Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Saturday, 22 November 2025, 1:47 PM
Communicable Diseases Module: 42. Epidemic Investigation and Management
Study Session 42 Epidemic Investigation and Management
Introduction
In Study Sessions 40 and 41 you learned that one use of surveillance is to find out if there is an unusual increase in cases of any communicable diseases in your community, which could signal the start of an outbreak or epidemic. In this final study session, you will learn more about the different kinds of epidemics and how to investigate and manage them. A better understanding of epidemics will help you to detect an outbreak or epidemic of a communicable disease and report it immediately to the Health Centre and/or District Health Office. You are also expected to help the District Health Team in the control of any epidemics in your catchment area.
Learning Outcomes for Study Session 42
When you have studied this session, you should be able to:
42.1 Define and use correctly all of the key words printed in bold. (SAQs 42.1, 42.3 and 42.4)
42.2 Describe the different types of epidemics. (SAQs 42.1 and 42.3)
42.3 Describe the purpose of epidemic investigation. (SAQ 42.4)
42.4 Explain in outline the basic principles of epidemic management. (SAQs 42.2 and 42.4)
42.1 What is an outbreak and an epidemic?
If there is an increase in cases of a disease compared with the expected number, but it lasts for only a short time, or it occurs only in a limited area (e.g. in a few nearby households), the rise may be referred to as an outbreak. As you will remember from Study Session 1 of this Module, an epidemic is also an excess of cases compared with the number expected. However, an epidemic is more general than an outbreak, the increase in the number of cases continues far longer (possibly months or even years), and the cases are distributed across a wider area.
For example, it may be that during January to March there are normally fewer than 10 cases of tuberculosis (TB) in your kebele. If you found 30 cases of tuberculosis in a particular January, followed by 39 cases in February and 45 cases in March, then you would strongly suspect that there was an epidemic of TB in your community. You would then need to find out why TB had suddenly increased.
Which disease often causes epidemics during the months of June, September and October in Ethiopia? Why are these the months when these epidemics most often occur?
Malaria is the major vector-borne disease that causes epidemics in the months of June, September and October in Ethiopia. This is when the conditions are humid and warm enough and there are plentiful water collections for the vector mosquitoes to breed in. You learned about malaria in Study Sessions 5–12 of this Module.
42.2 Types of epidemics
Epidemics are classified into different types according to the source of infection and modes of transmission.
From Study Session 1 of this Module, briefly describe the two main modes of transmission of communicable diseases.
They are: (1) direct modes of transmission, such as from mother to child, or from faecally contaminated hands into the mouth; and (2) indirect modes of transmission, such as through vectors, contaminated air, water, food or objects such as cooking bowls and utensils.
Based on criteria such as this, epidemics are classified into three types:
- common source outbreaks
- propagated or progressive epidemics
- mixed epidemics.
We will look at each of them in turn.
42.2.1 Common source outbreaks
Common source outbreaks occur when the rise in cases of an infection occurs after a group of people all came into contact with the same unsafe source of infection (the common source), such as contaminated food or water. For example, imagine a wedding where food was prepared in the morning to serve to wedding guests in the evening. If the prepared food was left outside on a hot day under the sun until evening, bacteria might multiply in the food. If this food was served to the guests in the evening without reheating it thoroughly, many of the guests might fall ill from eating the contaminated food (Figure 42.1). This kind of epidemic is called a common source outbreak because the affected guests all ate the same contaminated food at the wedding.

After the food had been prepared in the morning, explain what should have been done to make it safe to serve to the wedding guests in the evening.
Bacteria like moisture and warmth, and they multiply quickly in food left in hot sun for many hours. After the food had been prepared, it should have been kept covered in a refrigerator (Figure 42.2) or in a cool place inside the house, away from direct sun. The food should also have been reheated thoroughly before being served to the guests.
 Figure 42.2 Refrigerating food reduces the risk of a common source outbreak of a foodborne infection.
Figure 42.2 Refrigerating food reduces the risk of a common source outbreak of a foodborne infection.
A point source outbreak is a common source outbreak where the exposure period (e.g. the time at which the contaminated food was eaten) is short. This means that all cases who fall ill after eating the food (the common source) also have the same incubation period, i.e. the period between infection (eating the contaminated food) and the appearance of the first symptoms.
42.2.2 Propagated or progressive epidemics
Propagated or progressive epidemics occur when the infection spreads from person to person. The infectious agents causing the disease pass from one host to another, either directly from person to person (e.g. via hand shaking or kissing), or indirectly via vectors (e.g. mosquitoes in the case of malaria), or in water, food or another medium. The distribution of malaria cases is a good example of a propagated epidemic, because increased numbers of malaria cases occur again and again at different times. Propagated epidemics last longer than the common source outbreaks described above. This is because malaria will continue to spread in the community, as long as mosquitoes are present in the environment and there are people who carry the parasite.
