Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Saturday, 7 March 2026, 10:14 AM
Antenatal Care Module: 3. Anatomy and Physiology of the Female Reproductive System
Study Session 3 Anatomy and Physiology of the Female Reproductive System
Introduction
Applied anatomy and physiology for basic obstetric care is an entry to your studies in this Module and the next four Modules, and is essential preparation for your practical skills training. Obstetric care refers to healthcare for women during pregnancy, labour and delivery, and their immediate postnatal care. It requires a good understanding of the anatomy and physiology of the female reproductive system. Anatomy is the study of the structures of the human body, i.e. the features of how the organs, tissues and body systems are constructed. Physiology, on the other hand, is the study of the coordinated functions of the organs, tissues and systems in the body.
In this study session, you will learn about the structures that make the external female genitalia and the internal reproductive organs. In Session 4, we teach you about the hormonal regulation of the internal female reproductive organs and the female monthly menstrual cycle (bleeding from the vagina). In Study Session 5, we describe ovulation, fertilisation and implantation of the embryo in the mother’s uterus (womb), and the development of the fetus, the placenta and fetal nutrition. In Study Session 6, you will learn the anatomy of the female bony pelvis, and also of the fetal skull, which has to pass through the mother’s pelvis during delivery.
Learning Outcomes for Study Session 3
When you have studied this session, you should be able to:
3.1 Define and use correctly all of the key words printed in bold. (SAQs 3.1 and 3.2)
3.2 Identify and describe the basic anatomical features of the external female genitalia and the internal reproductive organs. (SAQs 3.2, 3.3 and 3.4)
3.3 Describe the functions of the main anatomical structures in the female reproductive system and their importance for obstetric care. (SAQs 3.3 and 3.4)
3.1 Some common terms in anatomy and physiology
In learning anatomy and physiology for the first time, you will be exposed to a large number of new terminologies. Some of these may be familiar to you from your previous biology course at high school. In this study session, we have tried to use simple terms as much as possible to help you understand the study material. Defining most of the terms used in anatomy and physiology is beyond this study session, but defining the most important terms used in obstetric care will help you achieve the learning outcomes of this study session and Study Sessions 4 to 6.
The terminologies used in human anatomy often include a directional term, i.e. a term that indicates the position of one anatomical structure in relation to another one, or in relation to the body as a whole (see Box 3.1). You will encounter directional terms many times in this Module.
Box 3.1 Some common directional terms used in anatomy
Superior: above
Inferior: below
Medial: towards the midline of the body
Lateral: away from the midline (sides, edges)
Anterior: in front of
Posterior: behind, at the back of
3.2 Anatomy and physiology of the female reproductive organs
The reproductive role of females is far more complex than that of males:
- Women produce ova (eggs), which can be fertilised by the male.
Ova (plural) is pronounced ‘oh vah’. Ovum (singular) is pronounced ‘oh vumm’
- After fertilisation, women also carry and protect the developing fetus in the uterus.
- After childbirth, the breasts (mammary glands) produce milk to nourish the baby.
By nature, every one of us is eager to know how we develop in our mother’s uterus, how a fetus (the growing baby inside the uterus) develops during the nine months of pregnancy, how it is nourished, and how the female menstrual cycle is controlled. To understand these and other related questions about female reproductive functions, you have to learn about the anatomy (structure) of the female reproductive organs, and understand the physiology (function) of each organ.
We begin with the anatomical positions of the female reproductive organs in relation to the urinary system (the kidneys and bladder), the gastrointestinal system (the ‘gut’ where digestion of food occurs), and other nearby structures in the pelvic cavity, (see Box 3.2 and Figure 3.1 below).
Box 3.2 Cavities in the human body
A cavity is a space in the human body which contains different organs, fluids and other structures. For example, the cranial cavity contains the brain; the chest cavity contains the lungs and the heart; the abdominal cavity contains the stomach, intestines, liver, kidneys and some other organs; and the pelvic cavity contains the reproductive organs and bladder. Note that the pelvic cavity is actually the lower part of the abdominal cavity, and that there is no barrier between them.
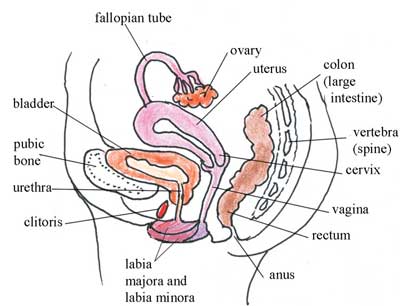
Look carefully at Figure 3.1 for about two minutes, taking note of the position of the labelled structures. Choose the correct directional terms from Box 3.1 to describe the position of the uterus in relation to the bladder.
