Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Thursday, 22 January 2026, 7:06 AM
Communicable Diseases Module: 25. Prevention of HIV Infection, and Community Mobilisation
Study Session 25 Prevention of HIV Infection, and Community Mobilisation
Introduction
In this study session, you will learn about two distinct but interrelated subjects concerning prevention of HIV infection. First, we will describe general prevention measures that individuals can practise in order to avoid or minimise the risk of HIV infection, with particular emphasis on ways to avoid the sexual route of HIV transmission. Secondly, you will learn about a series of steps you should undertake to mobilise your community in the context of HIV prevention. As a result, you will become familiar with ways to facilitate and organise numerous community mobilisation activities at your kebele, in order to both encourage members of different groups in your society to participate actively in HIV prevention measures and, at the same time, create awareness about available services in the higher-level health facilities closest to them. We will also discuss the Ethiopian Federal Ministry of Health (FMOH)’s national strategy for HIV prevention in the context of your work in the community. At the end of this study session, you will be able to relate HIV infection preventative measures at the individual, community and national levels.
Learning Outcomes for Study Session 25
When you have studied this session, you should be able to:
25.1 Define and use correctly all of the key words printed in bold. (SAQs 25.1 and 25.2)
25.2 Describe the basic principles of prevention of HIV transmission. (SAQ 25.1)
25.3 Explain the importance of safe sex as a prevention measure for HIV transmission in the community. (SAQ 25.2)
25.4 Describe the main national HIV community mobilisation strategies, and the processes and steps in community mobilisation. (SAQ 25.3)
24.5 Identify your role in community mobilisation activities related to HIV/AIDS. (SAQ 25.3)
25.1 General principles for preventing HIV infection
The goal of prevention in the context of HIV/AIDS is to avoid or minimise the risk of transmission of HIV from an infected person to an uninfected person. HIV prevention measures currently recommended at the individual and community levels are based on our knowledge of how HIV can be transmitted from person to person.
What are the modes of transmission of HIV?
Through sexual relations; through direct contact with contaminated blood; and from mother to child.

In this section, we will focus on prevention measures that individuals in a community should take in order to avoid HIV transmission through sexual relations and through direct contact with contaminated blood. In later study sessions, you will learn about how to protect yourself against HIV infection in the workplace (Study Session 26) and about specific preventative measures to reduce mother-to-child HIV transmission (Study Session 27).
Provider-initiated testing and counselling for HIV are also important preventative measures for HIV transmission (Study Session 24). Note that the measures described below are aimed at all individuals within a community, whether they know their HIV status or not. Specific issues concerning the prevention of HIV transmission from people living with HIV (PLHIV) to their partners will be discussed in more detail in Study Session 29.
25.1.1 Strategies for preventing sexual transmission of HIV
Sexual transmission accounts for the majority of HIV infection cases in Ethiopia. Remember from Study Session 20 that HIV can be transmitted via blood or sexual fluids (from a man’s penis or a woman’s vagina) through sexual intercourse, which includes vaginal, anal and oral sex. HIV infection may then occur when infected fluids come into contact with the internal linings of someone’s body (usually the vagina, mouth, or anus) through which the virus can enter the bloodstream. Thus, HIV-transmission prevention through the sexual route aims to avoid or reduce contact between blood and/or sexual fluids of an infected person and the internal linings of another person.
The most widely known strategies for prevention of HIV transmission through the sexual route are often known as the ‘ABC rules’:
- ‘A’ stands for ‘Abstinence’, which means refraining from premarital sexual intercourse.
- ‘B’ stands for ‘Be faithful’, which means maintaining faithful relationships with a long-term partner.
- ‘C’ stands for ‘proper use of Condoms’, which means correct and consistent use of condoms in sexual relations.

Abstinence
Abstinence in principle is the most effective way to prevent sexual HIV transmission, as there is no possibility of direct contact between infected blood and/or sexual fluids and another person’s body. Abstinence is therefore a valid option for individuals who do not have a regular sexual partner, or for PLHIV. However, many sexually active people may find difficulties in maintaining abstinence for long periods of time, making it an unrealistic choice. Moreover, the ‘A’ rule excludes the circumstances of forced sexual relations, as in the cases of rape and coercive marriage of young girls, which unfortunately still occur in Ethiopia.
