Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Thursday, 18 April 2024, 10:05 AM
Communicable Diseases Module: 5. Malaria Epidemiology and Transmission
Study Session 5 Malaria Epidemiology and Transmission
Introduction
In this study session you will learn about the burden of malaria worldwide, in Africa and in Ethiopia. As malaria is a vector-borne disease you will learn about the vectors, which in the case of malaria are the mosquitoes that carry the malaria parasite from person to person. You will learn where mosquitoes lay their eggs and the stages of development leading up to a new flying adult. Information about the breeding habitats (water collections where mosquitoes lay eggs and develop), and the life cycle of mosquitoes, is essential for you to target anti-vector interventions in the right way. A clear understanding of the life cycle of the malaria parasite and of the mosquito, the vector which transmits it from person to person, will help you carry out your responsibility of protecting people in your community from getting malaria and of treating people who do get malaria.
Learning Outcomes for Study Session 5
When you have studied this session, you should be able to:
5.1 Define and use correctly all of the key words printed in bold. (SAQ 5.1)
5.2 Describe the burden of malaria globally, in Africa and Ethiopia. (SAQs 5.2 and 5.3)
5.3 Describe the life cycle of the malaria parasite. (SAQ 5.4)
5.4 Describe the life cycle of the mosquito vector. (SAQ 5.5)
5.5 Explain how to identify the potential vector of malaria and tell it from other mosquitoes. (SAQ 5.6)
5.6 Describe the behaviour of vector mosquitoes. (SAQ 5.7)
5.1 The burden of malaria
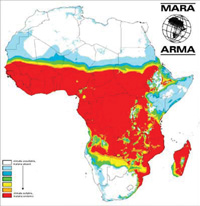
Malaria is one of the most serious diseases to affect people in developing countries with tropical and subtropical climates. It is particularly dangerous for young children and for pregnant women and their unborn babies, although others may also be seriously affected in some circumstances. Malaria is endemic in 109 countries and more than three billion of the world’s population lives in malaria risk regions. Globally, 300–500 million episodes of malaria illness occur each year, resulting in over one million deaths. As Figure 5.1 shows, changes in socio-economic conditions and anti-malaria interventions have gradually reduced the areas of the world where malaria is endemic, but it is still widespread as a major global disease. A communicable disease is said to be endemic in a region or country if it is always present there. In areas where many cases occur throughout the year, the disease is said to be highly endemic, or (to say it another way) it has high endemicity.
Endemic is pronounced 'end-em-ik', and endemicity is pronounced 'end-em-iss-it-ee'.

More than 90% of the worldwide deaths from malaria occur in sub-Saharan Africa and most of these deaths are in children. Malaria risk is highest in tropical Africa where conditions (which will be considered further below) are very favourable for malaria transmission (Figure 5.2).
Look at Figure 5.2 and describe what it shows about the incidence of malaria in Africa.
Figure 5.2 shows that the highest incidence of malaria (as shown in red) is around the equator and in the tropics. Malaria is much less common in the northern and southern part of the continent.
The intricate interactions between host, parasite, vector and the environment are the major factors in the distribution of malaria. Different areas can experience different levels of incidence rates.
Malaria can be viewed in terms of being stable or unstable. Malaria is said to be stable (and therefore endemic) when malaria infections occur for many months in a year, over many years. People living in highly endemic areas usually exhibit a high level of immunity and tolerate the infection well. Immunity against malaria is the ability to fight the infection, which is developed by people with repeated episodes of malaria. Under endemic conditions, children under the age of five years, and pregnant mothers, are most likely to be infected as they have weaker immunity.
Unstable (epidemic) malaria refers to a seasonal type of transmission seen in areas of low endemicity, or to outbreaks in areas previously without malaria, or among non-immune persons. Epidemics can be due to changes in human behaviour, environmental and climate factors. For example, human migration and resettlement can introduce malaria into an area that did not have it previously, and this can expose a population to the disease that was not immune to malaria. Malaria epidemics generally occur when the population in an area has weak immunity to the disease, because so many people in the population will be vulnerable to malaria, not just children under five years of age and pregnant women.
However, it is important to remember that children and mothers are always more at risk, so they will need particular attention.
