Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Tuesday, 23 April 2024, 9:38 AM
Adolescent and Youth Reproductive Health Module: 4. Sexually Transmitted Infections (STIs)
Study Session 4 Sexually Transmitted Infections (STIs)
Introduction
In this study session, you will learn why young people are at risk of developing sexually transmitted infections (STIs), and the long-term health consequences of acquiring these infections. You will learn about the major STI syndromes, what biological and social factors influence their transmission and what advice to offer on how individuals can protect themselves from STIs.
STIs, including HIV are discussed in Study Session 28 in Part 3 of the Module on Communicable Diseases, but in this session you will learn about the peculiar features of these infections among young people. Note that you are not expected to treat STIs. The Ethiopian Ministry of Health has recommended that treatment of STIs using the syndromic approach will only be given at a health centre or hospital. You are, however, expected to identify young people with STIs and refer them to the appropriate health facility.
Learning Outcomes for Study Session 4
When you have studied this session, you should be able to:
4.1 Define and use correctly all of the key words printed in bold. (SAQ 4.1)
4.2 Explain why young people are at risk of acquiring STIs. (SAQ 4.1)
4.3 Describe the impact of STIs (including HIV) on young people. (SAQ 4.3)
4.4 Describe how you can work with young people to ensure that they understand prevention strategies that can be used to stop the transmission of STIs, including HIV. (SAQs 4.2 and 4.4)
4.1 Why are young people at risk from sexually transmitted infections?
According to the World Health Organization (WHO), the highest reported rates of STIs are found among 15–24 year olds, while about half of all of the people infected with HIV and 60% of all new HIV infections are also in that age group. WHO also estimates that in 2008 there were around one million Ethiopians living with HIV.
The most widely known STIs are gonorrhoea, syphilis and HIV – but there are more than 30 STIs and disease syndromes that result from STIs. It is important to note that certain STIs substantially increase the risk of transmission of HIV for both men and women. HIV, in its turn, facilitates the transmission of some STIs and worsens the complications of STIs because it weakens the immune system.
Why do you think young people have a high risk of contracting STIs including HIV?
There are many biological, psychological and social reasons that put young people at a high risk of acquiring STIs. The major ones are listed below.
Biological factors:
- Young women are biologically more susceptible to STIs than older women. This is because their vaginal mucosa and cervical tissue are immature, and this makes these tissues more vulnerable to STIs.
- Boys and girls may have immune systems that have not previously been challenged and have not mobilised defences against STIs and HIV.
- Young people may also be more prone to infection because of anaemia or malnutrition.
Another biological factor, though not exclusive to young people, is that women often do not show symptoms of chlamydia and gonorrhoea (the most common STIs), so they do not seek treatment. For example, up to 70% of women and 30% of men infected with chlamydia have no symptoms. Similarly, up to 80% of women and 10% of men infected with gonorrhoea also have no symptoms.
Psychosocial factors:
- Adolescents often lack basic information concerning their sexual health, or the symptoms, transmission and treatment of STIs.
- Often there is poor communication between young people and their elders, and there are few learning materials (books, magazines) designed for young people.
- Sexual intercourse is often unplanned and spontaneous among young people.
- They often have multiple, short-term sexual relationships and do not consistently use condoms.
- Young people may feel peer pressure to have sex before they are emotionally ready to be sexually active and they often confuse sex with love and engage in sex before they are ready in the name of ‘love’ (see Figure 4.1).
- Young men sometimes have a need to prove their sexual powers. Young men may have their first sexual experiences with prostitutes (commercial sex workers), while young women may have their first sexual experiences with older men, both of which increase the chance of getting STIs including HIV.
- Sexual violence and exploitation, lack of formal education (including sex education), inability to negotiate with partners about sexual decisions (in some cultures, girls are not empowered to say ‘No’) and lack of access to reproductive health services together put young women at especially high risk.
- Some adolescents are subject to early marriage, forced sex, trafficking and poverty, and may engage in sex work for money or favours.
- Substance abuse or experimentation with drugs and alcohol is common among young people, which often leads to their making irresponsible decisions such as having unprotected sex.
Even when young people realise that they are infected they may be afraid to seek treatment for STIs and so go on to infect others unnecessarily.