Can you think of any epidemic-prone diseases that spread quickly in overcrowded conditions where there is poor sanitation and personal hygiene?
You may have thought of typhoid fever, cholera, shigellosis (bacterial dysentery), louse-borne relapsing fever and typhus. (Think back to Study Sessions 33 and 36.)
42.2.3 Mixed epidemics
Mixed epidemics show characteristics of both common source and propagated epidemics. So a mixed epidemic can start with a common source and be followed by a propagated spread. Mixed epidemics are often caused by foodborne infectious agents.
Typhoid fever can easily spread and become a propagated epidemic. Can you remember from Study Session 33 how the typhoid bacteria are transmitted from person to person?
Typhoid bacteria are transmitted from infected people to new susceptible hosts via contaminated food or water.
The organism that causes typhoid (Salmonella typhi) can survive in sewage for 14 days and in water for up to seven days. Water polluted by faecal matter is therefore the main source of infection for typhoid. If the whole community drinks water from the same water source (Figure 42.3), which has been contaminated with Salmonella typhi, there will be a common source outbreak of typhoid fever. The epidemic may continue to spread through faecal matter passing from person to person, if the people in the affected community do not improve their standards of personal hygiene, or if the water is not treated and made safe to drink. This type of spread of typhoid is called a propagated epidemic of typhoid.

42.3 Epidemic investigation
Epidemic investigation is a set of procedures used to identify the cause, i.e. the infectious agent, responsible for the disease. It is also used to identify the people affected, the circumstances and mode of spread of the disease, and other relevant factors involved in propagating the epidemic. This is especially important if the epidemic has unusual features, if it presents a significant threat to public health, and it is not self-limiting (i.e. it does not end spontaneously without professional intervention).
Epidemic investigation is a challenging task for health workers. The main purpose of epidemic investigation is to control the spread of the disease before it causes more deaths and illness. As a Health Extension Practitioner, the first action you should take is to confirm the existence of an epidemic. To do this, you need to know the average number of cases of that disease during this specific month in your community in previous years, so you can compare that number with the current number of cases. Is there an excess number of cases or deaths from this disease compared to the usual occurrence? If there really are excess cases, you should report your findings to the District Health Office immediately. The reporting formats were given in Study Session 41.
The next steps (Box 42.1) will be taken by the District Epidemic Management Team, which is composed of many different health professionals such as doctors, nurses, environmental experts and others. These steps include confirming the cause (the infectious agent involved), the number of people affected (the cases) and the modes of transmission of the infection from cases to new susceptible hosts.
Box 42.1 Steps in an epidemic investigation
- Establish the existence of an outbreak
- Verify the diagnosis or causes
- Define and identify cases:
- a.Use a standard case definition (see Study Session 41)
- b.Identify and count cases
- Perform descriptive epidemiology, i.e. collect data on the age, sex, etc. of the cases and analyse the data to see if useful patterns emerge
- Develop hypotheses to explain the occurrence of the epidemic:
- a.Evaluate the hypotheses
- b.Reconsider/refine the hypotheses
- Carry out additional studies to confirm or reject the explanations for the epidemic:
- a.Additional epidemiological studies
- b.Other types of studies, e.g. laboratory tests, environmental investigations
- Implement control and prevention measures
- Communicate findings to higher levels in the health system, community leaders and other local stakeholders.
42.4 Management of epidemics
Epidemic management activities include taking appropriate control measures, such as treating those who are ill to reduce the reservoir of infection, and providing health education to limit the transmission of the disease to others. Health professionals at higher levels will require your help in putting into taking any measures needed to control the spread of the disease, such as giving drugs to people in the community and providing health education.
As mentioned above, you may be involved in the management of an epidemic once it is confirmed by the health authorities. The type of control measures you need to implement depend on the type of infectious agent, how the disease is transmitted, and any other factors contributing to the disease. Generally, your control measures should target the infectious agent, the source of any infection, and the treatment of those who became ill. Remember, the source of infection could be humans or animals, or non-living things in the environment.
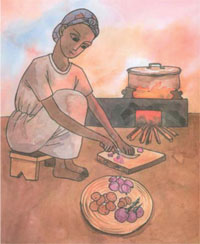
If you do not implement the correct control measures, the epidemic may continue to spread in your area. For example, if contaminated food is the source of an outbreak in your community, you will need to control the outbreak by teaching the community about food hygiene (Figure 42.4), so they are not exposed to contaminated food. If it is caused by contaminated water, you should educate them not to drink the water until it is treated with chlorine. If mosquito breeding sites are the source of a malaria epidemic, you will need to teach the community to clear the breeding sites for mosquitoes.