Maintaining faithful relationships
For faithfulness (the ‘B’ rule of Being faithful) to be successful and minimise transmission of HIV, it is essential that both partners, or the multiple partners in polygamous relationships, know whether they are HIV negative before starting unprotected sexual intercourse. Without condoms there are no barriers for the transmission of HIV between partners. Unprotected sexual intercourse refers to all penetrative practices (through vagina, anus or mouth) performed without a condom. Thus, an important role for health workers such as you is to provide HIV counselling and testing to partners before marriage, or before starting faithful relationships (Study Session 24). It is important for them to realise that, if either of the partners has unprotected sex outside the relationship, it is not only they who are put at higher risk of HIV infection, but also their long-term partner.
In addition, remember that people who have recently been infected with HIV may test negative in the rapid HIV tests while they are in the ‘window period’, but they are still able to transmit HIV to others if they practise unprotected sex.
Based on your previous studies, why may some people test negative on a rapid HIV test during the first few months of infection?
Rapid HIV tests detect antibodies against HIV in the blood. The immune system of individuals recently infected by the virus may take a few months to produce enough antibodies to reach levels detected by HIV rapid tests. These individuals might test negative even though they are infected with HIV.
Therefore, it is important to advise individuals who are about to embark on a faithful relationship not to practise unprotected sexual intercourse before their negative HIV status is confirmed by two separate HIV rapid tests performed at least three months apart. Note also that if one or both partners is HIV positive, maintaining faithful relationships will not be sufficient to prevent HIV infection (this issue will be further discussed in Study Session 29).
Forced marriage of young girls, also known as child brides, may make them more vulnerable to HIV infection. Their future husbands may already be infected with HIV, especially if they are much older. In addition, it may be more difficult for young girls to negotiate sexual decisions with their partners such as maintaining faithful relationships, practicing safer sexual practices (see below) and/or demanding HIV testing.
Issues such as these are discussed in more detail in the Module on Adolescent and Youth Reproductive Health.
Safer sexual practices
As discussed above, abstinence and faithfulness to one’s partner(s) are viable alternatives for some individuals to actively reduce their risk of HIV infection. However, safer sexual practices (also know as safer sex) should be actively encouraged for all of your clients who have an active sexual life outside a faithful relationship. Safer sex includes non-penetrative sexual activities and the correct use of condoms. The goal of safer sex is to reduce the possibility of transmitting HIV by minimising exchange of blood or sexual fluids. Practising safer sexual practices also reduces the risk of other sexually transmitted infections or STIs (Study Session 31). Remember from Study Session 20 that the presence of STIs in an individual increases the likelihood of becoming infected by HIV, so safer sexual practices target HIV transmission both directly and indirectly.
The following four points should form the basis of the education you provide in your community about preventing the further spread of HIV:
1. Individuals with multiple partners increase their chances of contracting or spreading HIV (the higher the number of partners, the more likely it is that HIV will be transmitted from person to person). Being faithful to one partner, or multiple partners in a polygamous marriage, decreases the chances of transmitting or contracting HIV.
2. Non-penetrative sexual practices constitute an alternative way to satisfy sexual needs without being at risk of HIV infection. These alternative practices to sexual intercourse include hugging, kissing, rubbing and masturbation, which are all considered to have an extremely low risk of transmitting HIV infection.

What is the most common route of sexual transmission of HIV in Ethiopia? How can this be avoided?
Heterosexual sex is the most common route of HIV transmission in our country, that is anal and/or vaginal penetrative sex between two people of the opposite sex. There are also reports of anal transmission of HIV between men who have sex with men. Avoiding unprotected penetrative sex constitutes an important preventative measure for HIV infection.
3. If penetrative sexual intercourse is the preferred choice, advise clients on the correct and consistent use of condoms, and the importance of using them every time they have sex. Box 25.1 contains important points to remember about condom use that community members can be made aware of through health education or counselling sessions.
Box 25.1 Important points about condom use for safer sex practices
- Use only latex condoms.
- A new condom should be used for each sexual act.
- A damaged condom can allow HIV to be transmitted and should never be used.
- Many condoms have expiration dates and you should always check the package before use.
- Avoid damage to condoms by always using water-based lubricants. Oil-based lubricants, such as Vaseline or creams, can cause condoms to break and should not be used.
All sexually active individuals should be educated on the correct handling of condoms during and after sexual intercourse, as summarised in Box 25.2 and illustrated in Figure 25.1, which follows it.