5.2 Epidemiology and distribution of malaria in Ethiopia
About 75% of the landmass of Ethiopia is malarious and 68% of the Ethiopian population, estimated at about 54 million in 2010, live in malaria risk areas. As you can see from Figure 5.3, malaria is a risk in the western and eastern lowlands and central midlands. However, it is absent or the risk is low in the central highlands, where the altitude (or elevation) is 2,000 metres or more above sea level, as Figure 5.3 shows. As you will see later, the reason is the effects of altitude on the habitat of the mosquito vector, and the development of the parasite inside the mosquito.
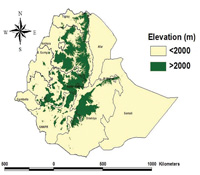
The exact number of people getting sick and dying of malaria every year in Ethiopia is not known. However, it is known that millions of people get sick and tens of thousands of people die due to malaria every year, and that rates of mortality (death) and morbidity (illness) dramatically increase during epidemics. The distribution of malaria in Ethiopia is not uniform. There are areas where the risk of malaria is high and there are areas where the risk is low. There are even areas, 25% of the country, that are malaria free.
You learned in Section 5.1 above that malaria transmission is classified as stable or unstable. The three most important factors that affect the distribution of malaria and its severity in Ethiopia are:
- Temperature
- Humidity (the amount of moisture in the air)
- The availability of water collections in which the mosquito vectors can breed.
Altitude, vegetation and rainfall have indirect effects because of their impact on temperature, humidity and availability of water collections for vector breeding.
The distribution of malaria in Ethiopia varies from place to place due to the above factors directly or indirectly affecting the pattern of malaria transmission. For example, the distribution of malaria in Ethiopia is largely determined by altitude. Altitude affects the pattern of malaria distribution in Ethiopia through its effect on temperature. Risk of malaria is highest in the western lowlands of Oromia, Amhara, Tigray and almost the entire regions of Gambella and Benishangul Gumuz. The midlands of Ethiopia between 1,000 and 2,200 metres altitude experience seasonal transmission of malaria with sporadic epidemics every few years. In the eastern lowlands of Ethiopia (primarily Afar and Somali), malaria is endemic only along the rivers, as this part of the country is largely dry away from rivers. Transmission is limited by the lack of water collections for mosquito breeding and low humidity due to low rainfall and sparse vegetation. The central highlands of Ethiopia are free of malaria mainly due to the low temperatures, which slows the development of the vector and the parasite.
5.3 Malaria parasites
Malaria is caused by Plasmodium parasites. Plasmodium parasites infect people and attack the red blood cells, which often leads to severe illness and death. The parasites are spread to people through the bites of infected Anopheles mosquitoes, which are the malaria vectors and which bite mainly between dusk and dawn.
There are four types of human malaria, each due to one of the parasites with the following specific names:
The species names of malaria parasites are frequently abbreviated to P. falciparum,P. vivax, etc.
- Plasmodium falciparum
- Plasmodium vivax
- Plasmodium malariae
- Plasmodium ovale.
Plasmodium falciparum and Plasmodium vivax are the most common malaria parasites in Ethiopia. 60% of malaria infections in Ethiopia are due to P. falciparum and 40% are due to P. vivax. P. falciparum is the most deadly and requires special attention.
Although both parasites are widely distributed, some communities will have more falciparum malaria while others will have more vivax malaria. Do you know which type of infection is more common in your community?
5.3.1 Life cycle of the malaria parasite
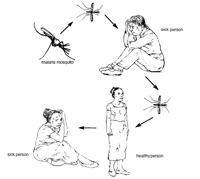
Human malaria (Plasmodium parasite) is transmitted from an infected person to another person by Anopheles mosquitoes, as shown in Figure 5.4. The parasite spreads by infecting two types of hosts: humans and female Anopheles mosquitoes. The mosquitoes then act as the vector for the parasite. Malaria is a human parasite that is transmitted only between people; malaria is not transmitted from animals to humans or from humans to animals.
Now you are going to learn about the life cycle of the parasite. Please study Figure 5.5 very carefully as it is going to help you understand about the pathology, signs, symptoms and treatment of malaria in the subsequent study sessions.
