Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Thursday, 5 February 2026, 8:52 AM
Family Planning Module: 6. Injectable Contraceptives and Contraceptive Implants
Study Session 6 Injectable Contraceptives and Contraceptive Implants
Introduction
This study session introduces the types of long-acting hormonal contraceptives which are injectable, or take the form of implants inserted under the skin of the upper arm. Once given to clients, a constant dose of hormonal contraceptives is released slowly into the body, making them very effective over long periods of time. In this study session, you will learn about these methods, their mechanism of action, effectiveness, advantages and disadvantages, and the most common side-effects. You will also learn about the management of side-effects related to these long-acting hormonal contraceptives.
Learning Outcomes for Study Session 6
When you have studied this session, you should be able to:
6.1 Define and use correctly all of the key words printed in bold. (SAQs 6.1, 6.2, 6.4 and 6.5)
6.2 Describe the main types of injectable contraceptives, their mechanism of action, effectiveness, advantages and disadvantages, mode of injection, and management of common side-effects. (SAQs 6.2, 6.4 and 6.6)
6.3 Describe the main types of contraceptive implants, their mechanism of action, effectiveness, advantages and disadvantages, insertion procedures, and management of common side effects. (SAQs 6.3 and 6.6)
6.4 Discuss common infection prevention precautions for injections and implant insertion. (SAQ 6.7)
6.1 Injectable contraceptives
Injectable contraceptives are artificial hormonal preparations administered by a deep intramuscular injection into the muscle of the arm or buttock, to be effective immediately. From the injection site they are slowly absorbed into the bloodstream and the body gets sufficient levels of hormone to provide contraception for one to three months, depending on the type of injectable contraceptive used. Injectable contraceptives can consist of progesterone-only preparations, or combined oestrogen and progesterone preparations (Figure 6.1).

6.1.1 Progesterone-only injectable contraceptives (POIs)
DMPA (Depo-Provera)

DMPA (Depot Medroxy Progesterone Acetate, or Depo-Provera) is an artificial progestin preparation which resembles the naturally occurring female hormone progesterone. It is usually given in doses of 150 mg, which gives three months’ protection following injection. It is the most widely available and commonly used injectable contraceptive in Ethiopia.
In what situations would you advise a client to choose an injectable contraceptive over an oral contraceptive?
When the client wants to prevent pregnancy for a long period of time, and is having difficulty remembering to take an oral contraceptive pill on a daily basis, then having an injectable contraceptive every month is preferred (Figure 6.2).
Mechanism of action of DMPA
In Study Session 5 of this Module, you learnt the mechanism of action of progesterone-only oral contraceptives. Progesterone-only injectable contraceptives have the same mechanism of action as that of the progesterone-only oral contraceptives, except that injectable contraceptives have a longer duration of action.
Can you explain how progesterone-only contraceptives prevent pregnancy?
Progesterone-only contraceptives, including progesterone-only injectables (POIs), prevent pregnancy in the following ways:
- Inhibition of ovulation (the primary mechanism of action)
- Thickening of cervical mucus to stop sperm penetration
- Thinning of the endometrium of the uterus to make it unfavourable for implantation of the fertilised egg
- Slowing of sperm and ovum transport through reduced fallopian tube peristalsis (wave-like muscular contractions of the fallopian tube by which contents are forced onward towards the uterus).
How effective is DMPA?
DMPA is very effective. In the first year of use only about 0.3 pregnancies per 100 women occur, that is, one pregnancy for every 333 clients who do not get pregnant, providing the injection is given every three months (Figure 6.3).