This short discussion of epidemic investigation and management brings the Communicable Diseases Module to a close. We hope that after studying the 42 study sessions and completing your practical training attachments, you will feel confident to identify, treat, refer, prevent and control communicable diseases effectively in your community, and report cases accurately and at the proper time.
Summary of Study Session 42
In Study Session 42, you have learned that:
- An epidemic is the occurrence of more cases of a disease than would be expected in the population at that period of time. An outbreak is an increase in cases for a short time in a limited area.
- A common source outbreak is an epidemic which arises from a single source of infection, and where most people fall ill after the same incubation period.
- A propagated epidemic occurs when the infection spreads from one person to another, e.g. through the air, via a vector, via contaminated food or water, or during unprotected sexual intercourse.
- A mixed epidemic can start with a common source and be followed by a propagated spread.
- An epidemic investigation is conducted to rapidly identify the cause of an outbreak or epidemic and to take effective actions to contain and prevent the spread of the disease.
- Epidemic investigation and management involves team work. Your role as a Health Extension Practitioner is to report the occurrence of an epidemic, to mobilise and educate the community, and to assist the District Health authorities in carrying out control and prevention measures as required.
Self-Assessment Questions (SAQs) for Study Session 42
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 42.1 (tests Learning Outcomes 42.1 and 42.2)
Explain the difference between common source and propagated epidemics, and give one example of each.
Answer
In a common source epidemic, there is a single source of infection and most people develop the disease after the same incubation period. Good examples are foodborne diarrhoeal diseases. In propagated epidemics, the disease is transmitted from person to person via, for example, a vector, respiratory droplets coughed or sneezed into the air, sexual contact, or some other direct or indirect method. Good examples are a malaria epidemic, or louse-borne relapsing fever or typhus.
SAQ 42.2 (tests Learning Outcome 42.4)
If an outbreak is spread via a contaminated community water supply in your catchment area, what action should you take as a Health Extension Practitioner?
Answer
Educate the community to boil the water or add chemicals such as chlorine before drinking the water.
SAQ 42.3 (tests Learning Outcomes 42.1 and 42.2)
What differences would you expect to find if you could measure a. the incubation period in an epidemic of HIV/AIDS in a village and b. the incubation period in an epidemic caused by eating contaminated food at a birthday celebration?
Answer
- a.HIV/AIDS occurs in propagated epidemics. Therefore, in an HIV/AIDS epidemic, the people affected will not become sick after the same incubation period, because they were infected at different times and from different sources.
- b.By contrast, in a common source outbreak of a foodborne infection, most people will become sick after the same, single incubation period because they acquired the infection from the same food at the birthday celebration.
SAQS 42.4 (tests Learning Outcomes 42.1, 42.3 and 42.4)
Suppose at your Health Post you have seen 11 cases in three days of people who have acute watery diarrhoea, and recorded them as in Table 42.1. One patient (case 7) died soon after arrival at the Health Post.
- a.Describe the distribution of the cases by the sex of the patients.
- b.What diagnosis do you suspect from reviewing these 11 cases? Explain your answer.
- c.What action should you take?
| Case | Age in years | Occupation | Sex | Address/kebele | Date illness began |
|---|---|---|---|---|---|
| 1 | 25 | Teacher | Male | 01 | Jan 3, 2002 |
| 2 | 29 | Housewife | Female | 01 | Jan 4, 2002 |
| 3 | 45 | Farmer | Male | 01 | Jan 5, 2002 |
| 4 | 35 | Farmer | Male | 01 | Jan 4, 2002 |
| 5 | 38 | Teacher | Female | 01 | Jan 5, 2002 |
| 6 | 25 | Day worker | Female | 01 | Jan 4, 2002 |
| 7 | 10 | Child | Male | 01 | Jan 4, 2002 |
| 8 | 29 | Housewife | Female | 01 | Jan 4, 2002 |
| 9 | 22 | Housewife | Female | 01 | Jan 3, 2002 |
| 10 | 39 | Farmer | Male | 01 | Jan 3, 2002 |
| 11 | 21 | Farmer | Male | 01 | Jan 5, 2002 |
Answer
- a.There are 6 males and 5 females with acute watery diarrhoea.
- b.The number of cases (11) is high in three days and may indicate the occurrence of a cholera epidemic. In particular, the death of a person over 5 years old from diarrhoea is an indicator of cholera (think back to Study Session 33).
- c.Immediately report these cases and your suspected diagnosis of cholera to the District Health Office for further investigation and management. Go into the community and see if you can find other similar cases. Educate community members on how they can prevent the spread of the infection.