Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Thursday, 5 February 2026, 5:53 AM
Family Planning Module: 5. Oral Contraceptive Methods
Study Session 5 Oral Contraceptive Methods
Introduction
Oral contraceptives are pills that a woman takes by mouth to prevent the occurrence of pregnancy. The pills contain hormones which are similar to the natural female reproductive hormones, oestrogen and progesterone. Oral contraceptives are commonly known as ‘the pill’, ‘combined pill’, ‘birth control’ or ‘mini-pill’. The pill works mainly by changing the body’s hormone balance so that the woman does not ovulate. It is more effective if taken correctly and consistently. Most women can take the pill without developing any side-effects. However, a small number of women develop mild side-effects, which usually go away within days or weeks of starting the pill.
In this study session, you will learn about the concept, types and mechanism of action of oral contraceptive pills, their effectiveness, advantages and disadvantages, common side-effects, and the management of the side-effects of this method.
Learning Outcomes for Study Session 5
When you have studied this session, you should be able to:
5.1 Define and use correctly all of the key words printed in bold. (SAQ 5.4)
5.2 Discuss common myths and rumours about oral contraceptives. (SAQ 5.1)
5.3 Describe the types and mechanism of action of oral contraceptives.(SAQ 5.2)
5.4 Discuss the effectiveness and use of oral contraceptives. (SAQs 5.3, 5.4 and 5.5)
5.5 Explain the advantages and disadvantages of oral contraceptives. (SAQ 5.6)
5.6 Explain common side-effects and their management for oral contraceptives. (SAQ 5.7)
5.1 Misconceptions and facts about oral contraceptives
There are many myths, rumours and misconceptions associated with taking oral contraceptives. You may be aware of some yourself. The most common ones are listed in Box 5.1. Do your best to ensure that your clients know the truth about these myths.
Box 5.1 Myths and facts about contraceptive pills
| Myth: | Women who stop taking the pill may not be able to get pregnant. They become infertile. | |
| √ | Fact: | Most women who use a method of contraception, including the pill, can later get pregnant if they wish. The pill will not cause women to be infertile. |
| Myth: | The pill causes cancer. | |
| √ | Fact: | The pill does not cause cancer. In fact, the pill actually reduces the risk of getting certain cancers, such as endometrial and ovarian cancers. |
| Myth: | Oral pills build up in a woman’s body. | |
| √ | Fact: | Oral pills do not build up in a woman’s body. |
| Myth | Women need to rest from taking oral contraceptives on sex-free days. | |
| √ | Fact: | Women do not need a rest from oral contraceptives. They have to take them every day, whether or not they have had sex that day. |
| Myth: | Oral contraceptives cause birth defects or multiple births. | |
| √ | Fact: | Oral contraceptives do not cause birth defects or multiple births |
| Myth: | Oral contraceptives change women’s sexual behaviour. | |
| √ | Fact: | Oral contraceptives do not change women’s sexual behaviour. |
| Myth: | Oral contraceptives accumulate in a woman’s stomach. | |
| √ | Fact: | Oral contraceptives do not collect in the stomach. Instead, the pill dissolves each day. |
5.2 Oral contraceptives and how they work
Based on their hormone content, oral contraceptives are divided into two types:
- combined oral contraceptives (COCs), which contain the hormones oestrogen and progesterone
- oral contraceptives with a single hormone, known as progestin-only oral contraceptives.
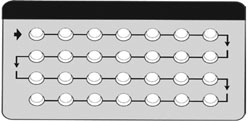
Combined oral contraceptives (COCs, OCs, and often just called the pill) are the most popular type of birth control. The term combined is used because they contain both oestrogen and progesterone hormones. There are many different brands, and they come in packs of 21 or 28 pills. Two brands, microgynon and Leo-femenal, both in packs of 28 pills, are the most popular ones in Ethiopia. One pill is taken every day. The first 21 pills have a combination of synthetic oestrogen and progesterone hormones. The last seven pills of a 28-day pack have no hormones and are called spacer pills. They are usually different in colour, and some brands contain iron. The iron in the pill can be taken as a supplement to avoid iron deficiency (Figure 5.1).