The bladder is in front of (anterior to) the uterus, or you could say instead that the uterus is behind (posterior to) the bladder. The top part of the uterus is bending over the bladder and is above (superior to) it, or you could say that the bladder is below (inferior to) the top of the uterus.
Behind (posterior to) the uterus, cervix and vagina in Figure 3.1, you can see part of the large intestine (colon) and the rectum, where solid waste is directed out of the body through the anus. Knowing about the anatomical position of all these structures is very important during pregnancy, labour and delivery. For example, in the pregnant woman, the enlarging uterus containing the growing fetus will push down on the bladder and large intestine. This can often result in decreased urine-carrying capacity of the bladder, so the woman has to urinate (pee) more frequently, and she may also experience constipation (drying and difficulty of passing stools).
When you are studying the female reproductive system, you have to bear in mind that structurally it is divided into two broad categories. Structures external to the vagina are said to be the external female genitalia, whereas structures above the vagina (including the vaginal canal), and lying internally, are called the internal female reproductive organs. You have already seen some structures in both categories from the side view in Figure 3.1. Now we will look at each of them in more detail.
3.3 External female genitalia
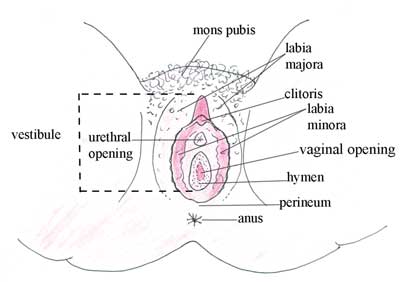
Look at Figure 3.2 carefully. All the structures which are visible externally, surrounding the urethral and vaginal openings, including the mons pubis, labia majora, labia minora, vestibule and perineum, make the external female genitalia. Sometimes these structures are collectively named the vulva.
Structures in the external female genitalia have a nerve supply, which can respond to different sensory stimuli (touch, pain, pressure and temperature). This makes these structures sensitive and active to sexual arousal during touch, especially by the male partner. Following this, the sexual act between the male and female facilitates the ejaculation of male sex cells into the female internal reproductive organs, initiating the process of fertilisation, pregnancy, labour and delivery.
Notice in Figure 3.2 that the urethral opening, the vaginal opening and the anus are all close together in the vulva. What do you think is the clinical importance of this close relationship for the pregnant woman?
As you know, the area around the anus is contaminated with bacteria from waste matter emerging from the gastrointestinal tract. So, direct bacterial contamination of the urethral and vaginal openings easily occurs.
Advising the pregnant woman to keep this area clean through good personal hygiene is very important. Infections of the bladder and vagina are common in pregnancy, and if bacteria get into her uterus, she could lose the baby.
Now we will look at each of the structures in Figure 3.2, beginning with those on the outer edges of the diagram, and ending with those in the centre.
3.3.1 Mons pubis
The mons pubis is a thick, hair-covered, fatty and semi-rounded area overlying the symphysis pubis. Symphysis is a type of strong and immovable joint between bones. As you will see in Study Session 6 (Figure 6.1), the two halves of the pubic bone are joined in the middle by the pubic symphysis. The function of the fatty tissue in the mons pubis is to protect the woman’s pubic area from bruising during the sex act.
Symphysis is pronounced ‘simm feh siss’.
3.3.2 Labia majora and labia minora
The labia majora are two elongated, hair-covered, fatty skin folds that enclose and protect the other organs of the external female genitalia.
The labia minora are two smaller tissue folds enclosed by the labia majora. They protect the opening of the vagina and the urethra (the tube that carries urine from the bladder to the urethral opening in the vulva). The labia minora normally have an elastic nature, which enables them to distend and contract during sexual activity, and labour and delivery.
How is this elasticity helpful during delivery?
The labia minora can stretch to let the baby’s head out.
In some countries, including parts of Ethiopia, the labia minora and the clitoris (described below) may be removed by female genital mutilation (FGM), one of the harmful traditional practices.
Female genital mutilation is discussed in the Module on Adolescent and Youth Reproductive Health.
3.3.3 Vestibule
The vestibule is the area between the labia minora, and consists of the clitoris, urethral opening and the vaginal opening.
The clitoris is a short erectile organ at the top of the vestibule, which has a very rich nerve supply and blood vessels. Its function is sexual excitation and it is very sensitive to touch. Its anatomical position is similar to the position of the male penis.
If the clitoris and labia minora are removed by female genital cutting, the vaginal opening will not expand easily during childbirth due to the scarring where tissue has been removed. This can result in difficulty in labour and delivery, including severe bleeding and rupture of the scarred tissue, sometimes even causing a fistula — a hole torn in the wall of the vagina.