4.2 Impact of STIs (including HIV) on young people
Sexually transmitted infections are of public health concern because of their potential to cause serious and permanent complications in infected people who are not treated in a timely and effective way. These can include cervical cancer, pelvic inflammatory disease, chronic pelvic pain, fetal death, ectopic pregnancy (pregnancy outside the uterus) and related maternal mortality. Chlamydial infections and gonorrhoea are important causes of infertility, particularly in women, with far-reaching social consequences including break-up of marriages. Chlamydial infection is an important cause of pneumonia in infants. Neonatal gonococcal infections of the eyes can lead to blindness. Congenital syphilis is an important and significant cause of infant morbidity and mortality. In adults, syphilis can cause serious cardiac, neurological and other consequences, which can ultimately be fatal.
Generally, the long-term health consequences of STIs are more serious among women.
Why should this be so?
This is because, women and girls are less likely to experience symptoms, and so many STIs go undiagnosed until a serious health problem develops.
People who become ill from STIs may face loss of community credibility and even health workers sometimes treat them badly, being judgemental and refusing to provide services. It is important that you provide a good role model and become known for being sympathetic and non-judgemental.
4.3 STI prevention strategies for young people
As a Health Extension Practitioner, you should advise and encourage young people to adopt the following healthy behaviours:
- Delay onset of sexual activity. Abstain from sexual intercourse until married or in a stable relationship.
- Learn how to use condoms. If young people are already sexually active, it is important to make sure they know how to use condoms correctly. You should demonstrate the proper use of condoms in your education sessions related to sexually transmitted infections either individually or in group meetings (in schools, at the health post or in the community).
- Condoms should always be used except when pregnancy is desired or when partners in a stable relationship know for certain they are both disease-free.
- Avoid any kind of risky behaviour; try to stick with one partner. Boys should avoid having contact with prostitutes.
- Discuss sexual issues. Young men and women must feel comfortable communicating with their partners and family about sex and their sexual histories. A communicative relationship is essential to emotional and physical health.

When you discuss these sexual issues with young people it is also a good idea to tell them how to recognise the symptoms of STIs (Figure 4.2). For example, you should explain that if they experience burning with urination, have a discharge from the penis/vagina, and/or have genital sores then they and their partner should not have sex but should go to the higher level health facility for treatment.
4.4 Young people with HIV
There are two groups of young people living with HIV: those who were infected around birth and have survived into adolescence and those young people who have been infected during adolescence, usually through unprotected sex. This infection history has an impact on many features of how HIV affects a young person, including prevention strategies and their HIV care and management (e.g. progression of HIV disease, treatment with antiretroviral therapy (ARV drugs), knowledge and disclosure of HIV status, access to care). For example, young people who have acquired the HIV infection at birth will have symptoms earlier than those infected after adolescence.
Young people who are infected before entering puberty often grow slowly and enter puberty later than is normal. Girls have irregular menstrual periods. This delay in growth and sexual maturation may also have an impact on the psychosocial development of the individual.
For young people infected after puberty, the infection can remain asymptomatic for a longer period of time than for adults. The younger the age at infection (after puberty), the longer the virus remains asymptomatic.
4.4.1 Prevention of the HIV epidemic
HIV prevention among young people is the key to reducing infection rates and slowing the epidemic. Those between the ages of 15 and 24 are at the greatest risk of acquiring and transmitting HIV. They are both the most threatened and the greatest hope for reversing the HIV epidemic, by changing attitudes and behaviours. The future epidemic will be shaped by the action and behaviour of young people.
The major aims of HIV prevention include:
- Prevent transmission of HIV for all people (HIV-negative, HIV-positive or of unknown status), to reduce the number of new infections.
- Help people who are HIV negative to stay negative.
- Promote testing and counselling for people who do not know their status.
Young people everywhere report that the education they receive about HIV and sexual reproductive health is too little and too late. Adults are often hesitant to provide young people with the facts about HIV prevention and sexual health, often because they fear this will encourage sexual activity. But there is convincing evidence from studies in many different cultures that, in fact, sex education encourages responsibility. Knowledgeable young people tend to postpone intercourse or, if they do have sex, to use condoms.
4.4.2 Who has a role in HIV prevention?
HIV prevention requires active involvement from all members of society to ensure an environment where young people feel safe and supported and able to protect themselves from HIV at home, school and work and in their community.
Young people
HIV prevention must focus on young people because young people have an essential role in slowing the epidemic. Many young people listen to their peers and believe their peers. Young people can be trained to spread messages and promote responsible behaviour among their friends and colleagues. This is known as peer education and is discussed in Study Session 12. As a Health Extension Practitioner you can help by raising the awareness of young people about STIs including HIV through peer education and education in schools.