Box 25.2 Instructions for using a condom during sexual intercourse
- Do not use an ‘out of date’ condom.
- Open the package carefully. Take care not to tear the condom, or damage it with your fingernails.
- Pinch the end of the condom and place it on the erect penis.
- Still pinching the end, unroll the condom right down the penis.
- If you want to use a lubricant, choose one that is water based. Oil-based lubricants can cause condoms to tear.
- After ejaculation, hold the condom and withdraw the penis before it becomes soft. Never re-use a condom.
- Wrap and dispose of the condom in the trash bin, not in a toilet.

Confusion or misunderstandings on how to use condoms correctly are unnecessary risks for HIV transmission. Make sure that patients and clients have clearly understood these instructions.
4. Finally, safer sex practices should be practiced regularly and consistently, that means in every sexual encounter, to prevent HIV transmission effectively.
Do you think it would give added protection against HIV transmission to use a double condom (two condoms, one on top of another) during penetrative sex?
No. Even though you may think that using double condoms would give added protection against HIV infection, there is no evidence that using them is more effective than single condoms. Rather, the use of double condoms may lead to incorrect use of condoms and increased risk of HIV transmission.
25.1.2 Strategies to prevent HIV transmission from contaminated blood
Prevention measures in the community may also be aimed at reducing personal contact with the blood of an HIV-infected person, and/or with objects contaminated with their blood. These may include avoiding the shared use of objects such as a toothbrush and/or sharps (blades, needles, etc.), either in households or in traditional healing; and avoiding harmful traditional practices (uvulectomy, tonsillectomy, milk teeth extraction, female genital mutilation).
Female genital mutilation is discussed in the Module on Adolescent and Youth Reproductive Health.
It is worth noting here that medical blood transfusions are potentially a route for HIV transmission. However, the FMOH has adopted an international standard of quality assurance for blood screening of HIV and other important pathogens. Hence, you need to reassure people in your community that blood transfusions are safe.
25.2 Community mobilisation for HIV prevention
Having discussed strategies that individuals can implement to prevent HIV transmission, we now turn our attention to collective HIV prevention strategies.
25.2.1 What is community mobilisation?
You learnt the basic principles of community mobilisation in the Module on Health Education, Advocacy and Social Mobilisation.
Community mobilisation is a capacity building process through which a community, individuals, groups and organisations plan, carry out and evaluate activities on a participatory and sustained basis to achieve an agreed-upon goal, either on their own initiative or stimulated by others. It uses deliberate, participatory processes to involve local institutions, local leaders, community groups and members of the community to organise for collective action towards a common purpose. Community mobilisation is characterised by respect for the community and its needs.
Community mobilisation for HIV is a process in which a community makes use of its own assets and capacities to prevent and control HIV/AIDS. A community takes ownership of actions with a shared sense of urgency to reduce and reverse the spread of the epidemic. It involves all relevant segments of society in order to create an enabling environment and effect positive behaviour and social change. It also brings together the community to provide care and support to infected, affected and vulnerable individuals; and to increase utilisation of HIV/AIDS services through creation of knowledge and skills at community level.
The daily routine of most people in Ethiopia is closely linked with religious, cultural and traditional values and norms. Formal and informal leaders, religious and other community leaders, have irreplaceable roles in mobilising their community due to their unique spiritual and traditional position. Hence, they have a critical role through community mobilisation, and in challenging traditional values and norms that are counterproductive to the prevention and control of HIV/AIDS.
Clearly, community mobilisation is a key intervention that brings different groups of your community together and uses community resources for shared and agreed action in the prevention and control of HIV.
25.2.2 Basic steps for community mobilisation
Community mobilisation in general involves certain basic steps that can be applied to HIV/AIDS-related community mobilisation efforts. These steps should be taken into account when preparing any type of community mobilisation to realise significant impact. At each level of the community mobilisation process, full participation of all relevant stakeholders is essential for successful community mobilisation. The basic steps of community mobilisation involve the following features:
Defining the problem
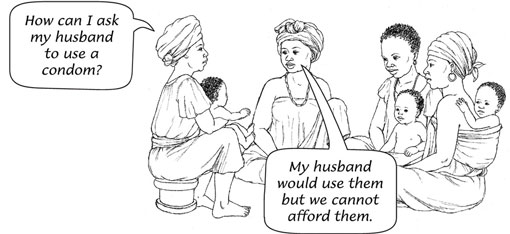
The first step in community mobilisation is to collect the basic information about the issue, in this context the HIV/AIDS epidemic in your community and/or catchment area. This will give you an idea of the extent of the problem and what the underlying causes are. In doing so, you will have a clear statement of the problem and identify the target population in the community affected by it. Traditionally, the most at-risk groups of HIV infection in Ethiopia include female sex workers, uniformed forces, long-distance drivers, migrant labourers and men having sex with men, among others. But it may also include family men who are unfaithful to their wives and will not use condoms, or cannot afford them (Figure 25.2).