Why do you think injectable contraceptives are more effective when compared to oral contraceptive pills?
Injectable contraceptives avoid passage through the gastrointestinal tract, and metabolism in the liver.
Advantages of DMPA
DMPA is very effective, and has the advantage for the client that it can be used privately without the knowledge of any other person, including their partner. It also has the advantage of being long acting, but reversible if the client later decides to have a child. Moreover, it does not interfere with sexual intercourse. It is also suitable for breastfeeding women (after six weeks post-partum) because it has no oestrogen side-effects.
DMPA has proved to protect against ectopic pregnancy, since ovulation does not occur. However, if ovulation does occur, the chance of ectopic pregnancy is higher than for women not using DMPA. Why does this happen? This is because DMPA reduces fallopian tube peristalsis, which in turn slows the transportation of fertilised eggs from the fallopian tube to the endometrium and, as a result, there is a high chance of implantation in the fallopian tube.
It is important for you to know some of the other contraceptive benefits of DMPA. Scientific research has shown that it helps prevent uterine tumours, may protect against pelvic inflammatory disease by making the cervical mucus thick and impenetrable for microorganisms, and finally it reduces the chance of seizures in women with epilepsy. The advantages and disadvantages of DMPA are summarised in Table 6.1.
Disadvantages of DMPA
In most women, the use of DMPA is associated with disturbance of the menstrual cycle. This can include absence of menstrual periods or monthly bleeding (amenorrhoea) for an unspecified period of time. Also, there can be prolonged menstrual flow, light vaginal bleeding at any time other than during the menstrual period (spotting between periods), or heavy bleeding, which usually occurs during the first two to six months of use. It can increase the appetite of some women, resulting in weight gain. It does not protect couples against sexually transmitted infections (STIs), including the human immunodeficiency virus (HIV).
There can be a delayed return to fertility after stopping DMPA. Most women take an average of four to six months longer than usual to get pregnant, but this may extend to one year in some women. This is because residual levels of DMPA exist for several months in the body after the end of contraceptive protection following the final injection.
Do DMPA injectable contraceptives cause infertility?
No, DMPA does not cause infertility. It is a completely reversible contraceptive, but after stopping DMPA there can be a delayed return to fertility of four to six months.
| Advantages | Disadvantages |
|---|---|
Very effective. | Disturbance of menstrual cycle. |
Maintains privacy. | Delayed return of fertility. |
Reversible. | No protection against STIs. |
Suitable for breastfeeding women; no oestrogen side-effects . | Increased appetite causing weight gain for some women. |
Best choice for those with gastritis or peptic ulcer diseases (ulcer of stomach or duodenum). Protects against ectopic pregnancy. | Other side-effects include headache and dizziness, breast tenderness, nausea, hair loss, acne and loss of sexual feeling. If ovulation occurs, the chance of ectopic pregnancy increases. |
Management of side-effects and problems of injectable contraceptives
DMPA cannot be given to all women. In particular, it is not recommended for pregnant women, or those with breast cancer, or where a client has a history of diabetes (increased blood glucose level), advanced heart or liver disease, severe hypertension (increased blood pressure), or frequent severe headaches.
If a woman comes to you with concerns associated with this injection, do not underestimate or ignore her. Reassure her that the side-effects are not dangerous. Remember that counselling after side-effects have occurred is still useful, but not best practice. The best time to counsel a client about side-effects is when they make their contraceptive method choice. This is because many women encountering side-effects may not come to you at all, so it is important that you have given them the information beforehand.
First, you should advise her to wait until the effective days of the injection have passed. Then, if she is concerned about not having her monthly period, for example, she may want to change to another method. With irregular bleeding, reassure her that it is not harmful and usually reduces or stops after the first few months of use. On the other hand, if the bleeding is profuse and continuous, you should refer her for further investigation and management at the health post or hospital, as there may be another cause.
If she is suffering from headaches, suggest she takes Aspirin (500 mg), Ibuprofen (400 mg) or Paracetamol (500 mg), as needed, and provide her with the pain killer of her choice. Be aware that Aspirin and Ibuprofen may not be tolerated by a woman with gastritis or peptic ulcer diseases. In general, if her condition is severe, or if she is unhappy with your advice, refer her to the nearest health centre or hospital.

Timing of, and techniques for, DMPA injections
Box 6.1 summarises the most appropriate times to start DMPA injectable contraceptives.
Box 6.1 When to start DMPA injections
- In the first seven days after menstrual bleeding starts.
- Six weeks after childbirth, or at any time once menstruation has returned, indicating the woman is not pregnant.
- Immediately, or on the seventh day after childbirth, if your client is not breastfeeding.
- Immediately, or on the seventh day after a miscarriage or abortion.
- Immediately after stopping another method.
![]() The injection site should not be massaged or pressurised, as this may accelerate absorption of the drug.
The injection site should not be massaged or pressurised, as this may accelerate absorption of the drug.
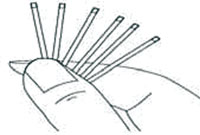
Injectable hormonal contraceptives are different from other injections because they are administered using deep intramuscular injection techniques (Figure 6.4). The vial must be shaken strongly before it is drawn into the syringe, to ensure the active ingredient is in suspension and not in the bottom of the vial. Following the procedure, the injection site should not be massaged or pressurised, because this may accelerate absorption of the drug. Infection prevention procedures are important (see Section 6.3 of this session).
Reinjection schedule
When the client comes to you to have her next or subsequent injection, you should check your records to see when you last gave her an injection. If it is the correct appointment date, give her the injection. If she comes to you up to two weeks before her appointment, or up to one month after her scheduled appointment, you can still give her the injection. But if she is more than one month late, she can get another injection that day only if you can be sure that she is not pregnant.
She is unlikely to be pregnant if:
- she has had no sex since the day of her last injection
- she has used condoms or another method every time she has had sex since the end of her last injection
- she had a baby less than six months ago, is fully, or nearly fully, breastfeeding, and has not had her period since
- she has taken emergency contraceptive pills after every sex act since her last injection.
Noristerat
Noristerat (NET-EN or norethisterone enanthate) is another artificial progestin preparation which resembles the natural female hormone progesterone. It is usually given in doses of 200 mg which gives two months’ protection after injection. It suits clients who want to prevent pregnancy for a relatively shorter period than DMPA users. Although this method is not available in Ethiopia, it is important to understand that all the mechanisms, effectiveness, advantages and disadvantages are similar to DMPA, except that its duration of action is shorter.
6.1.2 Combined injectable contraceptives (Mesigyna)
Mesigyna is a combination of a short-acting oestrogen and long-acting progesterone that is administered by intramuscular injection to give protection for one month. It is not available in Ethiopia at the moment; however it may come in the future. Note that all of its actions and effectiveness are similar to combined oral contraceptives.
6.2 Contraceptive implants
A contraceptive implant is a reversible, long-acting progestin which resembles the natural hormone progesterone in a woman’s body. It consists of flexible tubes or rods, each about the size of a match stick, inserted under the skin of a woman’s upper arm by a trained professional. Implants can give continuous protection for three to seven years, depending on the number of rods inserted. This method of contraception has been used for more than 25 years. There are four types of contraceptive implants used today. These are Norplant, Jadelle, Implanon and Sino-implant, according to their sequence of discovery. In this section, you will learn about their mechanisms of action, effectiveness, advantages and disadvantages, side effects, and how to manage the side effects.
6.2.1 Norplant
Norplant is a progestin-only contraceptive implant that consists of six rods inserted into the upper arm of the client to five to seven years of protection (see Figure 6.5). Its effectiveness decreases from five years onwards so women are advised to have it removed five years after insertion. It was the first implant to be introduced (25 years ago), and its manufacture was phased out in 2004. Although it is no longer available, it is important for you to know about it, so that you can advise those who have had Norplant implants inserted previously.
6.2.2 Jadelle

