Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Sunday, 8 March 2026, 6:32 AM
Communicable Diseases Module: 26. Universal Precautions, Infection Prevention and Post-Exposure Prophylaxis for Health Workers
Study Session 26 Universal Precautions, Infection Prevention and Post-Exposure Prophylaxis for Health Workers
Introduction
So far, in this part of the Module, you have learnt many important topics concerning HIV and AIDS. This study session gives you the opportunity to learn about another aspect of this condition, which is especially important to you in your work as a Health Extension Practitioner. In particular, you will learn about:
- the basic principles and procedures of universal precautions
- infection-prevention methods in healthcare settings
- post-exposure HIV prophylaxis
- measures to be taken when a healthworker suffers a needle-stick injury
- referral for post-exposure prophylaxis for someone who has been raped.
You need to learn about infection prevention because the procedures to be described are very important for your daily work in the health post, and in the community at large. In particular, the guidance we give here will mean that you are unlikely to become infected with HIV and other blood-borne infectious agents through occupational exposure during your work as a Health Extension Practitioner.
Learning Outcomes for Study Session 26
When you have studied this session, you should be able to:
26.1 Define and use correctly all of the key words printed in bold. (SAQs 2.1 and 26.3)
26.2 Describe the basic principles and standard procedures of universal precautions to prevent exposure and transmission of blood-borne infectious agents. (SAQ 26.1)
26.3 Describe the standard procedures for giving safe injections to prevent occupational exposure to infectious agents. (SAQ 26.2)
26.4 Explain the principles of post-exposure prophylaxis. (SAQ 26.3)
26.5 Assess the risks of HIV infection following accidental occupational exposures. (SAQ 26.4)
26.6 Describe the measures that should be taken when a healthcare worker suffers a needle-stick injury. (SAQ 26.4)
26.7 Explain how you would refer someone who has been raped for post-exposure HIV prophylaxis. (SAQ 26.5)
26.1 Universal precautions
The term universal precautions (UP) refers to the standards of infection control developed to prevent exposure and transmission of blood-borne infectious agents like HIV and hepatitis virus. In some texts you will find them referred to as ‘standard procedures’, because they should be routine in all contacts with patients. The universal precautions that are described here should be implemented and practised at all times by all healthcare providers and caregivers in all settings, in particular in hospitals, health centres, health posts and community settings, as well as in the homes of your patients.
Standard procedures is the term used in Part 2 of this Module in the prevention of occupational exposure to tuberculosis.
26.1.1 Why are universal precautions needed?
Universal precautions were developed because it is not possible to identify all patients with blood-borne diseases caused by microorganisms. With many of the patients you are looking after, there is no risk of HIV transmission. So, it is not appropriate to routinely test every health worker or patient for HIV. However, increased risks are faced by healthcare workers when providing care to HIV-positive patients, or those infected with other blood-borne agents such as the hepatitis virus. It was in response to such concerns that UPs were developed — the term ‘universal’ reflects the fact that they are intended to refer to contact with all patients, not just those known to have blood-borne infections.
UPs are designed to provide for the safe handling of infectious material, including amniotic fluid, cerebrospinal fluid, pleural fluid, abdominal fluid, serum, semen, vaginal fluids, blood and blood-tainted body fluids. As part of this process, barriers to infection were developed, such as gloves, gowns, masks and eye goggles to protect health workers from splashes or sprinkles of infectious materials. The procedures summarised below are designed to keep all healthcare workers safe, and to protect the public against infectious waste material that could pose a risk to them. Safety involves not just patient contact, but the management of the environment in which the patient is situated. Note that, with universal precautions, everyone is considered infectious, since it is impossible to tell ahead of time who is infected and who is not.
26.1.2 Specific universal precautions
Universal precautions include the following measures and actions:
- Increased attention to the correct handling of sharps and all infected materials. The safe disposal of sharps (e.g. needles, scalpels, lances and suture materials) is relatively easy to achieve. Home-made containers that have an open top, firm sides, and are made of durable materials, can be used as containers for used sharps (Figure 26.1).