Progesterone-only (or progestin-only) oral birth control pills (or mini-pills) come in packs of 28 pills and women take one every day. They contain a synthetic form of the progesterone hormone called progestin, and no oestrogen (Figure 5.2).
![]() Remember oral contraceptives do not protect against STIs or HIV/AIDS.
Remember oral contraceptives do not protect against STIs or HIV/AIDS.
Neither combined, nor progesterone-only oral contraceptives, protect against sexually transmitted infections (STIs), including HIV/AIDS. If your client has or might get an STI, they should be given condoms to use regularly.
The pill works mainly by changing the body’s hormonal balance so that the woman does not ovulate. That is, she does not release an egg (or ovum) each month from one of her ovaries. In addition, the pill causes the mucus made by the cervix to thicken and form a ‘mucus plug’ in the cervix which makes it difficult for sperm to get through to the uterus (womb) to fertilise an egg. The pill also makes the lining of the uterus thinner, which makes it unlikely that a fertilised egg will be able to attach to the uterus.
5.3 Effectiveness of oral contraceptive methods
5.3.1 Combined oral contraceptive (COC)
Effectiveness depends on the user. It is 99.9% effective if used correctly and consistently. This means that less than one woman in 1,000 using combined oral contraceptives correctly and consistently will become pregnant in the first year of use. Correct use means not missing any pills, and taking extra contraceptive precautions if that happens. Risk of pregnancy is greatest when a woman starts a new pill pack three or more days late, or misses three or more pills near the beginning or end of a pill pack.
5.3.2 Progesterone-only oral contraceptive or mini-pill
The mini-pill is more effective for lactating mothers. It is 99% effective if used consistently and correctly by breastfeeding mothers, because breastfeeding itself provides protection against pregnancy. For all women, it is very effective when used correctly and consistently, with an incidence of less than 0.5 pregnancies per 100 women in the first year of use.
In this context, what does correct use mean?
It means taking the pill every day, at about the same time, not missing any pills, and taking extra contraceptive precautions when necessary.
Mistakes in pill taking lead to pregnancy more often with the mini-pill than with combined oral contraceptives.
5.4 Use of oral contraceptives
What makes using oral contraceptives attractive to many women?
Pills are a particularly attractive contraceptive option for women who like to be in control of their method, and can take a daily dose in a consistent way.
Oral contraceptives are particularly popular with young, sexually active, nulliparous women (those who have never given birth), and those who are not at risk from STIs. Lactating and non-lactating mothers can also use oral contraceptives. They can be used in the post-abortion and post-partum period, and they are preferred by women who desire a fast return to fertility when stopping birth control. Finally, they are known to reduce pre-menstrual pain.
5.4.1 How to use COCs
As part of your role as a health practitioner you need to know how to help clients use their contraceptive method(s) of choice. In Box 5.2, you will find a summary of the procedure for using COCs.
Box 5.2 Procedure for using COCs
Give your female client at least one packet of the same pills that she will use, even if she will be getting her pills elsewhere later.
Show her:
- which kind of pill packet you are giving her (21 pills or 28 pills). If the pack has 28 pills, point out that the last seven ‘remainder’ pills are a different colour and do not contain hormones.
- how to follow the direction of the arrows on the packet to take the rest of the pills, one each day (including the remainder pills).
- Give her instructions on starting the first packet, starting the next packet, and what to do if she misses a pill.
- Ask her to repeat the most important instructions, and show you how she will take her pills, using the pill packet.
- Ask her if she has any questions, fears or concerns, and answer her concerns clearly and respectfully.
Starting COCs
There are several ways to begin taking the pill. One common way is to start on the first day of menstruation (or period), or the first day after an abortion.
Continuing COCs
The client has to take her pill on a daily basis, one pill every day until she finishes an entire pack. In order to remember this, she needs to link taking the pill with a regular activity that she does at the same time every day, like eating a meal or brushing her teeth.