Malaria in humans develops via two stages: a liver and red blood cell stage. When an infected mosquito pierces a person's skin to take a blood meal, malaria parasites in the mosquito's saliva enter the bloodstream and migrate to the person’s liver. Within 30 minutes of being introduced into the human body, they infect liver cells, multiplying in the liver cells for a period of 6–15 days. In the process they become thousands of parasites which, following rupture of the liver cells, escape into the blood and infect red blood cells, thus beginning the red blood cell stage of its life cycle.
Within the red blood cells, the parasites multiply further, periodically breaking out of their host cells to invade fresh red blood cells. Several replication cycles occur. The pathology and clinical manifestations associated with malaria are almost exclusively due to the red blood cell stage parasites (Figure 5.5). The blood stage parasites are those that cause the symptoms of malaria.
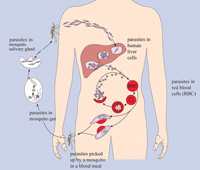
When certain forms of blood stage parasites, called gametocytes, are picked up by a female Anopheles mosquito during a blood meal, they start another, different cycle of growth and multiplication in the mosquito. After 10‒18 days, the parasites are found in the mosquito's salivary glands. When the Anopheles mosquito takes a blood meal from another human, the parasites are injected with the mosquito's saliva and start another human infection when they enter the new person’s liver cells. Thus the mosquito carries the disease from one human to another, acting as a vector. Unlike the infected human, the mosquito vector does not suffer from the presence of the parasites.
The most common way to be infected with malaria is through the natural transmission by mosquitoes, as already described. However, malaria can also be transmitted via blood transfusions or sharing syringes. Mother to child transmission during pregnancy has also been documented, but all the modes of transmission other than via the mosquito are believed to be very rare and unimportant.
5.3.2 Incubation period of malaria
When a person becomes infected with one of the Plasmodium parasites that cause malaria, he or she will not feel sick immediately. The period between infection with the parasites that cause the disease and the beginning of malaria symptoms is called the malaria incubation period. The infected person may feel normal from 7 to 21 days when infected with Plasmodium parasites. P. falciparum has a shorter incubation period (7 to 14 days) than P. vivax (12 to 18 days). Plasmodium malariae tends to have a much longer incubation period, as you can see from Table 5.1.
| Malaria parasites | Incubation period in days |
|---|---|
| P. falciparum | 7‒14 |
| P. vivax | 12‒18 |
| P. ovale | 12‒18 |
| P. malariae | 18‒40 |
As you will learn in Study Session 7, Plasmodium infection causes fever in cycles or episodes which occur at either 48 or 72 hour intervals. Episodes of fever occur when the parasites are released into the blood and infect new red blood cells (see Figure 5.5).
5.3.3 Partial immunity to malaria
The severity of the attack depends on the Plasmodium species, as well as other circumstances, such as the state of immunity and the general health and nutritional status of the infected individual.
Following several attacks of malaria, people living in highly endemic regions can develop partial immunity that can protect them from severe attacks and death. But no-one develops complete immunity against malaria that can fully protect the person from infection. Pregnant women and children under five years of age are more susceptible to severe forms of the disease and death due to their weak immune system.
5.4 Life cycle of the mosquito vector
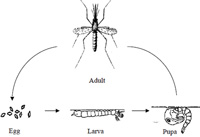
Now you will learn about the life cycle of the vector of the malaria parasite, the mosquito. Mosquitoes have four different stages in their life cycle: the egg, larva, pupa and adult (see Figure 5.6). The first three stages are immature and are found in water collections. The adult is a flying insect. The time taken for the different stages to develop depends on temperature and nutritional factors in their environment. Development takes a shorter time at higher temperatures.
5.4.1 Eggs
A female Anopheles mosquito normally mates only once in her lifetime. It usually requires a blood meal after mating before her eggs can develop. While the blood meal is not essential for the survival of female mosquitoes, it is crucial for successful egg production and egg laying. Blood meals are generally taken every two to three days, before the next batch of eggs is laid. About 100 to 150 eggs are laid on the water surface during oviposition (egg laying). Oviposition sites vary from small hoof prints and rain pools to streams, swamps, canals, river beds, ponds, lakes and crop fields. Each species of mosquito prefers different types of habitats to lay eggs. Under the best conditions in the tropics, the average lifespan of female Anopheles mosquitoes is about three to four weeks.
