Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Friday, 19 April 2024, 3:10 AM
Communicable Diseases Module: 41. Integrated Disease Surveillance and Response
Study Session 41 Integrated Disease Surveillance and Response
Introduction
In Study Session 40 we considered what public health surveillance means and the activities it involves. In this study session, we will consider the Integrated Disease Surveillance and Response (IDSR) system. IDSR involves carrying out disease surveillance activities using an integrated approach. An integrated approach means that data on all important diseases will be collected, analysed, interpreted and reported in the same way, by the same people who normally submit routine report forms on health-related data. In this study session, we will also consider the case definitions of priority diseases in Ethiopia, and how priority diseases are reported. Proper understanding of IDSR, the case definitions and reporting methods will enable you to identify, register, analyse and report priority diseases quickly and accurately to the proper authorities. These activities are essential in order to ensure that priority diseases in your community can be prevented and controlled.
Learning Outcomes for Study Session 41
When you have studied this session, you should be able to:
41.1 Define and use correctly all of the key words printed in bold. (SAQs 41.1, 41.2 and 41.3)
41.2 Describe the key features and importance of the Integrated Disease Surveillance and Response (IDSR) system in Ethiopia. (SAQs 41.1 and 41.3)
41.3 Explain how you should use case definitions to identify and report cases of priority diseases and conditions in your community. (SAQs 41.1, 41.2 and 41.3)
41.1 Importance of the Integrated Disease Surveillance and Response (IDSR) system
IDSR brings many surveillance activities together to try and make sure that priority diseases can be controlled and prevented more effectively. The IDSR system requires that all important communicable diseases within a health facility are reported together, using the human and other resources already available within that facility. Collecting, analysing and reporting priority diseases in this way has several advantages:
- First, it is cheap, since the same health personnel and reporting formats are also used for routine reports of health-related data.
- Second, it creates an opportunity to computerise all the available data at the central level.
- Third, it provides training and capacity building opportunities for health personnel to develop new skills.
- Fourth, it encourages community participation to detect and respond to disease epidemics.
Thus, IDSR is a cost-effective surveillance system which addresses the major health problems of Ethiopia. Many other countries in sub-Saharan Africa have adopted a similar IDSR system.
From what has been mentioned above, is IDSR a passive or active surveillance system? Think back to Study Session 40 and give reasons for your answer.
IDSR is a passive surveillance system as the data used are collected during routine health work. Active surveillance, on the other hand, uses data collected after a request from higher authorities for specific information.
41.2 Priority diseases for IDSR in Ethiopia
Priority diseases are diseases that fulfil one or more of the criteria in Box 41.1.
Box 41.1 Priority disease criteria
- They have a high potential for causing epidemics
- They have been targeted for eradication or elimination
- They have significant public health importance (causing many illnesses and deaths)
- They can be effectively controlled and prevented.
Currently, there are 20 reportable priority diseases or conditions in Ethiopia, which are included in the IDSR system (Table 41.1). As the table shows, these 20 priority diseases are further classified into ‘immediately’ or ‘weekly’ reportable diseases. Some of the priority diseases, such as avian influenza, pandemic influenza A, cholera, measles, meningitis and relapsing fever are likely to spread quickly and to affect a large number of people. Therefore, you should always be alert for such diseases in your community, and report immediately to a health centre if you suspect, or are unsure about, a case.
