Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Thursday, 22 January 2026, 7:06 AM
Communicable Diseases Module: 38. Common Zoonotic Diseases in Ethiopia: Rabies and Taeniasis
Study Session 38 Common Zoonotic Diseases in Ethiopia: Rabies and Taeniasis
Introduction
In the last two study sessions in this Module, you learned about vector-borne diseases in which the infectious agent is transmitted to new human hosts by body lice, flying insects or snails. In this study session, we turn to two communicable diseases found in Ethiopia in which a non-human warm-blooded animal transmits the infectious agent to humans. These diseases are rabies transmitted to humans by dogs, and taeniasis (or tapeworm disease) transmitted by cows. Diseases in which a warm-blooded animal transmits the infectious agents to humans are known as zoonotic diseases (or zoonoses).
Taeniasis is pronounced ‘teen-eye-assis’. Zoonotic is pronounced ‘zoo-nott-ik’.
Zoonotic diseases are difficult to control because the non-human animal acts as a reservoir of infection that can be passed on to humans. Dogs and cows are domestic species, living in large numbers in human settlements (Figure 38.1), where it is very easy for the infection to be transmitted to people. In this study session, you will learn about the causes, modes of transmission, clinical manifestations, and the prevention and control measures against these two zoonotic diseases – rabies and taeniasis.

Learning Outcomes for Study Session 38
When you have studied this session, you should be able to:
38.1 Define and use correctly all of the key words printed in bold. (SAQs 38.1, 38.2 and 38.3)
38.2 Describe the mode of transmission of rabies and taeniasis to humans by their animal hosts. (SAQs 38.1, 38.2 and 38.3)
38.3 Describe the symptoms and diagnosis of rabies and taeniasis and state how you would treat or refer cases to a higher level health facility. (SAQs 38.1, 38.2 and 38.3)
38.4 Describe how you would apply prevention and control measures against rabies and taeniasis. (SAQs 38.2 and 38.3)
38.1 Rabies
Rabies is a severe life-threatening viral disease, transmitted to humans in saliva in the bite of infected animals, particularly those in the dog family (canines). Foxes, wolves, hyenas, bats, raccoons and skunks are also a reservoir of rabies virus, but in most countries they rarely transmit the disease. Bats are the main cause of rabies transmission in the USA and Canada.
The infectious agent of rabies is a virus in the rhabdovirus family, which attacks the nervous system. If an infected person is not treated very quickly, death is almost inevitable (i.e. rabies has a very high case-fatality rate). The WHO estimates that around 55,000 people die from rabies every year, and 24,000 of them are in Africa; 99% of these deaths are the result of a bite from a dog (Figure 38.2).

38.1.1 The transmission of rabies in Ethiopia
Rabies is one of the most severe communicable diseases in Ethiopia, with many cases of the disease diagnosed in many parts of the country. For example, a study in Addis Ababa showed that about 73% of street dogs are infected with rabies virus and more than 2,000 people annually received treatment for rabies after a dog bite. Children are particularly vulnerable to being bitten by dogs, and about 40% of all cases are children under 15 years.
The rabies virus exists in the saliva of the infected animal (as well as in its nervous system) and is transmitted to a person through a bite. Transmission can also be if an infected animal licks a fresh break in the person’s skin or mucus membranes, e.g. in the mouth (see Table 38.1 later, for different exposure categories). The virus travels in the nerves to the brain, where it causes inflammation. Person-to-person transmission is theoretically possible if someone with advanced rabies bites another human, but this is not known to have occurred.
38.1.2 Clinical manifestations and diagnosis of rabies
From the site of the bite, the virus goes to the central nervous system (Figure 38.3) and causes the clinical manifestations which, if untreated, eventually lead to death. Rabies has the highest case-fatality rate of any communicable disease. After an incubation period usually lasting one to three months, but sometimes even up to one year after the bite, the patient develops symptoms that are similar to many other illnesses – fever, headache and general weakness. The speed of progression is faster if the original site of infection was in an area of the body that is close to the spinal cord or brain, e.g. a bite on the face or hands. As the disease gets worse, the patient experiences anxiety, confusion, difficulty sleeping, hallucination (seeing things that aren’t there), spreading paralysis (inability to move the muscles), difficulty swallowing and convulsions (uncontrollable shaking). A characteristic sign of late-stage rabies in some patients is hydrophobia (fear of water), which manifests in the patient reacting in terror if a bowl of water is brought near. This form of the disease (known as ‘furious’ rabies) prevents the patient from drinking and speeds the arrival of death within a few days. Other patients become increasingly paralysed and lose consciousness before death.

