4.1 Are the diagnostic categories correct?
According to DSM-IV-TR, if the criteria for two or more disorders – such as MD and GAD – are each satisfied in the same person, the disorders are comorbid.
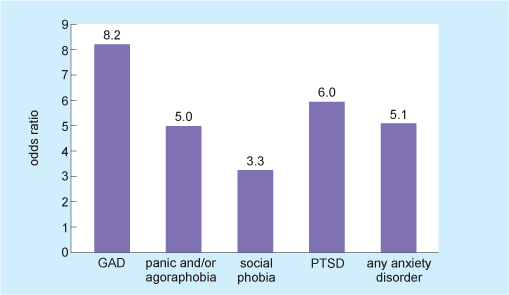
In fact, MD and GAD are often comorbid. Figure 12 shows the odds ratios for having an anxiety disorder at the same time as major depression. Box 6 explains what an odds ratio is if you are not familiar with this term.
Box 6 Odds ratio
Imagine that the chances in the USA of adult men having GAD are on average 1 in 100. But what of the subset of adult men who already have MD? What are the chances that such men will have GAD as well as MD? An odds ratio tells us about the increase in the chance that such men will have GAD, already having MD. If having MD increases the chances of having GAD from the usual 1 in 100 to 8.2 in 100, then the odds ratio for having GAD when you have MD is 8.2. If having MD has no effect at all on the chances of having GAD then the odds ratio is 1.00 (it does not affect the odds). An odds ratio of 1.05 means for the population of men with MD the chances of having GAD are increased by 5%. The further away from 1 the odds ratio is, the stronger the effect.
What might this kind of pairing between MD and GAD suggest?
That there is some connection between the two conditions. For instance: (i) one causes the other; (ii) both are due to a common cause; (iii) there is just one underlying condition with a range of symptoms, with some symptoms matching the (artificially set up) criteria for one condition and others matching the criteria for the other condition.
Activity 8 Identifying an odds ratio
Look at Figure 12. What is the odds ratio that ‘any anxiety disorder’ will be present in people who have major depression? What does this mean?
Answer
The odds ratio that ‘any anxiety disorder’ will also be present in people who have major depression is 5.1. This means that the chance of ‘any anxiety disorder’ being present is 5.1 times higher in people who have major depression, compared to the normal chance of having ‘any anxiety disorder’.
In practice, it is increasingly recognised that in many cases a person has some symptoms of depression (but not enough to justify a diagnosis of depression), and some symptoms of anxiety (but not enough to justify a diagnosis of anxiety). Neither DSM-IV-TR nor ICD-10 provide for the proper diagnosis of such a condition. However, an increasing number of researchers recognise this as mixed anxiety and depression disorder (MADD), also called mixed anxiety and depression (MAD – see Figure 1) or cothymia (Tyrer, 2001). Indeed MAD was found to occur in around 55% of all those suffering from an emotional disorder (or common mental disorder) (McManus et al., 2009), making it the most common emotional disorder by far.
The existence of strong comorbidity between anxiety and depression, and mixed anxiety and depressive disorder, have led some researchers to suggest that these disorders lie on an anxiety–depression continuum or spectrum.
Indeed there is evidence to suggest that ‘cases’ of disorder might map onto a single spectrum of ‘counts of mental symptoms’, with no evidence for clustering of symptoms into disorders such as those proposed by DSM-IV-TR and ICD-10 (Das-Munshi et al., 2008; Melzer et al., 2002).
Using a CIS-R scale (‘Clinical Interview Schedule – Revised’ scale – see Box 7), Das-Munshi et al. (2008) assessed the presence of symptoms of mental disorder and mapped them onto ‘recognised’ depression and anxiety disorders such as MD, GAD, MAD and comorbid anxiety and depression.
Box 7 Clinical Interview Schedule – Revised (CIS-R)
The CIS-R is a structured interview schedule used in national surveys such as the Adult Psychiatric Morbidity in England, 2007: results of a household survey (McManus et al., 2009) to assess neurotic symptoms and common mental disorders in the population. For each interviewee, the severity of symptoms such as fatigue, concentration and forgetfulness, sleep problems, irritability, depressive ideas, depression, anxiety, panic, worry about physical health, compulsions, obsessions and so on, is scored on a scale of 0–4 (0–5 in the case of depressive ideas). The scores are summed to give an overall severity score: a score of 12 or more indicates a significant level of symptoms, and a score of 18 or more suggests treatment is needed. In the APMS (2007) interviewees’ answers to the CIS-R were also used to derive ICD-10 diagnoses of GAD, MD, phobias, OCD and panic disorder. MAD was defined as having a CIS-R score of 12 or more but falling short of the criteria for any other common mental disorder.
The distribution of CIS-R scores they obtained for the four different disorders (and for ‘no diagnosis’) is shown in Figure 13.
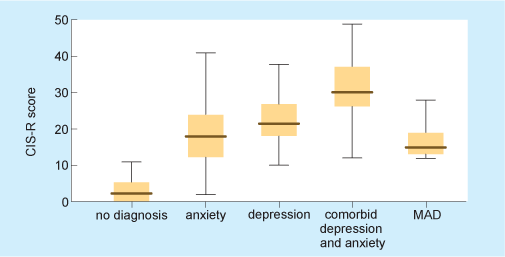
The higher the CIS-R score, the more serious on average a disorder is likely to be. On this basis, looking at Figure 13, which of the four disorders would appear to be least serious and which would appear to be most serious?
Mixed anxiety-depression would be least serious; comorbid depression and anxiety would be most serious.
Interestingly, such critiques appear to be having some impact. The next version of the DSM (DSM-5, published 2013), while still applying a categorical approach, proposed a new disorder called mixed anxiety depression.
Activity 9 Using the diagnostic categories
Think back to Suzanna’s case in Vignette 2. Does it satisfy DSM-IV-TR criterion C for the diagnosis of GAD (Box 7)? Give reasons for your answer.
Answer
Yes, her case appears to satisfy criterion C. Suzanna has at least three of the symptoms listed, and she has suffered from GAD for over 6 months. The symptoms she has include: (6) sleep disturbance (she mentions insomnia); (5) muscle tension (she mentions ‘feelings of tightness in the head’) and (1) feeling keyed up or on edge (she mentions ‘constant feeling that I am going to die’, which could fit with this).