| I. Immediately reportable diseases (report within 30 minutes to higher authority) | Description of the disease | |
|---|---|---|
| 1 | Acute flaccid paralysis (AFP) | Polio is the major cause of AFP (see Study Session 4 of this Module) |
| 2 | Anthrax | An acute bacterial disease, transmitted from animals to humans (zoonosis), manifested by skin lesions and (rarely) respiratory symptoms, e.g. shortness of breath |
| 3 | Avian human influenza | An acute viral disease of the respiratory tract, transmitted from birds to humans, characterised by fever, headache, muscle pain, prostration, runny nose and other symptoms of head cold, sore throat and cough |
| 4 | Cholera | Bacterial disease that causes profuse, watery diarrhoea (see Study Session 34) |
| 5 | Dracunculiasis/ Guinea worm disease | An infection of the deep part of the skin by a worm, manifested by blister formation and discharge of the worm when the affected leg of the patient is immersed into water |
| 6 | Measles | A viral disease manifested by a whole-body rash, cough and sore eyes (see Study Session 4) |
| 7 | Neonatal tetanus | A rapidly fatal bacterial disease of newborns manifested by neck stiffness, convulsions, sensitivity to bright light and inability to feed due to locked jaw (see Study Session 3) |
| 8 | Pandemic influenza A (H1N1) | An acute viral disease of the respiratory tract, transmitted from animals to humans, characterised by fever, headache, muscle pain, prostration, runny nose and other symptoms of head cold, sore throat and cough |
| 9 | Rabies | A viral disease affecting the nervous system, transmitted by the bite of a rabid dog (see Study Session 38) |
| 10 | Severe acute respiratory syndrome (SARS) | A rapidly fatal severe viral respiratory infection associated with gastro-intestinal symptoms such as diarrhoea |
| 11 | Smallpox | A viral disease manifested by a rash (but this disease has been eradicated from the world) |
| 12 | Viral haemorrhagic fever (VHF) | An acute viral disease manifested by fever, muscle pain and bleeding |
| 13 | Yellow fever | An acute viral disease of short duration, transmitted by mosquitoes, manifested by fever, muscle pain and headache |
| II. Weekly reportable diseases | ||
| 14 | Dysentery | A bacterial or amoebic disease manifested by bloody diarrhoea (see Study Sessions 33 and 34) |
| 15 | Malaria | An acute febrile disease with chills, headaches and muscle pain, caused by plasmodium parasites transmitted by mosquitoes (see Study Sessions 5 to 12) |
| 16 | Malnutrition | A condition caused by shortage of protein, or carbohydrate or vitamins or minerals |
| 17 | Meningitis | A bacterial disease manifested by fever and stiffness of the neck (see Study Session 3) |
| 18 | Relapsing fever | A bacterial disease, transmitted by human body lice, manifested by episodes of fever, headache and muscle/joint pain (see Study Session 36) |
| 19 | Typhoid fever | A bacterial disease manifested by fever, headache, joint pain and diarrhoea (see Study Session 33) |
| 20 | Typhus | A bacterial disease, transmitted by human body lice, manifested by sustained high fever, headache and muscle/joint pain (see Study Session 36) |
What is the difference between eradication and elimination? (Think back to Study Session 2 of this Module).
Elimination is reduction to zero (or a target very close to zero) of cases of a particular communicable disease in a particular geographic area. Eradication is the elimination of a communicable disease from the whole world. Polio, guineaworm disease and neonatal tetanus have been targeted for global eradication by the World Health Organization (WHO).
In addition to the reportable diseases and conditions listed in Table 41.1, you should report the health emergencies or emergency conditions listed in Box 41.2. The term cluster refers to a larger-than-expected number of cases with similar symptoms, but without clear evidence (at this time) that they are connected in any way. The increase in cases in a cluster could simply be a coincidence, but it could also be a sign that an epidemic is beginning, i.e. the rise in number is due to transmission of the infectious agents between cases. That is why you should report the conditions in Box 41.2 immediately.
Box 41.2 Health emergencies or conditions to report immediately
- Clusters of respiratory illness (including upper or lower respiratory tract infections and difficulty in breathing)
- Clusters of gastrointestinal illness (including vomiting, diarrhoea, abdominal pain, or any other gastrointestinal distress)
- Influenza-like symptoms and signs, such as fever, cough and runny nose
- Clusters of symptoms or signs indicating the possibility of meningitis (stiff neck, sensitivity to bright light, severe headache, etc.)