Female genital mutilitation that involves the labia minora and clitoris is usually performed without an anaesthetic. What will be the consequence of this for the female?
There will be severe pain due to the nerve supply to this area, which can lead to fainting (becoming unconscious).
Also, the labia minora and clitoris have a rich blood supply, so cutting them leads to severe bleeding, which may cause fainting and shock.
The urethral opening is the mouth or opening of the urethra, which is a small tubular structure that drains urine from the bladder. In Study Session 22, at the end of this Module, and in your practical training classes, you will learn how to insert a small tube (called a catheter) into this opening to drain urine from the bladder. This may be necessary during emergency care for a pregnant woman, or during labour and delivery, if she cannot pass urine for herself because the tissues of the vestibule have swollen and squashed the urethra flat.
The vaginal opening is the entrance to the vagina. It is where you will begin to see the ‘presenting part’ of the baby as it stretches wider open near the end of labour.
3.3.4 Perineum and hymen
The skin-covered muscular area between the vaginal opening and the anus is called the perineum. It has strong muscles and its own nerve supply, and it helps to support the contents of the pelvic cavity. The hymen is a fold of thin vaginal tissue which partially covers the vaginal entrance in girls. It can be torn during strenuous exercise, as well as by the first sexual penetration.
3.4 Internal female reproductive organs
In learning about pregnancy and delivery, understanding the anatomical structures involved in production of eggs (ova), fertilisation and fetal development is fundamental. In this section, you will learn how to identify and describe the internal female reproductive organs involved in these processes. Knowledge of the position and function of these organs is also essential for the accurate examination of pregnant women, and a safe labour and delivery.
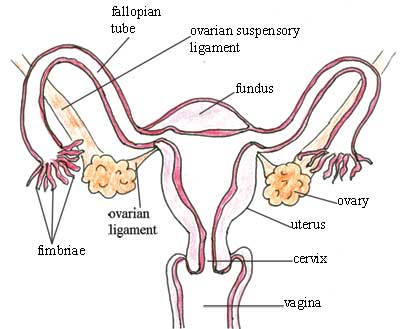
3.4.1 Fallopian tubes and ovaries
Begin by looking carefully at Figure 3.3. As you can see from the diagram, there are two fallopian tubes — one on each side of the uterus — and the finger-like ends of each tube (called the fimbriae) are close to the ovary on the same side, and open to the pelvic cavity. This means that if there is an infection in the pelvic cavity, it can get into the uterus through the fallopian tubes. Similarly, if there is an infection in the uterus, it can spread along the fallopian tubes and out into the pelvic cavity, and from there all around the woman’s abdomen, affecting her other organs. This can be very dangerous if it is not treated early.
Fallopian is pronounced ‘fah loh pee ann’. Fimbriae is pronounced ‘fimm bree aye’.
The ovaries are paired female reproductive organs that produce the eggs (ova). They lie in the pelvic cavity on either side of the uterus, just below the opening of the fallopian tubes (see Figure 3.3). They are kept in position through attachment to two ligaments. Ligaments are the fibrous, slightly stretchy, connective tissues that hold various internal organs in place; they also bind one bone to another in joints.
Women are born with a fixed number of immature eggs (ova), around 60,000 in number. The eggs are held in small ‘pits’ in the ovaries, named ovarian follicles. Each ovum has the potential to mature and become ready for fertilisation, but in actuality only about 400 ripen during the woman’s lifetime. Every month, several ovarian follicles begin to enlarge and the ovum inside it begins to mature, but usually only one will ‘win the race’ and be released from the ovary. The moment when the ovum is released is called ovulation. The other enlarging follicles degenerate.
What could happen if two ova are released at the same time?
The woman could become pregnant with twins.
The enlarging ovarian follicles also produce the female reproductive hormones, oestrogen and progesterone, which are important in regulating the monthly menstrual cycle, and throughout pregnancy. You will learn a lot more about these hormones in Study Sessions 4 and 5.
Oestrogen is pronounced ‘ee stroh jenn’. Progesterone is pronounced ‘proh jest err own’.
Hormones are signalling chemicals that are produced in the body and circulate in the blood; different hormones control or regulate the activity of different cells or organs.
After ovulation, the lining of the empty follicle grows and forms a yellow body in the ovary called the corpus luteum, which temporarily functions as a hormone-producing organ.
Corpus luteum is prounounced ‘korr puss loot ee umm’.
It secretes oestrogen and progesterone for about the next 14 days. Oestrogen thickens the fatty tissues in the wall of the uterus in case pregnancy occurs. Progesterone stops further ovulation from occurring during the pregnancy.
