5.3 Adjuvants
Adjuvants are components of vaccines that enhance their immunogenic potential. In general, they work in one of two ways:
-
They concentrate the antigen in one place (the ‘depot effect’).
-
They activate antigen-presenting cells and induce cytokine production (Figure 8).
The first adjuvants to be devised used antigens in emulsions with aluminium salts, which created depots of antigen and greatly enhanced the levels of antibodies produced in response. Aluminium hydroxide is still added to some vaccines for use in humans, including the diphtheria and tetanus toxoids. Work in animals showed that emulsions containing killed mycobacteria were exceptionally good at producing strong immune responses to other antigens. Mycobacterial products are very effective at activating macrophages and these adjuvants are thought to act by enhancing antigen presentation.
Activity 20
How can bacterial products enhance antigen presentation by macrophages?
Answer
Macrophages have receptors for a variety of bacterial components (including lipopolysaccharide, LPS). Receptor binding to these components causes increased expression of MHC molecules and costimulatory molecules on the macrophage surface, and enhanced secretion of stimulatory cytokines such as IL-1 and TNFa. This upregulation increases the efficiency with which macrophages present antigens to T cells and stimulate T cell activation.
Some bacterial components such as LPS produce adverse local reactions in human recipients, which prevent their use in human vaccines. For example, mycobacteria can cause severe ulceration of the skin, especially in people who have been previously sensitised to them. However, these problems have been overcome in the newer conjugate vaccines (described earlier), which link the antigen irreversibly to bacterial products such as diphtheria or tetanus toxoid, or lipid A. Another technique is to use liposomes, microscopic sacs formed from phospholipids, which trap antigens and ensure that they can be taken up in quantity by antigen-presenting cells. In general, these adjuvants act via the depot effect.
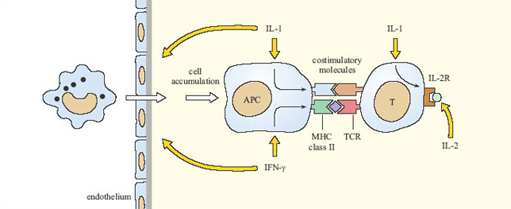
The second category of adjuvants takes a different approach, by incorporating cytokines into the vaccine to enhance the immune response directly. At present (2003) this strategy has been tried in experimental animals, principally using IL-1, IL-2 and IFN-γ, but none have yet been approved for use in vaccines for humans. Figure 8 summarises how these cytokines should (in theory) enhance immune responses to vaccines, although there are many difficulties to be overcome, including the high cost of producing synthetic cytokines.