- Clusters of rash-like symptoms
- Non-traumatic coma (unconsciousness which is not due to an injury), or sudden death.
41.3 Role of the Health Extension Practitioner in IDSR
As a Health Extension Practitioner working and living in a community, you are likely to know the residents well (Figure 41.1). Your relationship with the community is very important and should help you in your surveillance activities. You can teach the community about priority diseases and conditions in the area so that they are aware of such diseases and report them to you. With good community participation, you can perform surveillance activities (outlined in Box 41.3) in your catchment area much more effectively.

Box 41.3 Role of Health Extension Practitioners in IDSR activities
Your roles are to:
- Identify cases of priority diseases and conditions in the community by using case definitions (see Section 41.4 below)
- Report any cases or possible cases to the nearest Health Centre as soon as possible
- Study suspected cases, identify everyone who is affected, and determine where and when the disease is most common
- Actively search for other cases in the community by doing home visits; inform the community about cases in the area and work with community members to find more cases
- Assist the District Health authorities to treat cases and to control the spread of the disease
- Mobilise and educate the community to prevent the disease from spreading
- Keep your community informed about the cases that have been identified and how they are being managed.
41.4 Case definitions of priority diseases
You learned in Study Session 40 that a case definition is a set of standard criteria used to help you to separate true cases (those with the disease) from suspected cases that do not have the disease. Health workers in hospitals and Health Centres should use standard case definitions for reporting suspected priority diseases, i.e. a definition that has been agreed and should be used by all health professionals at higher levels within the country. Standard case definitions should be applied in the same way to all the persons examined.
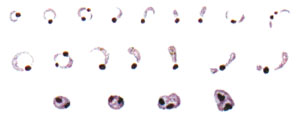
Standard case definitions classify cases as confirmed or suspected. A confirmed case shows all the typical symptoms of a disease and the infectious agent or other cause has been positively identified in a laboratory investigation. For example, in a confirmed case of malaria, the patient shows symptoms typical of malaria, such as fever, headache and joint pain, the rapid diagnostic test (RDT) is positive, and laboratory investigation of a blood smear has confirmed that the person is infected with the Plasmodium parasites that cause malaria (Figure 41.2). On the other hand, a suspected case of malaria means that the person shows symptoms of malaria, but a laboratory investigation either has not been conducted yet, or has failed to find evidence of the parasite that causes malaria.
A community case definition is a simplified version of the standard case definition, adapted to suit the needs and resources of Health Extension Practitioners/Workers, community health volunteers, community members, traditional healers and birth attendants. It is useful to make a poster showing these definitions for the Health Post wall in the local language. Table 41.3 summarises community case definitions for some of the priority diseases in Ethiopia.
| Priority disease | Simplified community case definition |
|---|---|
| Acute watery diarrhoea in children aged under 5 years | Any child having loose stools within the last 24 hours, or showing danger signs of loss of fluid from the body (dehydration) |
| Cholera | Any person aged 5 years or older with lots of acute watery diarrhoea |
| Diarrhoea with blood and mucus | Any person with diarrhoea and visible blood and mucus in the stools |
| Epidemic typhus | Any person with sudden onset of headache and fever with chills, and general muscle pains, with or without spots (rash) |
| Guineaworm | Any person with a history of emergence of worms from the leg |
| Leprosy | Any person with loss of sensation and/or weakness in the muscles of the hands, feet or face; or loss of part of the hands or feet |
| Malaria | Any person with fever, or fever with headache, back pain, chills, sweats, muscle pain, nausea and vomiting |
| Measles | Any person with fever and spots (rash) |
| Meningitis | Any person with fever and neck stiffness |
| Neonatal tetanus | Any newborn who is normal at birth, but after two days becomes unable to suck or feed |
| Polio | Any acute paralytic disease |
| Plague | Any person with painful swelling(s) under the arms or in the groin area; in an area where plague is endemic, any person with a cough, chest pain and fever |
| Pneumonia | Any child less than 5 years of age with a cough and fast breathing, or difficulty in breathing |
| Relapsing fever | Any person with a fever that returns following a previous fever |
| Tuberculosis | Any person with a cough lasting three or more weeks |
| Typhoid fever | Any person with fever, constipation or diarrhoea, confusion (delirium) and with the body in a passively prone position (prostration) |
| Viral haemorrhagic fever | Any person who has an unexplained illness with fever and bleeding, or who died after an unexplained severe illness with fever and bleeding |
| Yellow fever | Any person with fever and yellowing in the white part of the eyes, or yellowing of the skin |
As a Health Extension Practitioner, you need to teach the community about these community case definitions of common diseases (Figure 41.3). The community can recognise and report common diseases to you if they understand these case definitions. The advantage of using community case definitions (instead of standard case definitions) is not only that they are simpler to understand. They are also ‘broader’ than standard case definitions, which means that more suspected cases will be identified using the community case definition, and fewer cases will be missed.