![]() Never fill a safety box beyond three-quarters full. Beyond this point you risk an injury when adding more sharps to the box!
Never fill a safety box beyond three-quarters full. Beyond this point you risk an injury when adding more sharps to the box!
- Safe disposal of waste contaminated with blood or body fluids. Contaminated clinical waste includes used bandages, dressings, and linens or materials contaminated with blood or body fluids; these must all be handled with gloved hands and placed in containers for safe disposal, as shown in Figure 26.2.

- Hand washing with soap and water before and after all procedures. This is the single most important step that all healthcare workers can take to ensure the safety of their patients and themselves. You must wash your hands before and after putting on gloves, and before and after you move from one patient to another.
- Use of protective barriers (personal protective equipment or PPE) when in direct contact with potentially infected body fluids. Protective barriers such as gloves, gowns, masks and goggles protect healthcare workers from occupational exposure to infectious material (see example in Figure 26.3). Gloves provide an important barrier between infectious material and the healthcare provider. Using gloves does not mean that you don’t have to wash your hands.

- Proper disinfection of instruments and other contaminated equipment. In an effort to make universal procedures routine, more emphasis is put on preventing the transfer of infection from one patient to another by proper disinfection of instruments and contaminated equipment.
26.2 The safe injection of patients
A common source of injury for healthcare workers is poor practise when giving injections. This section shows the standard procedures for giving an injection, designed to ensure your safety and that of your patient when giving injections in the health post and in the patient’s home.
26.2.1 Preparing to give an injection
Using a new sterile syringe and needle for each injection is one of the most effective ways to prevent the spread of blood-borne infections.
- Use a new packaged sterile syringe and needle for every injection.
- Inspect the packaging very carefully. Discard a needle or syringe if the package has been punctured, torn or damaged in any way.
- Check the expiry date on the package. Never use needles or associated injection materials that are ‘out of date’.
- Prepare injections in a clean designated area or on a clean surface; in a patient’s home you will need to use a clean dish or tray that you have washed in soap and water, left to air dry and then swabbed with alcohol before laying out the injection equipment.
- Prepare each dose immediately before administering; do not prepare several syringes in advance.
- Do not touch the needle. Discard a needle that has touched a non-sterile surface.
26.2.2 Avoiding needle-stick injuries
A needle-stick injury refers to a healthcare worker accidentally puncturing their own skin with a needle that has previously been used to inject a patient. Needle-stick injuries can occur at any time, but they happen most frequently during and immediately after an injection is given. They can also occur when needles are not disposed of in safety boxes, for example when a healthcare worker picks up contaminated waste in which a needle has been left unnoticed.
In general, the more injection equipment that is handled, the greater the risk of needle-stick injuries. But these injuries are preventable. Box 26.1 lists the simple steps you can follow to reduce the risk of needle-stick injuries.
Box 26.1 Steps to reduce the risk of needle-stick injuries
- Handle needles and syringes as little as possible; avoid recapping the needle after use, and do not remove a used needle from the syringe.
- Handle needles and syringes safely; ensure you wear suitable gloves, and avoid recapping needles (Section 26.2.3 gives more details).
- Set up the injection preparation area so as to reduce the risk of injury. A safe work area for a clinic is shown in Figure 26.4.
- Position the patient, especially children, correctly for injections. (You will learn how to give injections via different routes of administration in the Module on Immunization, and in your practical skills training.)
- Place a safety box close to where the injections are being given, so that used syringes and needles can be disposed of immediately. Practise safe disposal of all contaminated sharps and waste.