Diagnosis is made on the basis of these clinical signs. There are no tests to confirm rabies with absolute certainty while the patient is still alive. Viruses can be detected by laboratory investigation of the patient’s brain after death, but this test is not usually carried out in countries with few resources.
38.1.3 First aid and post-exposure prophylaxis for rabies
Wound care and anti-rabies treatment after a dog bite can reduce the occurrence of rabies in a bitten person by up to 90%. This is what you should do if someone is bitten by a dog in your kebele.
First aid
Immediately after a dog bite, you should thoroughly clean and flush the wound with soap and water, detergent, or a substance that kills viruses such as 70% alcohol, tincture of aqueous solution of iodine, or povidone iodine. Continue flushing the wound for at least 15 minutes. The wound should not be sutured (stitched) unless this is essential to stop heavy bleeding. If stitches are required, the wound should not be sutured until after post-exposure prophylaxis has occurred.
Post-exposure prophylaxis for rabies
If a person is bitten by a dog in countries where rabies is endemic, there is no way of being certain that the animal is free from rabies. The bitten person should be given post-exposure prophylaxis (details of the regimen are described below) as soon as possible after the bite. Every year, around 15 million people receive this treatment worldwide, preventing an estimated 327,000 human deaths from rabies.
What do you understand by the term ‘post-exposure prophylaxis’ and where have you met this term in an earlier part of this Module?
Post-exposure prophylaxis (or PEP) means giving preventive therapy very soon after a possible exposure to a life-threatening infectious agent; it is given without waiting for a test to see if the exposure has actually transmitted the infection, because delay could mean that the infection spreads through the person’s body. PEP is given after possible exposure to HIV, for example when a healthcare worker is splashed with blood or is pricked with a needle after injecting a patient with HIV/AIDS.
Post-exposure prophylaxis for HIV is described in Study Session 26 in Part 3 of this Module.
The WHO has published the guidelines in Table 38.1 for PEP following different levels of contact with a suspected rabid animal. Details of the vaccines and rabies immunoglobulin mentioned in the table will be described below.
| Contact category | Action |
|---|---|
| Category I: touching or feeding the animal, licks on intact skin (i.e. no exposure) | None |
| Category II: nibbling of uncovered skin, minor scratches or abrasions without bleeding
| Immediate vaccination and local treatment of the wound |
| Category III: single or multiple bites or scratches that break the skin; contamination of mucus membranes with saliva from licks | Immediate vaccination and administration of rabies immunoglobulin; local treatment of the wound |
Rabies vaccines
Two types of vaccines exist to protect people from rabies after a Category II or III exposure. The older type is made from nerve tissue infected with rabies virus and is given intramuscularly (IM). The newer type of vaccine is made from virus-infected cells grown (cultured) in the laboratory and is safer and more effective. The WHO recommends that the rabies cell-culture vaccine (rabies CCV) should be used in preference to the nerve tissue vaccine wherever possible. Rabies CCV can be given either by intramuscular injection, or intradermally (ID) into the upper arm (Figure 38.4). The intradermal route has been shown to be as safe and effective as the traditional intramuscular route, and is cheaper because it requires less vaccine.

Modern cell-culture vaccines should be given in four or five doses: the dosage for each injection depends on the vaccine type and the route of administration (intramuscular dosages are 0.5 ml or 1.0 ml, whereas the intradermal dosage is only 0.1 ml). If you are referring someone to a health centre for rabies post-exposure prophylaxis, you should tell the patient and their family that it is essential to return at fixed intervals for repeat vaccinations in order to prevent rabies if they have been infected by the bite.