Women who cannot take the pill
Some women may not be able to take the pill because of the risk of serious health problems. If they display any of the following symptoms, which could be due to a blood clot, they must see a health officer or doctor straight away:
- Severe headache
- Bad pains in the chest
- Leg swelling
- Breathing difficulty
- Coughing up blood
- Sudden problems with sight or speech
- Weakness or numbness in an arm or leg
- Collapse.
Women who are under 35 years and have migraines, gall bladder disease, hypertension, diabetes, epilepsy, sickle cell disease, and/or have had elective surgery, have a history of blood clots, or liver or heart disease, may not be able to take the pill.
Women who are over 35 years and have a history of heart attacks, or strokes, blood clots, unexplained vaginal bleeding, known or suspected cancer, known or suspected pregnancy or liver disease, should not take the pill at all.
Instructions for missed pills
You will need to instruct women on how to continue taking pills after they have missed one or more pills from the pack. See Box 5.3 for some useful rules for missed pills.
Box 5.3 Rules for missed pills
ALWAYS:
- Take a pill as soon as you remember.
- Take the next pill at the usual time. This may mean taking two pills on the same day or even at the same time.
- Continue taking active pills (see Figure 5.1) as usual, one each day.
You should also advise your clients to follow the steps in Table 5.1 when they have missed a pill or started the pack late.
| When pills are missed | How pills are missed | Follow the three rules in Box 5.3 and instructions below |
|---|---|---|
| In the first seven days | Started the pack two or more days late, OR Missed any two to four pills | Avoid sex, or use additional contraception for the next seven days. |
| Days 8–14 | Missed any two to four pills | Follow the three ‘Always’ rules in Box 5.3. |
| Days 15–21 | Missed any two to four pills | Go straight to the next pack. Throw away inactive pills from 28-day pack (days 22–28); don’t wait seven days before starting a 21-pill pack. |
| In the first three weeks (days 1–21) | Missed five or more days in a row | Avoid sex, or use additional contraception for the next seven days. Go straight to the next pack. Throw away inactive pills from a 28-day pack (days 22‒28); don’t wait seven days before starting a 21-pill pack. |
5.4.2 How to use the mini-pill
Starting mini-pills
With mini-pills there are hormones in each pill, and there are no spacer pills. It is important for women to take a pill every day, preferably at the same time each day. Forgetting a mini-pill, or taking it late, increases the chance of pregnancy more than missing a COC pill.
The client can improve the effectiveness of mini-pills by adding a back-up method, for example condoms or spermicides (chemicals that kill sperm cells). This is most important during the first three months, and for days 8–18 of your menstrual cycle after that. The client should take the first pill on the first day of her period. She also needs to take one pill daily, at the same time of day, even during her period.
Continuing mini-pills
As soon as she finishes one pack the woman has to begin the next one, and start her next pack even if she is still bleeding, or has not started her period. She should continue taking one pill every day. If she has problems with the mini-pill, she needs to visit the health centre or hospital. She should not stop taking the mini-pill unless she wants to get pregnant or use another method of birth control.
Women who cannot use mini-pills
Every woman is different, and mini-pills are not recommended for all women. Due to the risk of serious health problems, women with the following conditions should not use mini-pills:
- Unexplained vaginal bleeding
- Known or suspected pregnancy
- Breast cancer.
Mini-pills are also not recommended for women who are concerned about weight gain, have liver disease, gall bladder disease, heart disease, diabetes, or a history of depression.
5.5 Advantages and disadvantages of oral contraceptive methods
Here you will learn about the common advantages and disadvantages of oral contraceptives (OCs). By the end of this study session, you should be able to explain to your family planning clients the advantages and disadvantages of COCs and mini-pills.
5.5.1 Advantages of COCs
Most women can safely use COC pills throughout their reproductive years.