26.2.3 Recapping used needles
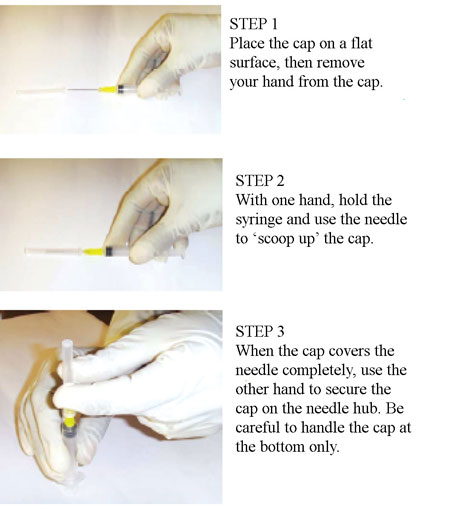
Although you should not recap needles routinely, you may need to recap a needle to avoid carrying an unprotected sharp when immediate disposal is not possible, or if an injection is delayed because a child is agitated. If it does become necessary for you to recap a used needle, follow the one-handed recapping technique (also called the single-handed scoop method) illustrated in Figure 26.5.
26.3 Post-exposure prophylaxis (PEP)
The most effective (and cheapest) way to deal with exposure to disease-causing agents is prevention, so the implementation of universal precautions, with appropriate training and monitoring should be your immediate priority. However, although universal precautions will decrease the occurrence of occupational exposure, ‘accidents’ and unanticipated exposures will sometimes occur, and it is essential to know how to deal with them.
Chemoprophylaxis means using drugs to prevent a disease from developing in the first place. Post-exposure prophylaxis (PEP) for HIV means taking antiretroviral medication (ARVs were described in Study Session 22) as soon as possible after a possible occupational exposure to HIV, so that the exposure will be less likely to result in HIV infection. PEP is also provided after rape to prevent possible HIV transmission. Due to the psychosocial impact of HIV/AIDS, and the fact that the disease is not curable, PEP for HIV is made freely available in Ethiopia.
![]() Note that you cannot prescribe ARVs for PEP. You must refer such cases to health centres providing ARVs as a matter of urgency.
Note that you cannot prescribe ARVs for PEP. You must refer such cases to health centres providing ARVs as a matter of urgency.
What does occupational exposure mean?
Occupational exposure means coming in contact with infectious agents whilst carrying out your duties as a healthcare worker.
Examples of occupational exposure to HIV are needle-stick or other sharps injuries, a splash of infected body fluid into the eyes or onto cracked skin, bites and sexual assaults by infected patients. Procedures such as gynaecological examinations, spinal taps, labour and delivery, and surgery can also place the healthworker at risk. Splash exposure carries a lower risk than a needle-stick injury, but it should be taken seriously in both the workplace and the patient’s home.
For healthcare workers, PEP usually relates to exposure to HIV or hepatitis virus, but we will only deal with HIV exposure here. (Note: you learnt about hepatitis B in Study Session 4.) The risk of transmission of HIV after accidental occupational exposure is about 100 times less than the risk of occupational transmission of the hepatitis B virus.
26.3.1 Risks of HIV infection after accidental occupational exposures
Transmission of HIV is estimated to occur in about 1 in 300 cases of occupational exposure. The factors that increase the risk of transmission of HIV after an occupational exposure are if:
- exposures are deeply penetrating, as opposed to superficial splashes onto mucus membranes (e.g. broken skin, mouth, eyes).
- the injury is caused by a device that was in an artery or vein in the infected person.
- blood is visible on any device involved in the exposure.
- exposure is to a large volume of blood, or other potentially infectious fluids, such as blood plasma, pus or cerebrospinal fluid (from a spinal tap).
- the injury is caused by wet instruments, which have a much higher risk of transmission than with dry instruments.
- hollow bore needles are involved in the exposure; they are more likely than solid needles to bring about transmission of HIV.
- gloves are not used while preparing and giving injections.
- the ‘source patient’ has advanced HIV disease, taking into account factors such as the clinical stage of the illness, the extent of virus circulating in the blood, and the presence of antiretroviral drugs in their blood. The level of risk relates to the number of viruses present in the infected blood or body fluid involved in the exposure.
Hollow bore needles are used as intravenous (IV) needles or canullae, or to give drug injections. Solid needles are those used in suturing wounds.