Why is it beneficial to prevent further ovulation once a woman is pregnant?
It means she cannot get pregnant again during this pregnancy, so all her resources can go towards nourishing and protecting the first fetus developing in her uterus.
But if pregnancy does not occur within 14 days after ovulation, the corpus luteum degenerates and stops producing progesterone. As a result, the blood supply to this additional fatty tissue in the wall of the uterus is cut off, and it also degenerates and is shed through the vagina as the menstrual flow. The levels of oestrogen can then begin to rise, and the woman can ovulate again in the following month.
When an ovary releases a mature ovum (ovulation), the fimbriae of the fallopian tube catch the ovum and convey it towards the uterus. The male sperm swim along the fallopian tubes, and if they find the ovum, they fertilise it (as you will see in Study Sessions 4 and 5). The lining of the fallopian tubes and its secretions sustain both the ovum and the sperm, encourage fertilisation, and nourish the fertilised ovum until it reaches the uterus.
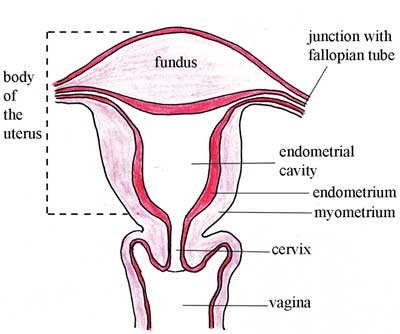
3.4.2 The uterus
The uterus is a hollow, muscular organ in which a fertilised ovum becomes embedded and develops into a fetus. Its major function is protecting and nourishing the fetus until birth.
During pregnancy, the muscular walls of the uterus become thicker and stretch in response to increasing fetal size during the pregnancy. The uterus must also accommodate increasing amounts of amniotic fluid (the waters surrounding the fetus, contained in a bag of fetal membranes), and the placenta (the structure that delivers nutrients from the mother to the fetus). You will learn a lot more about this in Study Session 5.
Why do you think the muscular walls of the uterus become thicker during pregnancy?
A thicker layer of muscle has the strength to support the growing fetus and the other contents of the uterus, which get much heavier as pregnancy proceeds.
The uterus has four major anatomical divisions, shown in Figure 3.4:
- Body: the major portion, which is the upper two-thirds of the uterus.
- Fundus: the domed area at the top of the uterus, between the junctions with the two fallopian tubes.
- Endometrial cavity: the triangular space between the walls of the uterus.
- Cervix: the narrow neck at the upper end of the vagina.
The wall of the uterus has three layers of tissue, two of which are shown in Figure 3.4:
- The perimetrium: the outermost thin membrane layer covering the uterus. (It is not important for you to know this term for obstetric care.)
- The myometrium: the thick, muscular, middle layer in Figure 3.4.
- The endometrium: the thin, innermost layer of the uterus, which thickens during the menstrual cycle. This is the tissue that builds up each month in a woman of reproductive age, under the influence of the female reproductive hormones.
What happens to the endometrium if the hormones stop circulating after ovulation?
The blood supply to the endometrium is cut off, and it sheds from the body through the vagina as the monthly menstrual flow.
3.4.3 The cervix and the vagina
The cervix is the lower, narrow neck of the uterus, forming a tubular canal, which leads into the top of the vagina (see Figure 3.4). It is usually about 3 to 4 cm (centimetres) long.
The vagina is a muscular passage, 8 to10 cm in length, between the cervix and the external genitalia. The secretions that lubricate the vagina come from glands in the cervix.
The vagina has three functions. Can you suggest what they are?
It is a receptacle for the penis, where sperm are deposited during sexual intercourse. It is the outlet for the menstrual flow every month in the non-pregnant woman. And it is the passageway down which the baby passes at birth.
Pregnant women should be encouraged to strengthen the muscles of the vagina by contracting (squeezing) them as hard as they can at least 10 times, and repeating this exercise at least four times a day. A woman can learn to do this exercise while she is urinating. As the urine comes out, she should contract the muscles in her vagina until the urine stops, then relax the muscles so the urine flows again. Once she learns how to squeeze these muscles, she should only do it when she is not urinating. Doing the squeezing exercises can help to:
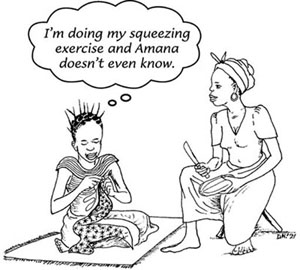
- Prevent leaking of urine
- Prevent the vagina and perineum from tearing when they are stretched during childbirth
- Speed healing after birth
- Increase sexual pleasure.
