4 Case study: resistance to cephalosporins
In Week 3’s case study, you looked at the molecular mechanisms of resistance to cephalosporins and were introduced to ESBLs. The most common class of ESBLs in Europe is the
In this case study, you will explore how bacteria acquire resistance to cephalosporin antibiotics through horizontal gene transfer and the mutation of CTX-M-type ESBLs. You will begin by looking at how the presence of CTX-M-type ESBLs has changed in the UK over recent years.
Activity 5 The rise of CTX-M-type ESBLs
The data in this activity are from The British Society for Antimicrobial Chemotherapy’s Resistance Surveillance Project (www.bsacsurv.org) which collects annual data on antibiotic resistance rates.
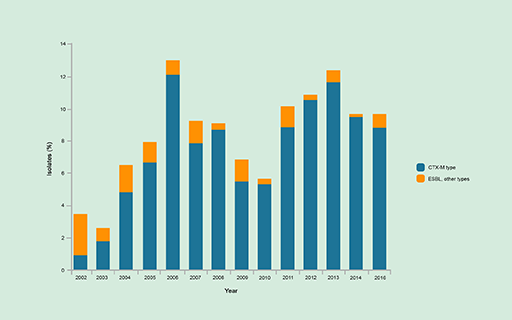
First, look at Figure 11 which shows the percentage of E. coli isolate producing CTX-M-type, or other, ESBLs between 2002 and 2016. Then answer the questions below.
(a) Using the data in Figure 11, how has the proportion of isolates producing CTX-M-type ESBLs changed over time?
Discussion
The proportion of isolates producing CTX-M-type ESBLs was low in 2002 and increased to a peak in 2006. The percentage of resistant isolates decreased between 2007 and 2010 and then began to increase again, peaking in 2013.
(b) CTX-M-type ESBLs emerged in the late 1990s and were first reported in the UK in 2002. Suggest one possible reason for the change in frequency of these ESBLs in the UK over time.
Discussion
The increasing use of cephalosporin antibiotics could create conditions where resistance to cephalosporin antibiotics through the acquisition of CTX-M-type ESBLs is advantageous for the bacteria. Hence these conditions would satisfy Darwin’s conditions for evolution through natural selection.
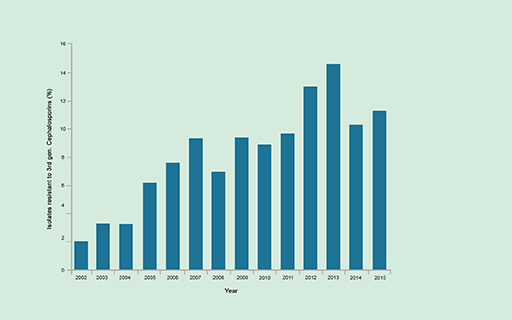
(c) In Activity 7 in Week 1, you looked at how resistance to cephalosporins had changed in the UK over time (Figure 12). By comparing the data in Figures 11 and 12 do you think that the occurrence of CTX-M-type ESBLs is a good indicator of the rate of resistance to cephalosporins?
Discussion
Yes. Patterns of resistance to cephalosporins and the occurrence of CTX-M-type ESBLs were broadly similar between 2002 and 2016. This suggests that CTX-M occurrence is a good indicator of cephalosporin resistance and that the presence of CTX-M-type ESBLs in E. coli is the major cause of cephalosporin resistance.
(d) What challenges might these changes in the prevalence of CTX-M-type ESBLs present to health care?
Answer
The increasing frequency of cephalosporin-resistant bacteria and CTX-M-type ESBLs restricts the treatment options for infections caused by these bacteria.