The intramuscular regimen is given at days 0, 3, 7, 14 and 28 after the exposure. The intradermal regimen is given at days 0, 3, 7, 28 and 90 after exposure. There is also a rabies vaccine which is administered at days 0, 7 and 28 days (IM), and rabies duck embryo vaccine, which is administered at day 0, 7 and 21 days (IM or ID). For both these vaccines, a booster dose is given after two to three years.
Rabies immunoglobulin
Specific protection in humans with Category III exposure (see Table 38.1) is provided by injecting a human or equine (horse) immunoglobulin at the site of the bite, as soon as possible after exposure to neutralise the virus. The term ‘immunoglobulin’ refers to a preparation of antibodies made either in humans or in horses who have been vaccinated against rabies. Antibodies from their blood which attack the rabies viruses are harvested and stabilised in an injectable liquid. As much as possible of the dose of rabies immunoglobulin is given into, or as near as possible to, the site of the bite. If there is any remaining in the syringe, it is injected at a different site to elicit active immunity. Human rabies immunoglobulin is given in a single dose of 20 international units (IU) per kilogram (kg) of the person’s body weight. Horse rabies immunoglobulin is cheaper, but less effective and more likely to produce adverse allergic reactions; it is given in a single dose of 40 IU/kg.
38.1.4 Prevention of rabies
Since very few people survive after they develop symptoms of rabies, prevention is the best alternative. The main prevention measures against rabies are aimed at controlling the animals that transmit the virus, educating the community on how to protect themselves from dog bites, and what action to take if they are bitten. Your roles as a Health Extension Practitioner are to contribute to a comprehensive rabies control programme by carrying out the following activities:
- Educate the owners of dogs and the public on the importance of restricting the activity of their dogs.
- People should be educated that they must be careful handling or approaching strange-acting dogs and other canines. Warn parents that their children are particularly at risk.
- If a registration and immunization programme is available in your locality, register and immunize with anti-rabies vaccine any dog that owners want to keep.
- All unwanted dogs should be killed to reduce the population of animals living wild; maintain active searching for rabid dogs and take measures to ensure that they are killed.
- Detain and clinically observe for 10 days any healthy-appearing dog known to have bitten a person, if the owner wants to keep the animal. Unwanted dogs and dogs developing suspicious signs of rabies should be destroyed immediately.
- Give first aid for any dog bite and immediately refer the patient to the nearby health centre for post-exposure prophylaxis.
38.2 Taeniasis (tapeworm infestation)
In this section, you will learn about the definition, mode of transmission, clinical manifestations, and methods of prevention of taeniasis (tapeworm infestation). Taeniasis is a parasitic zoonotic disease caused by the adult stage of large tapeworms that live in the intestines of human hosts. The most common causative agent in Ethiopia is the beef tapeworm, Taenia saginata, which has the cow as its intermediate host. The other tapeworm that can cause taeniasis (Taenia solium) has pigs as its intermediate host, but they are not so common in Ethiopia. Taeniasis due to beef tapeworm is highly prevalent in Ethiopia due to the widespread habit of eating raw beef (kitfo in Amharic, Figure 38.5) and poor sanitary conditions. Defaecation in open fields in grazing lands, disposal of raw human sewage in rivers and its use as a fertiliser, facilitate the spread of taeniasis. The highest cases of taeniasis are found in the towns of Northern and Eastern Ethiopia.

Other tapeworm diseases also exist in certain communities, e.g. people in fishing communities may be exposed to fish tapeworms (Diphyllobothrium species). Hydatid disease is also found in some parts of Ethiopia, caused by Ecchinococcus tapeworms transmitted mainly by dogs, which also infect people, cattle, sheep and horses. However, in this study session, we are focusing exclusively on the most prevalent form of tapeworm infestation in Ethiopia – taeniasis transmitted to humans by cows.
38.2.1 Mode of transmission of taeniasis
Adult beef tapeworms of the species Taenia saginata can grow very large – they can reach a length of five metres within a few months of infecting a person, but some have been recorded at up to 25 metres! The tapeworm attaches to the inside of the intestine by four strong suckers in its tiny head (Figure 38.6a). The long flat body of the tapeworm is formed from between 1,000 to 2,000 sections called proglottids (Figure 38.6b). The proglottids near the end of the tapeworm mature and become capable of surviving for a time after detaching from the main body of the worm. When a mature proglottid breaks away from the adult worm, it can contain up to 100,000 eggs. Approximately six mature proglottids are passed in the person’s stool every day – shedding up to 600,000 eggs into the environment daily!