Parents and other adults in the community
All adults have a role to play in their personal capacity as parents, members of extended families and adult role models. They may also have a professional role as teachers, sports coaches and religious leaders. Studies have identified that having a positive relationship with parents, teachers and other adults in the community and having spiritual beliefs helps adolescents avoid behaviour that puts them at risk of HIV.
Targeted strategies must be available that focus on individual needs. (E.g. safer sex information and free condoms for young prostitutes; outreach information programmes for young people who have left school).
Public idols who are role models for young people
Musicians, film stars and sports figures provide role models for young people through their personal lives and through their performances. The images and messages they portray should encourage young people to adopt and maintain healthy behaviours. You can use known examples to help you deliver safer sex messages and to discourage risky behaviour.
Government leaders and the media
Politicians, journalists and public servants can affect the social, economic, and political factors that determine the risk environments for HIV infection in which young people live and work. Public images of sexual behaviour and HIV in the media influence young people. You should look out for those that can help you achieve the aims of HIV prevention.
People living with HIV
People living with HIV and those with AIDS have a role in HIV prevention. They have a personal role to ensure they do not transmit HIV to any other person. People living with HIV are frequently subject to discrimination and human rights abuses. A strong movement of people living with HIV and AIDS can develop a network that provides mutual support and a voice at local and national levels and can be a particularly effective method of tackling HIV stigma. If there are such people living in your community you can work with them to teach young people about ways of preventing HIV infection and also offer your support by showing that you are not judgemental in your dealings with such people.
4.4.3 Key HIV prevention strategies for young people that you can offer at health posts
HIV prevention services must be offered to young people whenever they come for health services (STI, antenatal care, family planning, etc). Key prevention strategies for young people cannot be the same for all but need to be adapted to their different needs. For example for boys and girls in primary school (early adolescence age 10–14), it is appropriate to talk about the changes during puberty and the benefits of abstinence and delaying sexual activity. By contrast, for post-adolescents (aged 20–24) education about faithfulness and safer sex using condoms is relevant as they are likely to have started sexual activity anyway. Similarly, you need to provide appropriate messages for adolescents in and out of school and young people both married and unmarried based on their needs for information and services.
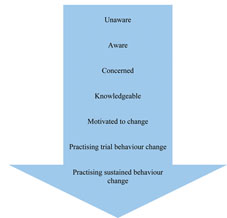
Postponing the first sexual activity and reducing the number of sexual partners can significantly protect young people from HIV. Behavioural change communication can help young people to develop positive behaviours. Behavioural change communication is the process of using communication approaches and tools to develop the skills and capabilities of individuals to promote and manage their own health and development. It promotes positive change in their behaviour, as well as in their knowledge and attitudes. The messages and the way the messages are given are very important for young people, as they do not want to only hear what they cannot do, but also what they can do. Figure 4.3 shows the stages of behaviour change that an individual passes through, from being completely unaware to making positive behaviour changes.
As you can see in Figure 4.3, behaviour change doesn’t immediately follow awareness. It takes some time for individuals to change their behaviour even after they have the necessary knowledge. Hence, whenever you counsel young people who are already engaged in some form of risky behaviours (such as having multiple sexual partners, chewing khat, or drinking alcohol), it is important that you tell them they shouldn’t expect everything to change overnight. Behaviour change is a process that needs to be continuously supported and reinforced in order to bring the desired change.
Provider-initiated testing and counselling and voluntary counselling and testing (VCT) services need to be available at all health facilities and in the community. These methods can be used both for giving information on sexual behaviour and HIV and also for opening the discussion on many sensitive issues faced by young people (e.g. peer pressure, condom negotiation, unwanted pregnancy, decision making, how to be an adult, disclosure of HIV status). There are more details on provider-initiated testing and counselling in Study Session 26 of the Communicable Diseases, Part 2 Module.
The use of latex condoms to prevent the exchange of body fluids during sex is an essential element of all HIV prevention activities. Safer sex depends on the correct and consistent use of condoms, so condom provision must be accompanied by clear instructions on condom use for every act of penetrative sex. Female condoms offer women an option that may give them more control but they also require more counselling and assistance with respect to their proper use and they are also more expensive and less available. Condom promotion also supports dual protection.
What is meant by dual protection?
Dual protection is the simultaneous protection against unwanted pregnancy and the possible transmission of STIs including HIV.
STIs greatly facilitate HIV transmission and acquisition between sexual partners, so treating and preventing them is an important step in HIV prevention. Effective and early treatment of STIs is an essential part of HIV prevention. Hence, it’s important that you refer adolescents with STIs to minimise the risk of transmission and complications.