5.4.2 Larvae
Larvae (pronounced 'lah-vee') is the plural of larva ('lah-vah'); this stage of the life cycle is called the larval stage ('lah-val'). Pupae (pronounced 'pyoo-pee') is the plural of pupa ('pyoo-pah'); this stage of the life cycle is called the pupal stage ('pyoo-pal').
A larva hatches from the egg after one or two days and generally floats parallel under the water surface, since it needs to breathe air. It feeds by taking up food from the water. When disturbed, the larva quickly swims towards the bottom, but it soon needs to return to the surface to breathe. There are four larval stages or instars. The small larva emerging from the egg is called the first instar. After one or two days it sheds its skin and becomes the second instar, followed by the third and fourth instars at further intervals of about two days each. The larva remains in the fourth instar stage for three or four more days before changing into a pupa. The total time spent in the larval stage is generally eight to ten days at normal tropical water temperatures. At lower temperatures, the larval stages take longer to develop.
5.4.3 Pupae
The pupa is the stage during which a major transformation takes place, from living in water to becoming a flying adult mosquito. The pupa is shaped like a comma. It stays under the surface and swims down when disturbed, but it does not feed. The pupal stage lasts for two to three days, after which the skin of the pupa splits. Then the adult mosquito emerges and rests temporarily on the water's surface until it is able to fly.
5.4.4 Adult mosquitoes
Mating takes place soon after the adult emerges from the pupa. The female usually mates only once because it receives sufficient sperm from a single mating for all subsequent egg batches. Normally the female takes her first blood meal only after mating, but sometimes the first blood meal can be taken by young virgin females. The first batch of eggs develops after one or two blood meals (depending on the species); while successive batches usually require only one blood meal. The process of blood-feeding, egg maturation and egg laying is repeated several times throughout the life of the mosquito. The length of time between two feeding cycles depends on the external temperature. In Anopheles arabiensis, for example, the cycle takes 48 hours when the average day-night temperature is 23°C.
5.5 Malaria transmitting vectors in Ethiopia
The scientific names of the mosquitoes that transmit malaria parasites are often abbreviated to An. arabiensis, An. pharoensis, etc.
You have now learned that malaria is transmitted from an infected person to another person by mosquitoes. However, not all mosquitoes carry malaria. There might be mosquitoes biting people in your village, but they may not be the ones that transmit the infection. The mosquitoes that transmit malaria belong to a group of mosquitoes called Anopheles. However, not all Anopheles mosquitoes are vectors of malaria. For example there are more than 40 species of Anopheles mosquitoes in Ethiopia, but only four species of Anopheles mosquitoes carry malaria. The scientific names of these mosquitoes are:
- Anopheles arabiensis
- Anopheles pharoensis
- Anopheles funestus
- Anopheles nili.
An. arabiensis is the most important transmitter of malaria in Ethiopia and is responsible for more than 95% of transmissions. It is found everywhere in Ethiopia. The other three are secondary vectors of very minor importance.
Distinguishing the above four species of Anopheles from other Anopheles mosquitoes is not your responsibility and will not be part of this training. However, it is important for you to distinguish Anopheles mosquitoes in general from other mosquitoes at their larval stage. You will see the importance of this knowledge when you learn about vector control in Study Session 9.
5.6 Distinguishing Anopheles mosquitoes from other types
The terms ‘anophelines’ and ‘culicines’ refer to all species of these mosquito types.
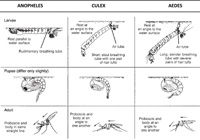
There are two common types of mosquitoes that lay their eggs in water: anophelines, which can be vectors of malaria, and culicines, which do not carry malaria. It is very important that you know the difference in the morphology (structure and shape) of these mosquitoes to identify the exact breeding habitats that support the development of the potential vectors.