In this study session you have studied the structures and functions of the organs in the female reproductive system and their importance in obstetric care. In the next study session you will look at the hormonal regulation of the reproductive cycle in women.
Summary of Study Session 3
In Study Session 3, you have learned that:
- Anatomy is the study of the structures of the human body, and physiology is the study of the coordinated functions of the organs, tissues and body systems.
- The female reproductive system is divided into the external genitalia (below and exterior to the vaginal opening), and the internal reproductive organs (above the vaginal opening in the pelvic cavity).
- The internal reproductive organs are close to the bladder, the large intestine and the rectum; the external opening of the vagina is close to the urethral opening and the anus. These close relationships increase the opportunities for infection to spread in the genital area.
- In some traditional societies, the clitoris and labia minora are often removed by female genital mutilitation; this can have serious (even fatal) consequences for the woman, especially during labour and delivery.
- The ovaries are female sex organs which usually produce one ovum every month during the reproductive years. One of the fallopian tubes carries the ovum from the ovary towards the uterus. If fertilisation occurs, it normally happens in the fallopian tube.
- The uterus is a muscular organ, which gives mechanical protection and nutritional support to the developing fetus during pregnancy.
- The female reproductive hormones, oestrogen and progesterone, direct the maturation of ova in the ovaries, the release of an ovum (ovulation), and the thickening of the endometrium (the fatty lining of the uterus). If fertilisation of the ovum and pregnancy does not result, the endometrium is shed as the menstrual flow.
- The vagina functions as a passageway for elimination of the menstrual flow; it receives the penis during sexual intercourse; and it forms the lower portion of the birth canal.
Self-Assessment Questions (SAQs) for Study Session 3
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 3.1 (tests Learning Outcomes 3.1 and 3.2)
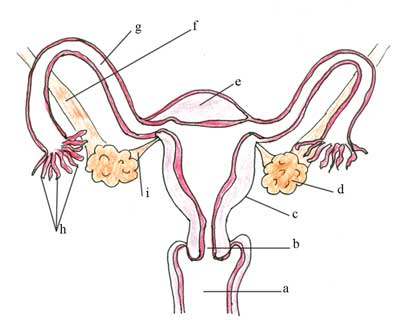
Look at Figure 3.5. Label the anatomical features marked from ‘a’ to ‘i’.
Answer
The correct labels for Figure 3.5 are as follows:
a is the vagina
b is the cervix
c is the uterus
d is the ovary
e is the fundus
f is the ovarian suspensory ligament
g is the fallopian tube
h is the fimbriae
i is the ovarian ligament.
SAQ 3.2 (tests Learning Outcome 3.1)
Choose the correct directional terms from Box 3.1 to describe the relative positions of the uterus and the rectum in Figure 3.1.
Answer
The uterus is anterior to (in front of) and superior to (above) the rectum. An alternative way of expressing the same positions is to say that the rectum is posterior to (behind) and inferior to (below) the uterus.
SAQ 3.3 (tests Learning Outcomes 3.2 and 3.3)
Which structures are removed in female genital mutilation, and what harm can come to a woman during labour and delivery as a result?
Answer
The structures removed in female genital mutilation are usually the clitoris and the labia minora. The scarring that results as the cuts heal interferes with the normal ability of the vulva to stretch during childbirth to allow the baby to pass through the birth canal. As a result, the birth can be obstructed and the vagina can tear, causing severe pain and loss of blood. In some cases, a fistula (hole in the vaginal wall) can tear open, and blood loss can put the woman’s life at risk.
SAQ 3.4 (tests Learning Outcomes 3.2 and 3.3)
Which of the following statements is false? In each case, state why it is incorrect.
A Infection in the uterus can get into the pelvic cavity through the vagina.
B The perineum is a muscular area between the vaginal opening and the anus.
C The maturation of an ovum is controlled by the female reproductive hormones.
D Glands in the cervix produce secretions which lubricate the vagina.
E The fundus is the narrow ‘neck’ at the bottom of the uterus.
Answer
A is false. Infection in the uterus can get into the pelvic cavity by passing outwards through the fallopian tubes, which are open at the ends. Infection in the uterus can pass down the vagina, and usually appears as a bad-smelling discharge from the vaginal opening in the vulva.
B is true. The perineum is a muscular area between the vaginal opening and the anus.
C is true. The maturation of an ovum is controlled by the female reproductive hormones.
D is true. Glands in the cervix produce secretions which lubricate the vagina.
E is false. The fundus is the name for the domed top of the uterus. The narrow neck at the bottom of the uterus is called the cervix.