Establishing a community mobilisation group
The aim is to establish a group that can influence community mobilisation activities. It usually consists of partners that have a stake in the issue (e.g. PLHIV and/or their families), as well as influential groups and members of the community such as formal and informal leaders and religious and traditional leaders.
Designing strategies, setting objectives and selecting target groups
To achieve a planned change at community level, resources need to be mobilised from the community and other external partners. After obtaining resources, the community mobilisation group should design strategies to address the identified problem with objectives that are SMART, which means Specific, Measurable, Achievable, Relevant and Time-bound. The objectives should be assessed for their impact on the targeted groups in the community.
Developing an action plan with a time line
An action plan links the general community mobilisation plan with time lines for the actual implementation of the planned activities, and the deadlines set for goals to be achieved. This enables the progress of activities to be monitored against the targets set during the planning phase.
Building capacity
Capacity building involves identifying existing capacity resources and assessing the gaps that exist to implement the community mobilisation. The gaps identified should be supplemented by capacity building of the community groups and other relevant stakeholders in the community involved in community mobilisation.
Identifying partners
In the community there are various partners that work independently to achieve similar goals. Therefore, it is important to identify relevant partners through a simple mapping exercise. With respect to prevention and control of HIV/AIDS, for instance, the following partners may be relevant: religious institutions, local non-governmental organisations (NGOs), kebele forums, maheber, idir, woreda HIV/AIDS Prevention and Control Office (HAPCO).
Implementing the plan of activities
Based on the action plans developed with all of the relevant community level partners, implementation of the community mobilisation activities is the main task. In the implementation process, a clear role for any partners that are involved should be put in place and communicated with all of them.
Monitoring and evaluation
Monitoring and evaluation is the last, but essential, element of community mobilisation. It enables you to check whether the action plan has been implemented effectively and the specific objectives are met with respect to the issue the community is mobilised to achieve.
25.2.3 National community mobilisation strategies for HIV
The Ethiopian Federal Ministry of Health (FMOH) advocates community mobilisation approaches for the prevention, control and treatment of HIV/AIDS. In general, this involves conducting an ongoing community dialogue about HIV/AIDS-related problems. Key strategies are to enable the community to establish or strengthen groups of individuals, associations and other community organisations aimed at preventing HIV infection and improving the health and quality of life for PLHIV. Community mobilisation in HIV/AIDS serves its purpose by empowering the community, and creating an opportunity to identify and solve the community’s health problems using their own resources.
The process of engaging with the community at each stage creates locally appropriate responses, and supports the creative potential of communities to develop a variety of strategies and approaches to HIV/AIDS. Bringing various groups of the community together enhances community participation in ways that recognise diversity and equity, particularly of those who are most affected by HIV/AIDS. One of its core values is preventing discrimination and stigmatisation of people infected and affected by HIV/AIDS, and providing continual support.
By utilising influential groups in the community, mobilisation creates a positive model for all behaviours and practices related to HIV/AIDS. It also fosters linking communities with external resources like NGOs and other funding institutions for technical and financial assistance. The FMOH recognises that committing enough time and resources to work with communities and partners is necessary to achieve the goals of community mobilisation for HIV prevention.
25.2.4 Respecting cultural values in community mobilisation
Different groups in the community have different values, norms and beliefs, which require different approaches to address their problems. Community mobilisation brings the community together, and helps to improve community awareness and mobilise community opinion and innovations towards a certain issue like HIV/AIDS. It also invests in the community’s capacity to apply its own resources to prevent diseases and promote better health.
Can you give any examples of community mobilisation activities that you may have participated in, or been aware of, for prevention of communicable diseases?