Now study the differences in the body structure and resting position in water collections of the anopheline and culicine larvae, as illustrated in Figure 5.7. You don’t need magnifying or other equipment to distinguish anopheline and culicine larvae. You can tell the difference by looking at the larvae in the vector breeding waters. Your mentor will show you the difference between the two during your practical training. This will be a very important part of your task as a Health Extension Practitioner: identifying water collections that shelter anopheline larvae and taking action to eliminate such breeding grounds or kill the larvae. You will learn more about the action against mosquito larvae in Study Session 8.
There are four stages in the mosquito life cycle, and three of them — eggs, larvae and pupae — are to be found in water.
5.6.1 Eggs
Mosquito eggs either clump together in a ‘raft’ (Culex) or float separately (Aedes); anopheline eggs float separately and each of them has ‘floats’.
5.6.2 Larvae
The culicine larva has a breathing tube (siphon) which it also uses to hang down from the water surface, whereas the anopheline larva has no siphon and rests parallel to and immediately below the surface.
5.6.3 Pupae
Pupae of both anophelines and culicines are comma-shaped and hang just below the water surface. They swim when disturbed. The breathing trumpet of the anopheline pupa is short and has a wide opening, whereas that of the culicine pupa is long and slender with a narrow opening. However, it is difficult to distinguish anopheline from culicine pupae in the field.
5.6.4 Adults
With live mosquitoes, you can distinguish between adult anopheline and culicine mosquitoes by observing their resting postures. Anophelines rest at an angle between 50o and 90o to the surface, whereas culicines rest more or less parallel to the surface.
5.7 Behaviour of mosquitoes that transmit malaria
To help you work effectively to prevent malaria transmission, you need to learn about the most important behaviours of a malaria-transmitting mosquito.
Female mosquitoes can feed on animals and humans. Most species show a preference for certain animals or for humans. They are attracted by the body odours, carbon dioxide and heat emitted from the animal or person. Species of mosquitoes that prefer to feed on animals are usually not very effective in transmitting diseases from person to person. Those who prefer to take human blood are the most dangerous as they are more likely to transmit diseases between people. One of the reasons why An. arabiensis mosquitoes are better vectors of malaria than other mosquitoes is that they feed mostly on humans and very little on cattle.
Most anopheline mosquitoes bite at night. Some species bite just after sunset while others bite later, around midnight or in the early morning. Those that bite in the early evening may be more difficult to avoid than species that feed at night.
Some species prefer to feed in forests, some outside houses and others indoors. Mosquitoes that enter a house usually rest on a wall, under furniture or on clothes hanging in the house. Mosquitoes that bite outside usually rest on plants, in holes, in trees, or on the ground, or in other cool dark places. Mosquitoes that rest indoors are the easiest to control, as you will learn in Study Session 6.
Because digestion of the blood-meal and development of the eggs takes 2‒3 days, a blood-fed mosquito looks for a safe resting place that is shaded and offers protection from drying out. Some species prefer to rest in houses or cattle sheds, while others prefer to rest outdoors, on vegetation or at other natural sites. After the mosquito takes a blood meal indoors, it usually rests inside the house, some for a short period and some for days. Mosquitoes do not usually bite while eggs are developing.
Adult females can normally live between 20 days and one month. The average survival is much shorter at 6‒9 days. The average life-span of the female has direct relevance to its efficiency as a malaria vector, because it has to live long enough to transmit malaria (i.e. long enough for the parasite to complete its life cycle in the mosquito host, approximately 10 days).
On average, the flight range of adult Anopheles is between a few hundred metres and 2 kilometres. Therefore water collections very close to houses are more important sources of vectors than those located far away from houses. As you will see in Study Session 9, this is something that could be important when considering vector control measures to prevent vectors from breeding in water collections.
Summary of Study Session 5
In Study Session 5, you have learned that:
- Malaria is a major public health problem in the world, Africa and Ethiopia, affecting millions of people each year.
- The malaria parasite is transmitted from person to person by the bite of female mosquitoes.
- The parasite is taken by the mosquito when feeding on an infected person.
- The parasite develops and multiplies in the mosquito body and the cycle takes about 10 days, depending on the temperature.
- The parasites are injected into humans when the mosquito bites.
- Studying the life cycle of the malaria parasite that causes human malaria makes understanding the pathology, signs, symptoms and treatment of the disease easier.
- Water collections are important for vector breeding.
