.2.1 The biopsychosocial model
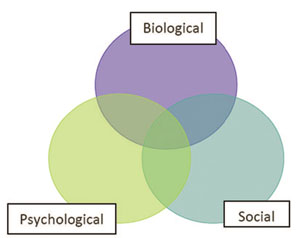
The causes of specific mental illnesses vary but most are caused by a combination of biological, psychological and social problems. Mental health professionals have developed a model of mental illness called the ‘biopsychosocial’ model (see Figure 9.8).
A model is a simplified way of describing how the different parts of a complex issue link together.
As Figure 9.8 shows, the biological, psychological and social factors often overlap. Here are some examples of biological, psychological and social causes of mental illness:
- Biological causes: genetic (inherited) causes, a chemical imbalance in the brain, head injury, alcohol or khat use, undernutrition
- Psychological causes: not loved in childhood, too many worries, the stress of somebody dying, disappointment, frustration, severe shock
- Social causes: poverty, not living in a good house, not having somebody who they can talk to about their problems, discrimination, migration.
Now read Case Study 9.1. As you do so, think about your answers to the following question:
Can you identify some possible biological, psychological and social factors contributing to Mr Hailu’s mental illness?
Case Study 9.1 Mr Hailu the farmer
A 33-year-old farmer developed mental illness after getting into a fight with one of his neighbours. For many years, the farmer had drunk araki every day to help him forget his problems. When he was drunk, he insulted his neighbour and they fought together. The neighbour hit him heavily on the head and the farmer fell to the floor for a few minutes before he was able to get up again. After that the farmer stayed in the house and then developed symptoms of mental illness. Nobody was sympathetic to the farmer because he had caused a lot of trouble in the local area. He had lost all his money because of his drinking, and his wife had gone back to her own family because she couldn’t stand it any longer. All these problems made him worry and he wished he had somebody to talk to. He couldn’t turn to his family because both parents died when he was a small child and his brothers lived far away.
Biological factors: in Mr Hailu’s case study he had a head injury and a long-term history of excessive alcohol use. Psychological factors: he had too many worries, and his parents died in childhood. Social factors: he was isolated and had nobody to talk to.
9.2.2 Explanatory models and cultural context
In the communities where you work, local people may have different explanations for why mental illness occurs. The way people explain an illness is called an explanatory model. Healthworkers often have different explanatory models (e.g. the biopsychosocial model) when compared with the local cultural model used by community members. See Table 9.2 for an example of this. It is very important to try to understand a person’s explanatory model for mental illness even if you don’t agree with it. This will help you to support the person better. You will learn more about how to manage competing explanatory models of mental illness in Study Session 18 on mental health promotion and Study Session 19 on disability and community rehabilitation.
| Questions | Biopsychosocial model | Local cultural model |
|---|---|---|
| Why did I get ill? | Because I was drinking and had lost my family and friends. | Because my neighbour bewitched me. |
| Will I get better? | Things could get better if I stopped drinking. | This is a serious thing. I might even die unless this curse is removed from me. |
| What treatment might help? | If I had help to stop drinking, and was able to talk about my problems to somebody. | Going to see the witch doctor (tanquaye) and slaughtering a sheep. |
Box 9.3 presents a list of some of the cultural explanations of mental illness found in Ethiopia. Beside those in Box 9.3, you could write down other causes that you know of in your area.
Box 9.3 Cultural explanations for mental illness
Spirit possession (likift, zar, wuqabi)
Punishment for sins
Evil eye
Bewitched/cursed
Thinking too much
Exposure to cold air (berrd)
Exposure to sun rays (mitch).
9.3 The treatment gap
So far, you have learned that mental illness is common and has a heavy burden for people affected by it, including family members. One of the best ways to reduce the burden of mental illness is to provide effective treatment. Simple, cheap and effective treatments are available for most mental illnesses but, in Ethiopia, only 10% of people with severe mental illness ever receive these treatments. The difference between those who need treatment and those who get treatment is known as the treatment gap.
From your general knowledge of people in your community, why do you think so many people with mental illness never receive the treatment that could help them?
Some possible reasons that may have occurred to you are as follows:
- they don’t know that effective treatments exist
- they don’t know where to get help
- the stigma prevents them asking for help
- they have to travel too far for help
- they can’t afford the medication
- they don’t believe that health staff can help with this kind of problem
- they prefer to have traditional treatments
- they don’t like the side-effects of medication
- they don’t believe that they have an illness.
In the next section you will learn about how mental healthcare can become more accessible to those who need it by providing support through the healthcare system.
9.4 Structure of the Ethiopian mental healthcare system
9.4.1 Mental healthcare in Ethiopia
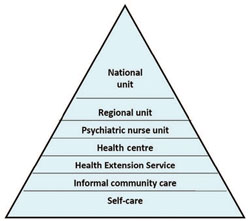
Figure 9.9 shows what mental healthcare is available for people with mental illness in Ethiopia. At the bottom, the biggest part of the triangle is labelled ‘self-care’. Self-treatment describes how the person with mental illness does things to try to help themselves, e.g. talks to someone they trust about their problems, stops drinking heavily, takes a rest from studying, and so on.