You may have come across Enhance Outreach Strategy (EOS) for child health, Community Conversation (CC) for HIV prevention, house to house counselling to pregnant women for prevention of maternal-to-child transmission of HIV (covered in Study Session 27), and Indoor Residual Spraying (IRS) for malaria prevention.
In HIV prevention, groups such as those involving the most ‘at-risk’ populations, local traditional associations and influential others, should be systematically mobilised to encourage HIV testing and counselling, and increase access to treatment services. Similarly, it helps to work with influential leaders and programme managers to improve adherence to treatment (Study Session 23).
A targeted HIV prevention programme is one of the key strategies adopted by the FMOH in Ethiopia, so one of the key activities in HIV community mobilisation is identifying the target groups.
Who are the most ‘at-risk’ population groups for HIV in Ethiopia?
The most ‘at-risk’ groups include female sex workers, uniformed forces, long-distance drivers, migrant labourers, and men who have sex with men.
Networking and partnership of all relevant stakeholders is essential, because community mobilisation is a group responsibility and it will be destined to fail if a partner does not take responsibility for their activities. So you need to coordinate and organise the various local and external groups working with you to mobilise the community on HIV control and prevention. When interacting with different influential groups of the community, you need to be politically sensitive, know cultural values, and take into consideration the gender bias that can affect the transmission of the virus. In summary, you should communicate clearly, and be able to facilitate different events together with civil societies and local associations in your community. In all your activities, you must respect cultural values that could affect HIV prevention and control.
25.2.5 Principles of community mobilisation to address HIV/AIDS
You need to recognise the key principles of HIV community mobilisation. They include the following:
- Community ownership and leadership. From planning to evaluating community mobilisation, the local community has to own the initiative and be involved in leadership responsibilities. This ensures sustainability of the programme, and capacity building of local managers and leaders.
- Shared sense of urgency by the target group and members of the community mobilisation groups.
- Involvement of most ‘at-risk’ and targeted populations. In Ethiopia, most at-risk populations include, among others, young people, commercial sex workers, construction workers, uniformed forces, men having sex with men, long-distance truck drivers, and daily labourers migrating from other areas for a commercial work purpose. In mobilising the community for control and prevention of HIV, these groups have to be actively involved in all steps of the process.
- Involvement of PLHIV. Maximising the involvement of PLHIV in both prevention and care interventions is important in reducing stigma and discrimination. It also ensures that PLHIV have an active role in HIV prevention and control activities.
- Evidence-based and result-oriented plans. HIV prevention plans should be clear in that they should address what needs to be done, by whom, when it should be completed, and how it is done. They should be based on clearly identified problems and on evidence-based solutions. They should also be accompanied by learning from the process of activities to be implemented, through monitoring and evaluation of the overall initiative.
- Coordinated effort and strong partnership. Coordination of all involved, with clear roles and responsibilities of partnership, is also important. You should play a lead role in bringing community groups together, and maintaining a healthy partnership for a common goal.
25.2.6 Community mobilisation activities for preventing HIV/AIDS
Below are common community mobilisation activities that you should undertake in your community:
- Mobilise local individuals, institutions and community groups including idir, maheber, iqub, anti-AIDS clubs, peer support groups, women’s support groups, religious groups, and other local civil society groups.
- Lead community conversation activities in your kebele. Community conversation is a key community mobilisation strategy advocated by the FMOH for different programmes, including the HIV prevention and care programme, and child and maternal health issues. The details of community conversation are not discussed here. You need to refer to the national guidelines for community conversation to have an in-depth insight and knowledge about how to use it in your community.
- Transmit HIV prevention messages through different forums like anti-AIDS clubs, student groups at schools, HIV associations, mothers’ groups and other civil associations.
- Help the community share best experiences from other communities and model families in their community.
- Build the capacity of voluntary community health workers who can facilitate community conversations and refer mothers for PMTCT (Study Session 27).
- Facilitate and hold local anti-HIV/AIDS festivals and events such as coffee ceremonies.
- Mainstream your community mobilisation activities for HIV prevention in local associations and governmental organisations at different levels.
- Sign contractual performance agreements on the joint implementation of community mobilisation plans and goals with various external and local partners.
Community conversation is described in detail in the Module on Health Education, Advocacy and Community Mobilisation.
Summary of Study Session 25
In Study Session 25, you have learned that:
- The main ways to prevent sexual HIV transmission among adults are abstinence from premarital sexual intercourse, faithfulness to a partner, and correct and consistent use of condoms, often termed the ‘ABC rules’.