From the above list, can you identify circumstances in which the risk of HIV transmission after an occupational exposure will be reduced, relative to these higher-risk criteria?
The risk will be lower if the exposure is onto mucus membranes, not deeply penetrating, or involves body fluids other than blood; and also:
- if the device is dry;
- it is not previously in the patient’s vein or artery,
- and/or blood is not visible on the device;
- the device is a solid (not hollow bore) needle;
- the amount of blood transferred is very small;
- gloves are worn;
- the patient is not in an advanced stage of HIV disease.
26.3.2 Immediate actions after occupational exposure to HIV
The following measures should be taken immediately after an accidental occupational exposure to a possible source of HIV infection.
Care of the exposure site
Wash the wound from a needle-stick or other sharps injury with soap and water, and let it bleed freely. The wound should be irrigated (flushed) with sterile saline and a disinfectant. Exposure to mucosal membranes (e.g. broken skin, mouth, eyes) should be dealt with by washing the affected area thoroughly with clean water, sterile saline or sterile eye irrigant from an eye-wash bottle.
Assessing the exposure risk
The level of risk will depend on the type of injury as described in Section 26.3.1 above.
Testing the source of the exposure
If the HIV status is unknown, a rapid HIV test should be performed on the individual or patient who is the source of the exposure, after counselling and consent has been secured. If the source is found to be HIV negative, there is no need for further assessment of the exposed healthcare worker. If the result is positive, the healthcare worker needs to be HIV tested.
Testing the healthcare worker
A rapid HIV test should be performed on the healthcare worker immediately after exposure. If the result shows that the healthcare worker is already HIV positive PEP cannot help them. If the test is negative then the healthcare worker should be administered PEP as described below. The HIV test should be repeated at six weeks, three months, and six months after exposure. If, as a consequence of these repeat tests, the healthcare worker is found to have become HIV positive, then they will be assessed for HIV care and treatment.
Following exposure to HIV, there is a need for psychosocial support and counselling on safer sexual practises. If ARVs are prescribed, close monitoring will need to follow to support adherence and identify any adverse side-effects of treatment (as described in Study Sessions 22 and 23).
Why should the HIV test be repeated at intervals up to six months after the exposure?
It takes up to three months before the body of a person newly infected with HIV produces enough anti-HIV antibodies to be detectable in an HIV rapid test. This is called the ‘window period’. A negative test result during this period cannot be taken as evidence that the exposure did not transmit HIV.
Starting PEP
![]() You must refer yourself, or any health worker you witness suffering a sharps injury from a contaminated instrument, or a splash exposure to their mucus membranes, as quickly as possible to an appropriate health facility.
You must refer yourself, or any health worker you witness suffering a sharps injury from a contaminated instrument, or a splash exposure to their mucus membranes, as quickly as possible to an appropriate health facility.
If you suffer an occupational exposure to blood or body fluids from any patient, you should seek PEP immediately, even before the HIV status of the source is known. To be effective, PEP has to be started as soon as possible, ideally within one to two hours after exposure. It is not worth undertaking PEP beyond 72 hours after the exposure, because by this time, if the virus has been transmitted, it will have entered the person’s bloodstream. PEP cannot prevent it from circulating around the body and possibly causing HIV infection. A standard course of PEP will normally last for 28 days. It can be provided only by trained nurses, health officers or physicians at health facilities offering antiretroviral therapy (ART). Most of the health centres and hospitals offer PEP services.
26.4 Referral after rape for post-exposure HIV prophylaxis
Rape is a major crime that could happen in your community, and you need to be prepared to support the victims, both in terms of their mental health and their physical health. Cases are treated according to the Ethiopian law for rape management, and anyone who suffers a rape or other penetrating sexual assault should be referred for post-exposure prophylaxis in case the rapist was infected with a blood-borne disease such as HIV or hepatitis. Since police procedures may take time, you have to urge the raped person, and whoever is caring for them, to go immediately to a health centre or hospital that provides PEP. Currently, all ART sites provide this service, as should most of the health centres in your catchment area.