Summary of Study Session 4
In Study Session 4, you have learned that:
- STIs including HIV are common among young people for biological and psychosocial reasons. Biologically, young women are more susceptible to STIs than older women because of their immature vaginal mucosa and cervical tissue.
- Adolescents are likely to engage in unsafe sexual practices (including having multiple sexual partners, using prostitutes and not using condoms), which predisposes them to STIs including HIV. This is because they often lack basic information concerning their sexual health, including ignorance of the symptoms, transmission, and treatment of STIs.
- In most rural areas girls are married at a very early age and they are not empowered to say ‘No’. As a result, young women may have their first sexual experiences with older men while young men may have their first sexual experiences with prostitutes; both behaviours increase the chance of getting STIs including HIV.
- STIs in young people can lead to multiple long-term negative consequences for their health and social life and can even result in early death. Health problems include pelvic inflammatory disease, chronic pelvic pain, fetal death, ectopic pregnancy, cervical cancer and related maternal mortality. Chlamydia and gonorrhoea can also result in infertility, particularly in women. Chlamydia can cause pneumonia in infants, while neonatal gonococcal infections of the eyes can lead to blindness. Syphilis in adults can cause serious heart and brain disease which can be fatal.
- Young people can acquire HIV in two ways through infection from their mothers at birth or through unprotected sex during adolescence. This infection history has an impact on how HIV affects a young person and on their HIV care and management.
- HIV prevention requires active involvement from all members of society including young people themselves, parents, role models, government leaders, the media and people living with HIV and those with AIDS.
- In general, behaviour changes take time and don’t always automatically follow awareness. Hence, it is important that you provide continuous support whenever you counsel young people who are already engaged in some form of risky behaviours to adopt healthy behaviours.
- In addition to awareness raising and education of young people on ways of STI prevention, there is a need to provide condoms and refer them for appropriate counselling and HIV testing.
Self-Assessment Questions (SAQs) for Study Session 4
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
First read Case Study 4.1 and then answer the questions that follow it.
Case Study 4.1 The marriage of Tessema and Meselech
Tessema (23 years) and Meselech (16 years) had been attracted to each other for some time. Meselech had to drop out from school when she was a 5th grade student as her parents felt she was not safe going to school alone; Tessema only completed 4th grade as his father decided that he had to take care of the farm and domestic animals. When they finally began to date, things moved very quickly and they decided to have sex. They were married 6 months later. Neither of them had any information about contraceptive use or STIs.
Almost a month later Tessema comes to see you because he has developed a small sore (blister) on his penis.
A year later Meselech comes to you complaining of having an unusual vaginal discharge and pain during urination. She thinks her problems may be related to the problem Tessema had because she has had similar symptoms many times in the preceding year. She says she has not seen any health worker but has been buying some (unidentified) antibiotics from the nearby drug shop but there has been little improvement. She is also concerned because she has not become pregnant even though she was expecting to conceive any time. She is particularly worried that her inability to conceive might damage her marriage. In addition, she is worried about the possibility of having HIV.
SAQ 4.1 (tests Learning Outcomes 4.1 and 4.2)
Tessema and Meselech may have an STI. Suggest factors that could have put them at risk.
Answer
Tessema and Meselech are young and uneducated. They did not know about dual protection or STIs. They may have contracted STIs from previous partners or Tessema might have visited a prostitute to prove his sexual powers.
SAQ 4.2 (tests Learning Outcome 4.4)
What should Tessema do and what help can you offer?
Answer
Tessema should go to a health facility that can offer treatment and counselling. Since you are not trained to provide this treatment you need to refer Tessema to seek care from the nearest health facility (health centre or hospital) where the service is available. You can advise Tessema not have intercourse before he gets treatment for his illness. You can also explain that he may have an STI and you can provide condoms and tell him about their proper use.
SAQ 4.3 (tests Learning Outcome 4.3)
Explain whether any of Meselech’s problems could be a consequence of having an STI.
Answer
Meselech seems to have one of the STIs characterised by vaginal discharge. She may also be infertile as a consequence of this and if she does not conceive she risks divorce which will affect her social status in the community.
SAQ 4.4 (tests Learning Outcome 4.4)
What advice would you now give to Meselech and Tessema to prevent such problems in the future?
Answer
Meselech appears to have an STI so you need to refer her to the appropriate health facility (health centre or hospital) where she can get treatment. Both Meselech and Tessema should be advised to go for HIV testing and counselling. You need to educate them on the prevention of STIs.
Meselech should also be advised to avoid taking medications without consulting a health professional.