41.5 Reporting of priority diseases
Complete and reliable reporting of surveillance data throughout the country is vitally important, so that programme managers, surveillance officers and other healthcare staff can use the information for action. The 20 priority diseases and conditions of concern shown in Table 41.1 are classified into two categories (immediately reportable and weekly reportable), depending on their epidemic potential and whether (like polio and neonatal tetanus) they have been targeted for elimination or eradication.
41.5.1 Immediately reportable diseases
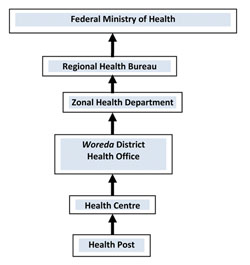
Of the 20 priority diseases in Table 41.1, 13 must be reported immediately to the next reporting level. For these immediately reportable diseases, a single suspected case could signal the outbreak of an epidemic, so it is important to report any cases or suspected cases to the next level of the reporting hierarchy within 30 minutes. This means you should report cases to the nearest Health Centre within 30 minutes, the Health Centre reports to the District Health Office within 30 minutes, and so on up to the highest national level (see Figure 41.4).
When you encounter a case of an immediately reportable disease, first report the information verbally or by telephone, or by sending a text using the SMS short message service. An official written report using the modified case-based reporting format (see Appendix 41.1) should follow immediately after the verbal report. You should remember to record the affected person’s address, age, sex, vaccination status and symptoms. You should also suggest a possible diagnosis – that is, which of the 13 immediately reportable diseases you suspect. The date of referral and your signature should also be on the reporting form. After completing the form, you should immediately send the patient to the Health Centre and check by telephone to confirm the arrival of the patient at the Health Centre.
41.5.2 Weekly reportable diseases
Currently, seven diseases and conditions are identified to be reported weekly to the next reporting level (see Table 41.1). Reports should include the total number of cases and any deaths seen during the week (Monday to Sunday). Reports should be sent to the Health Centre every Monday, using the weekly reporting format shown in Appendix 41.2. In this format, you are expected to record the name of the disease, as well as the age and sex of the patient, and the place where the case was diagnosed (Health Post or community). For suspected cases of malaria, the laboratory result based on the rapid diagnostic test (RDT) should also be recorded.
Before you use the weekly reporting format, what types of analysis should you do if there is more than one case of a priority disease? (Think back to Study Session 40.)
You should organise and report the data according to the age and sex of the cases to see if any patterns are evident. As you should remember from Study Session 40, data should be analysed in this way before reporting.
In the final study session in this Module, we describe in more detail the actions you should take to investigate and manage an epidemic of a communicable disease in your community.
Summary of Study Session 41
In Study Session 41, you have learned that:
- In the Integrated Disease Surveillance and Response (IDSR) system, important communicable diseases within a community are integrated and reported to higher levels in the health system, using the usual human and other resources of the health facility.