Usually when self-care isn’t enough to solve the problem, a person with mental illness will then access ‘informal community care’. This might include going to a priest or religious person for healing, e.g. holy water, driving out demons, or consult one of the traditional healers such as a herbalist, or a witch doctor (tanquaye). While a person with mental illness may find some of these healing practices to be helpful, other traditional practices may be harmful, e.g. beating, fumigation, instructing people to stop taking their medication. These harmful practices can be considered to be ‘abuse’.
As you can see, every level of the healthcare system in Ethiopia (from the Health Extension Service right up to the national referral units in Addis Ababa, e.g. Amanuel Hospital) needs to be involved in delivering mental healthcare. That is essential if we want to increase the number of people with mental illness who receive effective treatment. There aren’t enough psychiatrists and psychiatric nurses to see everybody who needs help. In any case, people with mental illness often don’t want to go to specialist mental health services. If mentally ill people can receive care from local health services then they don’t have to travel so far and they won’t have to spend so much money.
9.4.2 Mental healthcare and the Health Extension Service
As a key member of the Health Extension Service, you have several important roles to play in the primary healthcare system (the system operating at local level). These are summarised in Box 9.4.
Box 9.4 The roles of Health Extension Practitioners in mental healthcare
- Improving detection of mental illness by identifying people who are affected in your community
- Referring people with possible mental illness to the nearest health facility for further assessment and treatment
- Supporting people with mental illness and their families in the community
- Encouraging people to attend follow-up appointments and to keep taking their medication
- Educating patients, their families and the wider community
- Reducing stigma, discrimination and abuse against people with mental illness.
You will learn more about your role in relation to specific mental illnesses in later study sessions.
At the health centre level, nurses and health officers will decide whether the person with mental illness needs to be referred for more specialist assessment, e.g. at the psychiatric nurse unit, or even for in-patient care, e.g. at the regional psychiatric unit.
Finally, we would like you to complete Activity 9.2.
Activity 9.2 Mental healthcare in your area
So that you can advise people with mental illness, it is important to know about mental healthcare in your area. Find out what mental healthcare is available in your nearest health centre. Where is the nearest psychiatric nurse unit? Is there a regional in-patient unit? Outside the health system, where do people with mental illness look for help in your area?
Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting.
In the next study session in this Module, you will learn about assessing the person with mental illness.
Summary of Study Session 9
In Study Session 9 you have learned that:
- An estimated 1 in 6 Ethiopians will suffer from a mental illness that requires treatment during their lifetime.
- Mental illnesses carry a heavy burden in terms of disability and premature mortality.
- Mental health is important to be able to achieve the Millennium Development Goals, especially poverty eradication, child health, maternal health and combating HIV/AIDS.
- People with mental illness experience high levels of stigma, discrimination and abuse, and this can interfere with their recovery.
- The biopsychosocial model shows how biological, psychological and social factors often interact to cause mental illness.
- Cultural explanations of mental illness may stop people seeking effective care and can conflict with the healthworker’s understanding of what caused the illness.
- Only 1 in 10 people with severe mental illness in Ethiopia receive effective treatment for their condition.
- Most mental healthcare is provided outside the existing health system, especially from self-care, family support and traditional and religious healing.
- The Health Extension Service can help to close the treatment gap by improving detection and referral of mental illness, and supporting people with mental illness to take medication and attend for follow-up treatment.
- Other important roles of the Health Extension Practitioner include educating patients, their families and the wider community about mental illness, and reducing stigma, discrimination and abuse against people with mental illness.
Self-Assessment Questions (SAQs) for Study Session 9
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 9.1 (tests Learning Outcomes 9.1 and 9.5)
Which of the following statements are false? In each case explain why it is incorrect.
A The burden of mental illness is measured only in terms of the increased mortality that it causes.
B A woman who has severe depression can’t get out of bed to complete her housework – this is an example of disability.
C In the health system, most mental healthcare is provided by psychiatrists and psychiatric nurses.
D A man had psychosis and recovered well after receiving treatment, but he is refused work because he was once mentally ill. This is an example of discrimination.
E Self-care means that a person with mental illness doesn’t need any help from health services.
Answer
A is false – the burden also includes the amount of disability that a person suffers because of their mental illness.
B is true – although some people may describe the woman as lazy, this is not correct. She cannot work because of her mental illness and so this is disability.
C is false – most people do not have any access to specialist mental healthcare and must rely on ways of helping themselves or getting help within the family (self-treatment), using traditional healers (informal community care) or receiving care through the primary healthcare system.
D is true – this is an example of negative behaviour towards a person just because they had a mental illness and not because of their ability to do the job. Therefore it is discrimination.
E is false – self-treatment is what the person does to help themselves to get better, but often people with mental illness also need help from the health system, e.g. medication for people with psychosis.
SAQ 9.2 (tests Learning Outcome 9.2)
For an average kebele of 5,000 people, can you calculate how many adults might be suffering from mental disorders?