Combined oral contraceptives have a number of advantages. The main one is when taken consistently and correctly, COCs are very effective contraceptives that give women control over their own fertility. Most women can safely use COC pills throughout their reproductive years, as long as they want to prevent pregnancy. Thus, they can be used at any age from adolescence to menopause. More importantly, women’s fertility returns soon after stopping taking the pills. COCs can also prevent or decrease iron deficiency anaemia because the pills decrease menstrual flow significantly in women with a normal uterus, meaning they are less likely to develop iron deficiency anaemia.
COCs decrease menstrual cramps and pain. Some women consider this to be their most desirable effect. They also help prevent ectopic pregnancies, endometrial cancer, ovarian cancer, ovarian cysts, pelvic inflammatory disease and benign breast disease. Furthermore, combined oral contraceptives can increase a woman’s sexual enjoyment because she does not have to worry about getting pregnant. In addition, they can be used as an emergency contraceptive after unprotected sex (refer to Study Session 10 on Emergency Contraception). See Box 5.4 for a summary of the advantages of combined oral contraceptives.
Box 5.4 Key points about oral contraceptives
- COCs are very effective contraceptives, giving women control over their own fertility when taken consistently and correctly.
- Fertility returns soon after stopping COC pills, which makes them an excellent option for women who want to become pregnant in the near future.
- Combined oral contraceptive pills decrease menstrual flow significantly in women with a normal uterus. Therefore, pill users are less likely to develop iron deficiency anaemia. Pills also decrease menstrual cramps and pain.
5.5.2 Advantages of mini-pills
The mini-pill can be used by nursing mothers, as it does not affect breastmilk.
The major advantage of the mini-pill is that it can be used by nursing mothers six weeks after giving birth, and does not affect the quality and quantity of breastmilk. In contrast, COCs can slightly reduce milk production. As the mini-pill is free of oestrogen it avoids oestrogen-related side effects, such as heart attacks or strokes. It is also easier to understand how to take the mini-pill since women take one pill every day without a break. The mini-pill may also help prevent benign breast disease, endometrial and ovarian cancer, and pelvic inflammatory disease.
5.5.3 Disadvantages of COCs
Although they are advantageous in many cases, COCs have some disadvantages, and you should inform your clients about these disadvantages in order to help them choose from all available methods.
One of the main disadvantages of COCs is that they are not recommended for breastfeeding women, because they affect the quality and quantity of milk. Very rarely, COCs can also cause strokes, blood clots in deep veins of the legs, or heart attacks. Those at highest risk are women with high blood pressure and women who are aged 35 years or older. Also bear in mind that the pills do not protect against STIs, including AIDS.
5.5.4 Disadvantages of mini-pills
For women who are not breastfeeding, the most common side-effects are: changes in menstrual bleeding including irregular periods, spotting or bleeding between periods (which is common), and amenorrhoea or missed periods (which is less common, but may continue for several months). Note that some women see amenorrhoea as an advantage. A few women may have prolonged or heavy menstrual bleeding.
Breastfeeding women normally do not have regular periods for some months, whether or not they are using progestin-only oral contraceptives. Therefore, menstrual changes due to progestin-only oral contraceptives generally are not noticed or bothersome. Progestin-only oral contraceptives may lengthen amenorrhoea during breastfeeding. For women who are not breastfeeding, even taking a pill more than a few hours late can increase the risk of pregnancy, and missing two or more pills increases the risk greatly.
5.6 Side-effects and drug interactions
5.6.1 Common side-effects
Most women who take the pill do not develop any side-effects. However, a small number of women develop nausea, headaches, sore breasts, mood changes, spotting between periods, or irregular bleeding. These side-effects usually go away within days or weeks of starting the pill. If they persist, a different brand of pill may suit better.
Other side-effects are less common and include tiredness, changes in sex drive, skin changes and mood changes. Although these are unusual, if the user experiences such problems for a prolonged period you should advise them to see a doctor or health officer.
The pill sometimes causes an increase in blood pressure (hypertension). In this case, how would you best advise the user?
The best advice to give is that those who are using oral contraceptives and complain about having hypertension need to have their blood pressure checked every six months. The pill may need to be stopped if their blood pressure becomes too high.
