6 Case study: cephalosporin antibiotics
In this week’s case study you will learn about the history and development of cephalosporin antibiotics. You might recall from previous weeks that these are broad-spectrum, bactericidal, ß-lactam antibiotics.
The story starts in Italy where the first cephalosporin, cephalosporin C, was discovered in cultures of C. acremonium found growing in a sewer near the Sardinian coast. You can find out more in Activity 5.
Activity 5 The history of cephalosporins
First, listen to the following audio recording about the discovery and development of cephalosporins.
Transcript: Audio 1 Discovery and development of cephalosporins.
Now answer the following questions, based on the audio recording.
- Who discovered the first cephalosporin?
- What antibacterial activity did a crude extract derived from C. acremonium demonstrate?
- Which chemical structure is described as the ‘nucleus’ of cephalosporins and why is it significant?
- What is the difference between the first and later generations of cephalosporins in terms of their spectrum of activity?
Answer
- The Italian scientist Giuseppe Brotzu (1895–1976).
- The extract could suppress the growth of Salmonella typhi and Staphylococcus aureus.
- The starting point for all cephalosporin derivatives (generations) is 7-aminocephalosporic acid, or 7-ACA.
- First-generation cephalosporins are only effective against Gram-positive bacteria. The later generations have increasing activity against Gram-negative bacteria.
Guy Newton and Edward Abraham were interested in cephalosporin C because, although it was a weak antibiotic, it was resistant to ß-lactamase.This is the bacterial enzyme and resistance factor that can inactivate ß-lactam antibiotics.
The drive behind the experiments that resulted in 7-aminocephalosporic acid (7-ACA) was to create a chemically modified derivative of cephalosporin C with enhanced antibacterial activity and intact ß-lactamase resistance. Newton and Abraham found that modifying cephalosporin C could effect the desired change, as long as the 7-ACA ‘nucleus’ containing the ß-lactam ring remained intact (Figure 7).
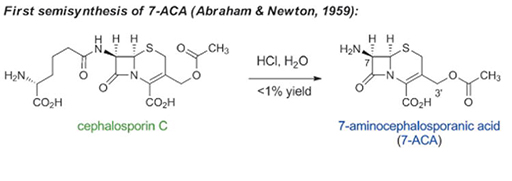
To this day, all cephalosporins are semi-synthetic and are derived from cephalosporin C via 7-ACA. Batch fermentation of the natural antibiotic produces vast quantities of the drug which is converted to the 7-ACA intermediate before being further modified to produce the range of cephalosporins on the market (Wright et al., 2014).