Anyone who has been raped should be counselled by the examining healthcare worker about the potential risks of HIV infection (Figure 26.6). Under these circumstances, the HIV status of the rapist should be considered as ‘unknown’, and therefore HIV transmission is a potential risk. Parents or guardians of traumatised children or adolescents should also be counselled and informed about the risk of HIV infection after a sexual assault.

Points to be covered in counselling after a rape include:
- The precise degree of risk of HIV transmission is not known, but it exists.
- HIV testing is very important, and should be made clear to the person who has been raped and their caregivers, but explain that testing cannot give a confirmed negative result until after the window period is over.
- The raped person can choose to be tested for HIV immediately. However, if they refuse, testing can be delayed until 72 hours after the initial examination visit.
- The management guidelines on sexual assault provide for a three-day starter pack of PEP for those who prefer not to be tested immediately, or those that are not ready to receive the results immediately.
PEP is not recommended if the person presents to a health facility later than 72 hours after the sexual assault. They should be counselled about the possible risk of infection, and the possibility of transmitting infection to another person during the window period. They should be told to return after six weeks and three months for further HIV testing and counselling.
Why is PEP not recommended if a person presents to a health facility more than 72 hours after a sexual assault?
Because by this time the virus has entered the bloodstream, and PEP given more than 72 hours after exposure is not effective. Ideally, PEP has to be started within one to two hours after exposure. If this is not possible, it should be started within the first 72 hours.
A person who undergoes PEP after a sexual assault should be carefully evaluated for psychosocial support and monitored for any adverse side-effects of PEP treatment. They should also be screened for other sexually transmitted infections and referred for treatment as appropriate.
Summary of Study Session 26
In Study Session 26, you have learned that:
- Universal precautions should be practised by all healthcare providers to reduce the risk of exposure and transmission of blood-borne infectious agents like HIV and hepatitis virus.
- The most important infection control method is thorough hand washing with soap and water.
- Correct handling and disposal of sharps is critical for reducing occupational exposure to blood-borne infectious agents.
- The level of risk of HIV transmission after an occupational exposure varies depending on the source of the contamination, the type of injury, and the clinical stage of the infected individual.
- Referral for PEP should occur immediately if a healthcare worker is exposed to blood or body fluids from any patient, without first waiting for the patient to be HIV tested.
- PEP should begin ideally within 1–2 hours of exposure, or up to 72 hours afterwards. It is not effective if begun after 72 hours.
- After a sexual assault, the victim (and/or the parents or guardians) should be counselled about the importance of HIV testing. If an HIV test is refused initially, a three-day starter pack of PEP can begin.
- Counselling is on the risks of HIV transmission, psychosocial support, and the need to return for repeat testing after six weeks and three months; follow-up should monitor the effects of PEP.
Self-Assessment Questions (SAQs) for Study Session 26
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the following questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 26.1 (tests Learning Outcomes 26.1 and 26.2)
State if the following statement is true or false. Explain your reasoning.
‘Universal precautions are used only with very sick patients.’
Answer
The statement is false because universal precautions are standard procedures used when we manage all patients. Universal precautions should be implemented and practised by all healthcare providers and caregivers in all settings, in particular in hospitals, health centres, health posts and community settings, as well as the homes of your patients.
SAQ 26.2 (tests Learning Outcome 26.3)
Which of the following statements about the standard procedures for giving safe injections is false? In each case, explain what is incorrect.
A The more you handle an injection instrument, the more skilful you will become at avoiding the risk of needle-stick injury.
B Place a safety box close to the person giving injections, so used syringes and needles can be disposed of immediately.
C Do not manually remove a used needle from the syringe.
D Do not carry used syringes and needles around with you.
E Avoid recapping the needle after you have given an injection.
F Close the safety box when it is full, and start a new one.
Answer
A is false. The more you handle an injection instrument, the more likely you are to suffer a needle-stick injury.
