2.1.1 Brain circuits and selective attention
After many years of research, scientists have begun to propose specific circuits involved in endogenous and exogenous selective attention. There is not yet a complete consensus on this, but there is now a good understanding of which structures are likely to be involved, even if the exact role of each brain region is not entirely understood.
Activity 6 Selective attention in the brain
Watch Video 5, which describes the structures and circuits thought to be involved in selective attention. As you watch the video, make notes about the brain structures involved in each type of attention. You may need to pause the video or watch it a couple of times. Then answer the questions that follow.
Transcript: Video 5 Selective attention networks in the brain
Which type of selective attention is driven by sensory stimuli, for example a flash of light?
Answer
This is exogenous attention.
What is the key difference between exogenous and endogenous attention, in terms of where the brain circuits begin?
Answer
The brain circuit for exogenous attention begins in sensory areas such as the visual cortex, whereas the circuit for endogenous attention begins in the prefrontal cortex.
Video 5 showed that there are several structures involved in selective attention, and therefore potentially implicated in the development of ADHD. One structure that has received a lot of attention in ADHD is the prefrontal cortex (PFC), which is a brain region responsible for reasoning, moderating behaviour, planning and decision making. The PFC has been examined using both structural and functional imaging techniques in children, adolescents and adults with ADHD and the results compared with participants of a similar age without ADHD.
Structural studies have consistently shown reductions in the volume of the PFC in individuals with ADHD relative to those without ADHD (Rubia et al., 2014). Furthermore, the reduction in volume correlates with illness severity (Mostofsky et al., 2002). It is suggested that this is due to delayed brain development in ADHD.
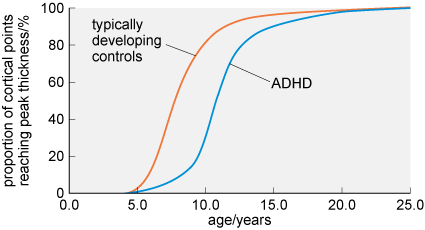
Longitudinal studies in the USA have supported this idea showing that, relative to typical controls, individuals with ADHD can show a delay in reaching the peak of cortical thickness and surface area by up to five years (Figure 7).
-
What percentage of cortical areas are fully developed in individuals following a typical trajectory compared with those with ADHD at the age of 10 years?
-
At 10 years of age, around 80% of cortical areas have reached peak thickness in typically developing children. This is compared with just 30% in children with ADHD.
Given the emphasis on the PFC in the brains of people with ADHD, you may be unsurprised to know that the frontal cortex, which includes the PFC, is the area which has the greatest delay in development (Shaw et al., 2007; 2013).
As well as delays in brain development, meta-analyses have shown that there are abnormalities in the white matter within the brain, including the PFC regions in the brains of individuals with ADHD. White matter within the brain is so called because it appears white when the brain is dissected. These white areas of the brain are made up of connections between brain cells, known as axons. The abnormalities discussed are thought to be due to a reduction in myelination of these axons (Rubia et al., 2014). Myelination is the name given to the process by which axons become coated in a fatty insulating substance called myelin. One of the functions of this substance is to speed up the conduction of signals between brain cells, so a reduction in myelination will slow down signalling within the brain.
As with reduced brain volume, the reduction in myelination correlates with severity of symptoms; the greater the reduction, the poorer the cognitive performance (Chuang et al., 2013).
Meta-analyses of functional brain imaging studies suggest a reduction in activity within the PFC in the brains of individuals with ADHD (Christakou et al., 2013). Interestingly, the reduced activity can be normalised with medication for the condition (Hart et al., 2012; Rubia et al., 2014), which you will learn more about in Sections 2.2.3 and 2.2.4.
-
What is the evidence for alterations to the PFC in the brains of individuals with ADHD?
-
- The PFC is reduced in volume and shows reduced activity.
- The PFC develops more slowly and has altered white matter (meaning signalling will be slower).
- The structural changes are correlated with symptoms and severity of the condition.
- Drug treatment for ADHD can normalise PFC activity.
As well as identifying specific brain regions important for attention and ADHD, changes in specific neurotransmitters, the chemical messengers of the brain, have also been identified.