5.6.2 Management of common side effects
If a client experiences common side-effects, such as nausea, mild headaches, mood changes, tender breasts, spotting between periods and irregular bleeding, you should advise the woman to keep taking her pills. Skipping pills may make these side-effects worse. Also, skipping pills risks pregnancy. For spotting or irregular bleeding, she can try taking each pill at the same time of day. You should reassure her that these are not signs of more serious problems and they usually go away within three months. Urge her to keep taking her pill every day.
If she is not satisfied with your counselling, however, you may need to help her choose another method. If she vomits for any reason within two hours after taking a hormonal pill, she should be advised to take another hormonal pill from a separate packet. (Give her extra pills to take if she vomits.) If she has had severe diarrhoea or vomiting for more than 24 hours, which is not caused by low-dose combined oral contraceptives, she should follow the instructions for missed pills in section 5.4.1. Diarrhoea or vomiting may reduce effectiveness in the same way as missing pills.
Do you need to see your client again after giving them oral contraceptives (both COCs and mini-pills)?
You should invite your client to return if she needs help with any problems, or if she has any concerns. Let her know that she can switch to another method any time she wishes, and explain the specific reasons for seeing a health officer or doctor. Refer back to Section 5.6.1 for problems that require medical attention.
5.6.3 Drug interactions
The effectiveness of oral contraceptives, both COCs and mini-pills, are lowered when taken with certain medications, including antibiotics, anti-seizure, anti-tuberculosis, and migraine medications. If a woman is taking any of these medications that could interfere with the pill, she needs to tell you so that you can advise her to consider adding a back-up method of birth control, like condoms and/or spermicide. As with all drugs, it is useful to all clients who are using hormonal birth control to inform their medical providers when they seek any other medical care.
Summary of Study Session 5
In Study Session 5, you have learned that:
- The combined oral contraceptive (COC) pill, oral contraceptive (OC) pill, and often just called the pill, is the most popular type of birth control. There are many different brands, and they come in packs of 21 or 28 pills. Two brands, Microgynon and Leo-femenal, both in packs of 28 pills, are the most popular ones in Ethiopia. Progesterone-only oral birth control pills, or mini-pills, come in packs of 28 pills, and users take one every day. They contain a synthetic form of the progesterone hormone called progestin and no oestrogen.
- The pill works mainly by changing the body’s hormonal balance so that the woman does not ovulate. It works by stopping an egg (ovum) from being released each month from an ovary, and by forming a mucus plug so that sperm cannot get into the uterus to fertilise the egg. The pill also makes the lining of the uterus thinner, which makes it unlikely that a fertilised egg will be able to attach to the uterus.
- If used correctly and consistently, the combined oral contraceptive pill is 99.9% effective. In lactating mothers, the progestin-only pill is more effective than the combined oral contraceptive pill, because breastfeeding itself provides some protection against pregnancy.
- Pills are a particularly attractive contraceptive option for women who are happy to take a daily dose and be in control of their own bodies.
- Women who are over 35 years should not take the pill if they have a history of heart attacks or strokes, blood clots, unexplained vaginal bleeding, known or suspected cancer, known or suspected pregnancy, or liver disease.
- In the mini-pill, there are hormones in all 28 pills, and no spacer pills. It is important to take a pill every day, preferably at the same time each day. Forgetting a mini-pill or taking it late increases the chance of pregnancy more than missing a COC pill. Therefore, a woman should not stop taking the mini-pill unless she wants to get pregnant or to use another method of birth control.
- One of the advantages of COCs is that when taken consistently and correctly, they are very effective contraceptives that give women control over their own fertility. Most women can safely use pills throughout their reproductive years as long as they want to prevent pregnancy.
- The major advantage of the mini-pill is that it can be used by nursing mothers, beginning six weeks after childbirth, and the quality and quantity of breastmilk is not affected.
- One of the disadvantages of COCs is that they are not recommended for breastfeeding women, because they do affect the quality and quantity of breastmilk.