B is true. Place a safety box close to the person giving injections, so used syringes and needles can be disposed of immediately.
C is true. Do not manually remove a used needle from the syringe.
D is true. Do not carry used syringes and needles around with you.
E is true. Avoid recapping the needle after you have given an injection.
F is false. Safety boxes should be closed when they are three-quarters full; you risk a sharps injury if you try to add needles or other instruments to a full safety box.
SAQ 26.3 (tests Learning Outcomes 26.1 and 26.4)
State if the following statement is true or false. Explain your reasoning.
‘If a health facility has all the personal protective equipment (PPE), the healthcare workers in that facility do not need a post-exposure prophylaxis (PEP) service.’
Answer
The statement is false. Remember that although universal precautions will decrease the occurrence of occupational exposure, there are ‘accidents’ and unanticipated exposures, which necessitate PEP for HIV. Even if a health facility has all the PPE, it needs a PEP service for its healthcare workers to prevent HIV transmission through accidental occupational exposure. If PEP is not available in a health facility, or when there is nobody trained in how to manage such cases, referral of the exposed health worker to a nearby health facility which has a PEP service should be arranged as soon as possible.
Read Case Study 26.1, and then answer the questions that follow.
Case Study 26.1 Ayelech’s story
Ayelech is a healthcare worker trained to provide a safe and clean delivery service (this is covered in the Labour and Delivery Care Module). One day she was attending a delivery in a household in her catchment area. The mother had been sick for about two months before the delivery with diarrhoea on and off, but she had persistently refused Ayelech’s counselling to be tested for HIV. Ayelech didn’t use any personal protection equipment for the delivery except gloves. After the delivery, she injected the mother with intramuscular (IM) oxytocin to help deliver the placenta and prevent excessive bleeding. Ayelech was trying to recap the needle with two hands, when she accidentally pricked her left index finger with the needle. Her finger was bleeding and it was a deep needle-stick injury, but the placenta was coming and the baby needed attention, so she ignored the injury.
SAQ 26.4 (tests Learning Outcomes 26.5 and 26.6)
- a.Was Ayelech following universal precautions? Say why or why not.
- b.Is there a risk that Ayelech could be infected with HIV? If so, what is the degree of the exposure?
- c.Explain what she should have done immediately after the injury.
- d.Explain what Ayelech should do next.
Answer
- a.No, Ayelech was not following universal precautions, because she didn’t use PPE except for wearing gloves. She also recapped the needle with two hands, instead of with one hand.
- b.Yes, Ayelech is at risk of being infected with HIV. The HIV status of the mother is not known, but the fact that she was sick makes the possibility of HIV infection more likely. It is a high-risk exposure since the needle-stick was a deep injury with a hollow needle, and the mother was sick.
- c.Immediately after the injury, Ayelech should wash the wound with soap and water and let it bleed freely. There should be antiseptic or disinfectant in the bag she takes to deliveries, and she should flush the wound with it.
- d.Ayelech should call for help for the mother and newborn, and go to the nearby health centre/hospital as soon as possible to begin PEP immediately. Ayelech should also be tested for HIV. If she is found to be positive, she doesn’t need the PEP and should be enrolled for HIV care at the health centre.
Read Case Study 26.2, and then answer the questions that follow.
Case Study 26.2 Fatuma’s story
While working in your health post, Fatuma, a 15 year-old girl, arrives with her parents. They have brought her because six hours earlier she was raped by a man whose HIV status is not known.
SAQ 26.5 (tests Learning Outcome 26.7)
- a.What do you tell Fatuma and her parents first?
- b.What will be the final advice you give to them?
Answer
- a.You should first tell Fatuma and her parents about the potential risk of HIV infection from the sexual assault, and explain that Fatuma should get PEP quickly, which you don’t have in your health post.
- b.You should refer Fatuma immediately to the nearby health centre or hospital for physical examination, PEP, and other necessary investigations and medications. You need to convince Fatuma and her parents that the legal process is a lower priority, as she has to take the PEP within 72 hours of the assault.