- Malaria is transmitted by Anopheles mosquitoes only; the larvae of Anopheles mosquitoes can be easily distinguished from other non-vector mosquitoes.
- A female Anopheles mosquito needs to feed on blood to develop its eggs and reproduce.
- The life cycle of the malaria vector from egg to adult takes 8 to 12 days, depending on temperature.
- The vectors bite people from dusk to dawn.
- The vectors can bite people indoors or outdoors.
- The vectors feeding indoors are likely to spend some time resting inside houses after taking a blood meal.
- Understanding the behaviour of the vector is important to plan preventive measures.
Self-Assessment Questions (SAQs) for Study Session 5
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 5.1 (tests Learning Outcome 5.1)
A person from a malaria-free place visiting a high malaria risk area shows signs and symptoms of malaria after 8 days of his stay in the area. Which of the following types of malaria parasites is the person most likely to be infected with: P. falciparum, P. vivax, P. ovale or P. malariae? Explain how you reached your answer.
Answer
P. falciparum is the most likely cause of the infection, because the symptoms began after 8 days. The period between infection with the parasites that cause the disease and the beginning of malaria symptoms (incubation period) for P. falciparum is 7–14 days. It is longer for the other species of Plasmodium.
SAQ 5.2 (tests Learning Outcome 5.2)
You have learned that the burden of malaria in Africa is higher than other parts of the world, and also that the malaria incidence varies in different regions of Africa. Where in Africa is the incidence of malaria highest? Where is malaria incidence low?
Answer
- Malaria incidence is high in countries around the tropics or closer to the equator.
- It is low in northern and southern African countries.
SAQ 5.3 (tests Learning Outcome 5.2)
The distribution of malaria in Ethiopia is not uniform. What are the possible explanations for the difference in malaria incidence in different areas of Ethiopia?
Answer
- Malaria incidence is high in the western lowlands of Ethiopia where the temperature and humidity is high and favourable for mosquito and parasite development.
- There is no malaria in the highlands because of low temperature.
- There is less malaria in the eastern lowlands because rainfall and humidity are low.
SAQ 5.4 (tests Learning Outcome 5.3)
Carefully study the life cycle of the parasite in the human body and the mosquito (see Figure 5.5). List the body parts of the mosquito and the body parts of humans that are directly associated with parasite development and reproduction.
Answer
The body parts directly associated with the development and reproduction of the malaria parasites are:
- Mosquito: gut and salivary glands.
- Human: liver and red blood cells.
SAQ 5.5 (tests Learning Outcome 5.4)
The following are statements about the life cycle of the malaria vector mosquito. Which of these statements is false? In each case, explain what is incorrect.
A The malaria vector mosquito lays its eggs on grass.
B The malaria vector mosquito life cycle has four stages.
C The malaria vector mosquito needs to feed on blood to develop its eggs.
D The adult female mosquito lays eggs only once in its life time.
E The stage that hatches from the eggs is the pupae.
Answer
A is false. The malaria vector mosquito lays its eggs on water surfaces (not grass).
B is true. The malaria vector life cycle has four stages: eggs, larvae, pupae and adults.
C is true. The mosquito needs to feed on human or animal blood to develop its eggs.
D is false. The adult female mosquito lays eggs several times in its life cycle.
E is false. The stage that hatches from the eggs is the larvae.
SAQ 5.6 (tests Learning Outcome 5.5)
List two characteristics that illustrate how the Anopheles larvae are different from other mosquito larvae.
Answer
Two characteristics that distinguish the Anopheles larvae from other types are:
- It has no breathing siphon.
- It rests parallel or horizontal to the water surface.
SAQ 5.7 (tests Learning Outcome 5.6)
You know that the parasite needs 10 days to develop inside the mosquito body. Therefore the mosquito needs to live at least 10 days to be able to transmit the infection. 10% of the mosquitoes live more than 10 days in February and more than 20% of them live more than 10 days in September.
- a.Do you expect malaria transmission to occur during these two periods?
- b.During which period will the incidence of malaria be higher?
Answer
- a.Yes; the 10% of mosquitoes living more than 10 days will have the potential to transmit malaria.
- b.Malaria transmission will be higher in September because a larger percentage of mosquitoes live more than 10 days during September.