- The advantages of the IDSR system are that it is cheap and provides a training opportunity for health workers. It also makes data about all priority diseases available at a central level.
- Priority diseases have been identified in each country to be included in the IDSR system. They are major causes of illness and death in the population, they can easily cause epidemics, they can be controlled and prevented, and they can be identified using standard or community case definitions.
- There are 20 priority diseases of public health importance included in the IDSR in Ethiopia. They are classified as immediately or weekly reportable diseases.
- Immediately reportable diseases should be reported to a higher level within 30 minutes, using verbal methods (radio, phone, text), followed by written reports using the official immediate reporting format. Weekly reports are sent every Monday using the official weekly reporting format.
- As a Health Extension Practitioner, you must keep a close watch for possible cases of priority diseases in your catchment area, and quickly report any suspected or unusual cases or clusters of symptoms to the nearby Health Centre for investigation and management.
- Standard case definitions of priority diseases are applied at Health Centres and hospitals. Simplified community case definitions have been developed for use by Health Extension Practitioners/Workers, community health volunteers, traditional healers and birth attendants, and community members. It is part of your role to educate your community on the community case definitions of priority diseases, so that they can be detected and reported as soon as possible.
Self-Assessment Questions (SAQs) for Study Session 41
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 41.1 (tests Learning Outcomes 41.1, 41.2 and 41.3)
Ayele is a 30-year-old farmer who comes to your Health Post with profuse and frequent watery diarrhoea. He has lost a lot of fluid and is very weak, so he finds it difficult to walk. His family informs you that there are several similar cases among adults in their village. What should you do?
Answer
Profuse and frequent watery diarrhoea in adults may be an indication of the occurrence of a cholera epidemic. You should report the situation within 30 minutes to the Health Centre. You should verify the existence of similar cases in the community and educate the community on environmental sanitation, such as using a latrine, ensuring a safe water supply for drinking and cooking, and using personal hygiene measures such as hand washing with soap to prevent the transmission of diarrhoeal diseases. Ayele should be started on oral rehydration solution (ORS, see Study Sessions 32 and 33) and transferred to the Health Centre urgently for specialist treatment.
SAQ 41.2 (tests Learning Outcomes 41.1 and 41.3)
Which one of the following health problems is not an immediately reportable disease?
- a.Polio
- b.Avian influenza
- c.Rabies
- d.Malnutrition
- e.Neonatal tetanus
Answer
d. is the correct answer. Malnutrition is a weekly reportable health problem, not an immediately reportable priority disease. Polio, avian influenza, rabies and neonatal tetanus are all immediately reportable priority diseases.
SAQ 41.3 (tests Learning Outcomes 41.1, 41.2 and 41.3)
Which of the following statements is false? In each case, explain why it is incorrect.
A IDSR is a type of active surveillance where data on priority diseases is actively collected in the community.
B IDSR is cost-effective and helpful for integrating data on all reportable diseases at central level.
C To identify priority diseases in the community, community health workers and member of the community should use standard case definitions.
D Diseases targeted for eradication should be reported weekly to the higher level.
E One case of a disease cannot be an indication of an epidemic.
Answer
A is false. IDSR is a type of passive surveillance where data for all important diseases are gathered routinely by health institutions.
B is true. IDSR is cost-effective, since the same human resources and formats are used to report all diseases in the community. It also creates an opportunity to integrate data on all important diseases at central level.
C is false. To identify cases in the community, community workers and Health Extension Practitioners should use simplified community case definitions. Standard case definitions are for use in Health Centres and Hospitals.
D is false. Diseases targeted for eradication, such as neonatal tetanus, should be reported immediately.
E is false. A single case of a disease can indicate an epidemic. For example, a single case of cholera or of acute flaccid paralysis may signal an epidemic of cholera or polio.