- Discussion on safer sexual practices for sexually active people should include decreasing the number of partners, and consistent and regular non-penetrative sexual practices, and/or use of condoms for penetrative sex.
- Prevention of HIV transmission via contaminated blood involves avoiding contact with objects potentially contaminated with blood, and reducing unsafe and/or harmful traditional practices.
- Community mobilisation is a process through which community, individuals, groups and organisations plan, carry out and evaluate activities on a participatory and sustained basis to achieve an agreed-upon goal, either on their own initiative or stimulated by others.
- Community mobilisation in general involves certain basic steps, including defining the problem, designing and evaluating strategies, setting objectives, selecting target groups, and identifying partners. These also apply to HIV/AIDS-related community mobilisation efforts.
- The national HIV prevention strategy generally involves conducting an ongoing community dialogue about HIV/AIDS-related problems to create awareness and stimulate behavioural change.
- Active involvement of most ‘at risk’ populations and PLHIV are integral in the effort to maximise community mobilisation for HIV prevention.
Self-Assessment Questions (SAQs) for Study Session 25
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the following questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 25.1 (tests Learning Outcomes 25.1 and 25.2)
Which of the following is not a strategy to prevent transmission of HIV? Explain your answer.
A Providing information on ABC rules of safer sex to clients.
B Providing information on prevention of mother-to-child HIV transmission.
C Provider-initiated HIV testing and counselling.
D Implementing HIV infection prevention measures at your health post.
E Not mobilising your community to reduce harmful traditional practices such as uvulectomy.
Answer
E is incorrect. Harmful traditional practices such as uvulectomy promotes sharing of sharp objects contaminated with blood, and hence facilitates HIV transmission. All the other statements are good ways to prevent HIV transmission.
SAQ 25.2 (tests Learning Outcomes 25.1 and 25.3)
A young couple who do not know their HIV status have been using condoms for six months and then started to practise unprotected penetrative sex because they felt that they were in a faithful relationship. What would you advise them?
Answer
You should inform them that maintaining faithful relationships is effective for HIV prevention only if both partners are confirmed HIV-negative. You should provide counselling for HIV testing and inform them about the consistent use of safer sex practices, including the correct and regular use of condoms in every sexual encounter for couples who are not tested for HIV.
Read Case Study 25.1 and then answer the questions below it.
Case Study 25.1 Community mobilisation for HIV prevention
You are working as a Health Extension Practitioner in one of the rural kebeles but close to a semi-urban town. Though the prevalence of HIV in your kebele is lower than the national average, the prevalence in the small town near your kebele is 10%. Recently, a private road contractor has started to build the main road to Addis Ababa in your region. They have built many camps for the daily labourers working for the construction company near your kebele. In addition, trading women come to the camp area from the small town, as well as from other areas, to serve the daily labourers.
SAQ 25.3 (tests Learning Outcomes 25.4 and 25.5)
- a.What steps would you plan to mobilise your community to prevent an increase in HIV transmission?
- b.Who would be your target groups for the community mobilisation programme?
- c.Who are your potential partners for this community mobilisation?
- d.What HIV prevention strategies will you be implementing?
Answer
- a.You may use the standard steps of community mobilisation, though you can modify or skip some of them depending on the availability of time and resources. You should consider the following:
- Clearly define the problems, including the causes, by gathering information about ways that HIV transmission could increase.
- Identify and establish community mobilisation groups from the community, kebele and woreda offices, and local charity organisations if they exist.
- Design your HIV prevention strategies.
- Plan the list of activities that you will implement in a certain time period.
- Identify all of your partners and their roles, including community mobilisers, target groups and other external partners.
- Implement your activities based on your designed HIV prevention strategies.
- Monitor and evaluate your implementation results, comparing it to your plan.
- b.The target groups for your community mobilisation could be:
- sex workers
- trading women
- daily labourers
- clients of sex workers
- the construction company workers.
- c.Your potential partners could be:
- formal and informal kebele leaders
- woreda HAPCO
- local associations of PLHIV support groups
- HIV/AIDS clubs
- charity organisations
- the construction company management team
- Ethiopian roads authority.
- d.HIV prevention strategies at community level may include:
- behavioural change communication using health education and other methods
- community condom distribution
- HIV prevention campaigns
- outreach peer education
- life skills training for vulnerable women.