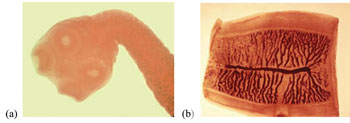
Proglottids of Taenia saginata passed in the faeces of an infected person onto grazing land, or used as fertiliser, are eaten by cows grazing on the same fields. The eggs hatch into larvae inside the cow’s intestine, and burrow out through the intestinal wall into the muscles, where they become trapped inside a wall of tissue that forms around them. This stage of the tapeworm’s lifecycle is called a cysticercus. Cysticercus (singular) is pronounced ‘siss-tee-surr-cuss’. The plural is cysticerci (‘siss-tee-surr-see’).Transmission to new human hosts occurs when the person eats raw or undercooked beef containing a cysticercus. The digestive enzymes in the person’s stomach and intestines digest the wall around the tiny immature tapeworm in the cysticercus, releasing it into the intestine, where it attaches to the intestinal wall by the four suckers shown in Figure 38.6(a). The tapeworm matures in the person’s intestine and begins to release proglottids, continuing the lifecycle.
38.2.2 Clinical manifestations, diagnosis and treatment of taeniasis
Generally, people live with relatively few symptoms even with a large tapeworm inside them. They may experience discomfort around the anus when proglottids are discharged, and diagnosis is made on the basis of seeing the flat white proglottids wriggling in the stools. Mild abdominal pain or discomfort, nausea, change in appetite, weakness, and weight loss can also occur with Taenia saginata infection.
Traditionally, people with tapeworm in Ethiopia self-treat with extracts of kosso – the Amharic name for a slender flowering tree (species name Hagenia abissinica, Figure 38.7), or enkoko – the scarlet fruits of the climbing shrub (Embelia schimperi), both of which have proven taenicidal properties.(Taenicidal refers to any treatment that kills tapeworms; it is pronounced ‘teen-ih-side-ull’). Medical treatment is to give a single dose of praziquantel (one 10 mg tablet for every kilogram of the patient’s body weight), which is highly effective at killing tapeworms. You are not expected to prescribe praziquantel, which is given at a health centre.

Which other communicable disease have you learned about in this Module, which is treated with praziquantel?
Schistosomiasis is also treated with praziquantel, but at a much higher dosage (40 to 60 mg/kg, given in two or three doses during a single day – see Study Session 37, Section 37.1.4).
38.2.3 Prevention and control of taeniasis
The most important role for you as a Health Extension Practitioner in the prevention of taeniasis in your community is to educate community members about the mode of transmission of tapeworms from humans to cows and back to humans.
What health education messages should you give to people in your community to help prevent taeniasis?
You should educate them to:
- avoid open defaecation in the fields, and instead they should use a latrine
- avoid fertilisation of grazing lands by untreated human faeces
- wash hands thoroughly with soap and water after defaecation
- cook meat thoroughly and do not eat raw beef.
Your role in education and inspection to improve food hygiene, sanitation and waste disposal are covered in the Module on Hygiene and Environmental Health.
You also have a role in food hygiene inspection and community sanitation. Refrigeration or salting for long periods, or freezing at -10°C for at least nine days, also kills cysticerci in beef. You should also oversee the proper disposal of human faeces in your kebele.
Summary of Study Session 38
In Study Session 38, you have learned that:
- Rabies is the most fatal of all communicable diseases; it is almost never cured once the patient shows symptoms.
- The virus that causes rabies is transmitted in the bite of infected canines; 99% of cases in Africa are due to dog bites.
- Immediate first aid for the wound and urgent referral for post-exposure prophylaxis with rabies vaccine and rabies immunoglobulin reduces the transmission of rabies after a dog bite and saves thousands of lives.
- Prevention of rabies is mainly through elimination of unwanted dogs, vaccination where this can be afforded, and education of the population about avoiding dog bites and seeking immediate treatment if they are bitten.