- Most women who take the pill do not develop any side-effects. However, a small number of women develop nausea, headaches, sore breasts, mood changes, spotting between periods or irregular bleeding.
- If a woman who takes the pill experiences common side-effects, such as nausea, mild headaches, mood changes, tender breasts, spotting between periods or irregular bleeding, you should reassure her that these are not signs of more serious problems and they usually go away within three months.
- The effectiveness of oral contraceptives, both COCs and mini-pills, are lowered when taken with certain medications, including antibiotics, anti-seizure, anti-tuberculosis, and migraine medications.
Self-Assessment Questions (SAQs) for Study Session 5
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module
SAQ 5.1 (tests Learning Outcome 5.2)
There are a lot of misconceptions about the use of oral contraceptives. List all the myths and rumours common in your community, and describe what you will do to overcome such problems.
Answer
There are a lot of misconceptions about the use of oral contraceptives. Some of those listed in Section 5.1 may also be common myths in your locality. In addition, the following misconceptions are sometimes cited:
- Some societies believe that oral pills cause severe heartburn if not taken with milk, so those who are not able to get milk should not take the pill.
- Some still perceive taking a pill is not allowed by God.
- Others say pills cause obesity and sometimes interfere with menstruation.
None of these are true.
SAQ 5.2 (tests Learning Outcome 5.3)
Explain how oral contraceptives work.
Answer
The pill works by altering the body’s reproductive hormone balance. As a result, the following occurs:
- The woman does not release an egg (ovum) each month from one of her ovaries, so ovulation cannot take place.
- The cervical mucus becomes thickened and forms a ‘mucus plug’ which makes it difficult for sperm to get through to the uterus (womb) to fertilise an egg.
- The lining of the uterus gets thinner and thinner. This makes it unlikely that a fertilised egg will be able to attach to the uterus.
SAQ 5.3 (tests Learning Outcome 5.4)
A woman who has forgotten to take three COC pills in the second week of her last menstrual period comes to your health post for help. What would you advise?
Answer
If a woman who forgot to take three COC pills in the second week of her last menstrual period comes to your health post, you may tell her she should take the following actions.
- Take a pill as soon as possible.
- Take the next pill at the usual time. This may mean taking two pills on the same day, or even at the same time.
- Continue taking active pills (see Figure 5.1) as usual, one each day.
SAQ 5.4 (tests Learning Outcomes 5.1 and 5.4)
Suppose one of your clients who is using COCs complains of a severe headache, vomiting and blurred vision. She is worried about becoming pregnant if she stops taking her pills. What would you tell her to help her?
Answer
Firstly, you should check her blood pressure to see if it has increased. In any case, these symptoms are serious and require medical intervention. So, you need to tell her to seek medical advice at the hospital or health post.
SAQ 5.5 (tests Learning Outcomes 5.4)
What is the major difference between COCs and mini-pills? Who would be eligible to use the mini-pill?
Answer
The major difference between COCs and mini-pills is that there are two hormones in COCs (progesterone and oestrogen), while mini-pills contain only one hormone (progesterone). All women are eligible to take mini-pills, but they are most suitable for breastfeeding mothers, as they do not interfere with breastmilk.
SAQ 5.6 (tests Learning Outcome 5.5)
Compare the main advantages and disadvantages of COCs and mini-pills.
Organise your comparison into a table.
Answer
The table below summarises the main advantage and disadvantages of COCs compared to mini-pills.
| Advantages | |
|---|---|
COCs
| Mini-pills
|
| Disadvantages | |
COCs
| Mini-pills
|
SAQ 5.7 (tests Learning Outcome 5.6)
A client using COCs develops pulmonary tuberculosis. What do you think would be important to tell her with regard to her contraception?
Answer
If one of your clients who is using COCs has developed pulmonary tuberculosis and been put on anti-tuberculosis drugs, you should advise her to switch her contraceptive method from COCs to a mechanical method, such as condoms or IUCD, so that she will avoid any drug interactions or possible side-effects.