8 Case study: Neisseria gonorrhoeae
In this week’s case study, you will look at how Neisseria gonorrhoeae, which causes gonorrhoea, is evolving into a superbug. Third-generation cephalosporins, also known as
The next activity will give you an overview of this topic.
Activity 7 Antibiotic-resistant N. gonorrhoeae in the USA
First, watch the following video about the emergence of antibiotic-resistant gonorrhoea in the USA. The video was produced by the USA’s foremost health protection agency – the Centers for Disease Control and Prevention (CDC).
Transcript: Video 5 Drug-resistant gonorrhoea: an urgent public health issue.
Now answer the following questions, based on the video.
- Which two cephalosporins were introduced in the 2000s to treat gonorrhoea?
- When were cephalosporin-resistant N. gonorrhoeae first detected?
- In 2018, only one therapy was recommended for gonorrhoea. What was it?
- Why does the narrator predict that the last treatment option ‘won’t last forever’?
Answer
- Cefixime and ceftriaxone.
- In 2012.
- Dual treatment with ceftriaxone and azithromycin – a macrolide antibiotic.
- N. gonorrhoeae has developed resistance to every antibiotic used to treat gonorrhoea. Reports of isolates resistant to ceftriaxone or azithromycin are expected to become more frequent.
ESC-resistant gonorrhoea has been reported in many other countries, as you will see in the next activity.
Activity 8 ESC-resistant gonorrhoea
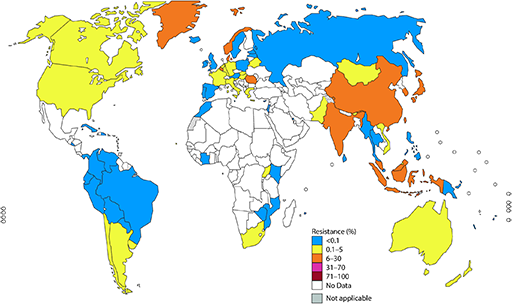
WHO recommends not using an antibiotic in cases where resistance levels are 5% or higher and the bacterial pathogen is unknown. Would this apply to any countries in Figure 12?
Answer
Yes. ESC-resistance is at least 5% in over 20 countries. Using ESCs in these circumstances increases the likelihood of resistance developing and spreading.
Although resistance to ESCs is low level and emerging, resistance to azithromycin is widespread. Gonorrhoea superbugs, which are resistant to ESCs and azithromycin, have already been isolated from Japan, France and Spain.
In the final activity this week, you will look at the scale of the problem and the challenges faced in trying to bring the situation under control.
Activity 9 The rise of antibiotic-resistant gonorrhoea
First, read the article below about the global challenge of treating gonorrhoea effectively because of antibiotic resistance.
Article 1: Antibiotic-resistant gonorrhoea on the rise, new drugs needed (WHO, 2017d). [Tip: hold Ctrl and click a link to open it in a new tab. (Hide tip)]
Now answer the following questions, based on the article.
- How many people become infected with gonorrhoea each year?
- Why is this probably an underestimate?
- What percentage of N. gonorrhoeae isolates are ESC-resistant?
- How many countries have reported resistance to cefixime or ceftriaxone?
- Why might antibiotic resistance increase in the absence of suitable diagnostics?
- How many new drugs are currently being developed to treat gonorrhoea?
Answer
- About 78 million people worldwide.
- LICs, where gonorrhoea is thought to be more common, do not have reliable diagnostic and reporting systems.
- 66%
- Over 50 countries have reported ESC resistance.
- Asymptomatic cases are undiagnosed and untreated, and the infection spreads. Conversely, patients presenting with gonorrhoea-like symptoms may be presumed to have the disease and be prescribed unnecessary or incorrect antibiotics.
- Only three drugs are in clinical development.
Globally, gonorrhoea is becoming increasingly difficult to treat as a result of antibiotic resistance. High infection rates result in high rates of antibiotic use. Inadequate diagnostics and poor monitoring and surveillance of AMR encourage the misuse and overuse of antibiotics. New antibiotics are urgently needed. The threat that gonorrhoea may again become impossible to treat is very real.