- Taeniasis due to beef tapeworm is a common disease in Ethiopia due to the culture of eating raw beef. Infected cows have tapeworms embedded in cysts in their muscles, which can be killed by thorough cooking.
- Infected humans pass up to 600,000 eggs in their faeces every day. Open defaecation in fields and using raw human sewage as fertiliser contaminates grazing land, where cows eat the eggs attached to the grass. This perpetuates the lifecycle.
- Environmental and food hygiene, proper sanitation, and cooking of beef thoroughly are the major prevention measures against taeniasis.
Self-Assessment Questions (SAQs) for Study Session 38
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the following questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 38.1 (tests Learning Outcomes 38.1, 38.2 and 38.3)
Mr. Kebede is bitten on the face by a dog which has shown abnormal behaviour in the last three days. The skin is clearly broken and the wound is bleeding a little bit.
- a.What category of exposure is this event?
- b.If Mr. Kebede comes quickly to your Health Post, which of the following actions should you do for him? In each case, explain why the action is correct or incorrect.
A Give him an antibiotic and send him home
B Suture his wound
C Thoroughly clean his wound with soap and water and send him to the nearby health centre for post-exposure prophylaxis
D Admit him to the Health Post and give him intravenous fluids.
Answer
Mr Kebede has had a Category III exposure – he is bleeding after being bitten by a dog that showed abnormal behaviour.
The correct and incorrect actions are listed below:
A is incorrect. Rabies is caused by a virus. Antibiotics kill bacteria – they have no activity against viruses.
B is incorrect. Suturing the wound seals the viruses inside the body and makes it more difficult to flush it with soap and water, detergent, alcohol or iodine.
C is the correct answer. Thoroughly clean the wound and send Mr Kebede to the nearest health facility for post-exposure prophylaxis.
D is incorrect. Mr Kebede’s wound is only bleeding a little bit. He does not need IV fluids! Admitting him to the Health Post delays referring him for urgent vaccination and rabies immunoglobulin treatment. The delay threatens his life!
SAQ 38.2 (tests Learning Outcomes 38.1, 38.2, 38.3 and 38.4)
Kemal is a three-year-old boy who has had close contact with his pet dog. In the last two days, the dog has showed abnormal behaviour and now it has run away. You examine Kemal carefully all over his body. You find that he has not been bitten and he does not have any scratches or breaks in his skin.
- a.What is Kemal’s category of exposure?
- b.What do you advise Kemal’s family?
Answer
- a.Kemal has had close contact with a dog that has shown some abnormal behaviour, but there are no signs of any bites or scratches on his body and there are no breaks in his skin. Therefore, he is in Category I – no exposure.
- b.Kemal’s family should be advised to search for the dog and approach it with great care. It should be destroyed if its behaviour is abnormal; otherwise it should be kept contained for ten days to see if it develops any signs of rabies and killed if it does. They should ensure that Kemal has no further contact with this (or any other) dog, because children are at high risk of being bitten.
SAQ 38.3 (testing Learning Outcomes 38.1, 38.2, 38.3 and 38.4)
Which of the following statements is false? In each case, explain what is incorrect.
A Most people who show symptoms of rabies will be cured if they are referred for medical treatment.
B Taeniasis causes discomfort in people who have a tapeworm in their intestines, but the disease is almost never fatal.
C Eating well-cooked beef may not protect people from taeniasis.
D Abdominal pain and the appearance of flat white worms in faeces are signs of taeniasis.
E Open defaecation in grazing lands is a risk factor for taeniasis.
Answer
A is false. It is almost inevitable that a person will die if they develop symptoms of rabies, no matter what medical treatment they receive.
B is true. Taeniasis causes discomfort in people who have a tapeworm in their intestines, but the disease is almost never fatal.
C is false. Thorough cooking kills the tapeworm larvae embedded in the meat and prevents their transmission to humans who eat the meat.
D is true. The common symptoms of taeniasis are abdominal pain and the appearance of flat white worms in the stools.
E is true. Open defaecation in grazing lands is a risk factor for taeniasis, because the eggs deposited in human faeces are eaten by cows; the lifecycle of the tapeworm is completed when the larvae become cysticerci in the cows’ muscles and people eat infected raw or undercooked beef.