Use the percentages listed in Table 9.1. For example, in a kebele you would expect half the population to be of adult age (2,500 people) and 2% of these adults (0.02 × 2,500 = 50) to have psychosis.
Answer
If the adult population of a typical kebele is about 2,500 people, we would expect the following number to have a mental illness:
50 adults (2% of 2,500) with severe mental illness (psychosis)
250–375 adults (10–15% of 2,500) with depression
125 adults (5% of 2,500) with anxiety disorders
75–125 adults (3–5% of 2,500) who have a problem with alcohol or khat.
These numbers show that it is likely that many people in your kebele could be affected by mental illness. Some adults may be affected by more than one disorder at the same time, e.g. depression and alcohol abuse.
SAQ 9.3 (tests Learning Outcome 9.3)
A community leader comes to tell you that you shouldn’t waste your time on people with mental illness. Write down 5 things you can tell him to try to convince him that mental health is important in his community.
Answer
Some reasons to bother about mental illness in the local community could include:
- Mental illnesses are common – they affect 1 in 6 people
- People with mental illness are more likely to die young
- Mental illness causes a lot of disability and means that the whole family is more likely to be poor
- Mental illness can be treated with cheap and simple medication, but few people manage to get the treatment
- Mental illness can complicate health conditions such as HIV/AIDS
- People with mental illness (and their families) endure a lot of unnecessary suffering because of stigma, discrimination and abuse.
Read Case Study 9.2 and then answer the questions that follow it.
Case Study 9.2 Mrs Tigist the postnatal woman
Mrs Tigist is a 28-year-old woman who developed the mental illness called psychosis soon after giving birth to her second child. While she was pregnant her husband lost his job and the family had to sell a cow so that they had enough money. Now Mrs Tigist can’t understand what is happening to her and is frightened that an evil spirit has possessed her mind. She believes she might die. The family take her to holy water but she doesn’t get better. They then spend a lot of money consulting the witch doctor (tanquaye), but again she doesn’t get better. The family cannot cope with Mrs Tigist’s disturbed behaviour and chain her up in the home.
SAQ 9.4 (tests Learning Outcomes 9.1, 9.4 and 9.5)
- a.Using the biopsychosocial model, can you identify possible causes for Mrs Tigist’s illness?
- b.What is an explanatory model?
- c.What explanatory model does Mrs Tigist have about her illness?
- d.How would you speak to Mrs Tigist about her illness?
- e.What would you advise the family about the levels of healthcare available for Mrs Tigist?
Answer
- a.Possible biological causes could be (i) inheriting increased risk of psychosis from her mother, and (ii) hormonal changes following childbirth. Stress because of her husband’s joblessness and their resulting poverty could be a social cause of her illness.
- b.An explanatory model is the way that a person understands their illness, including why it happened, what caused it, how serious it is, and what treatments they believe will help.
- c.Tigist understands her illness to be caused by an evil spirit. She believes that the illness is serious and that she could die. She believes the best treatment for her condition is from holy water or a traditional healer.
- d.You could explain to Tigist that you understand she is worried that her condition is caused by an evil spirit. You could then say that, in your experience, such a condition can also be due to changes in hormones that happen after childbirth. You could tell her that you would expect medical treatment to help her, and that she can continue her traditional treatments as well.
- e.You can advise the family that medical treatment is available for Tigist’s condition and encourage them to take her to the nearest health facility that can deliver mental healthcare. This might be the health centre or the nearest psychiatric nurse unit. You can also encourage the family to remove the chains.
SAQ 9.5 (tests Learning Outcomes 9.1 and 9.3)
Describe how mental health is important to the Millennium Development Goals.
Answer
Mental health is relevant to the following Millennium Development Goals:
MDG 1 End poverty and hunger Mental illness leads to poverty because the affected person may be too unwell to work, and sometimes because people with mental illness experience discrimination and don’t have as many opportunities to work.
MDG 2 Universal education Undetected mental illness in children interferes with their ability to benefit from education.
MDG 4 Child health Undetected maternal mental illness can affect child health (diarrhoea episodes), growth and development.
MDG 5 Maternal health Maternal health is compromised by mental illness. Pregnant women with depression and anxiety are more likely to have a prolonged delivery. Also, women who experience a complicated delivery are more likely to develop mental illness.
MDG 6 Combat HIV/AIDS Undetected mental illness can lead to people with HIV/AIDS not taking their medication regularly, resulting in a worse outcome.
SAQ 9.6 (tests Learning Outcomes 9.1 and 9.6)
- a.What is meant by the treatment gap for mental illness?
- b.How can the Health Extension Service help to reduce the treatment gap?
Answer
- a.The treatment gap is the gap that exists between the need for treatment for mental illness and the treatment that is actually available. In Ethiopia 9 out of 10 people with mental illness don’t receive the treatment that they need. This is a very high treatment gap.
- b.The Health Extension Service can help to reduce the treatment gap for mental illness by doing the following things:
- increasing detection of mental illness
- referring people with mental illness to the health centre
- supporting people with mental illness and their families
- encouraging people with mental illness to attend their follow-up appointments and take their medication
- educating patients, their families and the community
- challenging stigma, discrimination and abuse.