Jadelle is a progesterone-only contraceptive implant consisting of two rods implanted (instead of 6 rods in Norplant) to give effective protection for five years. Each rod contains 75 mg Levonorgestrel (150 mg in total). It is a new product, manufactured to replace the Norplant implant. By reducing the number of rods from six to two (Figure 6.6), it has made it easier to insert and remove. This method is in use in Ethiopia, and is provided by many trained health professionals in health centres and hospitals. After appropriate training, you may be able to insert Jadelle.
6.2.3 Sino-implant
Sino-implant is another contraceptive implant of two rods prepared from progestin, and is similar to Jadelle. It is effective for five years. It was introduced after Implanon and is available in Ethiopia, but at the time of writing it has not been approved by the Ministry of Health for use in Ethiopia.
6.2.4 Implanon
Implanon is a single-rod contraceptive implant prepared from another type of progestin, which gives effective protection for three years (Figure 6.7). It looks like a small flexible plastic matchstick. It can be inserted into the arm following a simple procedure, similar to an injection, and you do not need to make an incision as with other implants. Implanon is the best option for women who have had one or more children, or who may want children in the future. It has been introduced for use in Ethiopia, and has been approved by the Ministry of Health to be provided by you at health post level, once you have been given proper training.

Wozero Misgane has two children and works hard on her land. She recently asked you for advice on the most suitable contraceptive method for her. She explained to you that she is worried about the side-effects, that she might want more children again in the future, and that she works hard on her farm, so she needs a contraceptive that does not make her weak.
What would you advise for Wozero Misgane?
You may recommend Implanon for her as it is used by many women like her in Ethiopia and tell her that once it is removed she will be able to become pregnant.
W/ro Misgane decided to have the Implanon rod insertion. Six months later she told other women in her neighbourhood that it was the right contraceptive method for a rural hard-working woman like herself because she has had no side-effects and she has continued working hard without any ill effect.
How implants work
The mechanism of action of implants is similar to progesterone-only oral contraceptive pills and injectables, regardless of their route and duration of effectiveness.
How do implants prevent pregnancy?
Implants have the following effects:
- They stop the release of the egg from the ovary by slowly releasing progestin (an artificial progestrone) into the client’s body.
- The progestin in implants causes thickening of the cervical mucus, which makes it harder for sperm to move through the cervix.
- The progestin also causes thinning of the endometrial lining, making it less likely that a fertilised egg will implant in the uterus.
- Progestin slows the transportation of eggs along the fallopian tube by reducing peristalsis.
Effectiveness of contraceptive implants
Implants are more than 99.9% effective when they are inserted correctly (WHO, 2007). This means that less than one woman in 1,000 will get pregnant in the first year of use. There is no reported difference in contraceptive effectiveness or continuation rates among users of the various types of contraceptive implants. However, the effectiveness of contraceptive implants quickly reduces if women weigh more than 70 kg. In this case the implant needs early replacement, as early as one year before the intended year.
Advantages
Implants are very effective when compared to other contraceptive methods, and are particularly useful for women who know they do not want to get pregnant for a while. Once the implant is in place, the client does not have to think about contraception for the period of the implant. It is also a good choice of method for women who can’t use any contraceptive that contains oestrogen, and for women who find it difficult to regularly take a pill at the same time every day. For these reasons, its continuation rate is high.
Disadvantages

Implants require a trained provider (Figure 6.8) to insert and remove the rods. When the implant is first inserted into the upper arm, the woman may feel some bruising, tenderness or swelling at the insertion site. For most women, during the first year of implant, their menstrual cycle may become irregular, lighter, heavier or longer. This usually settles down after the first year. In some clients, periods stop completely (amenorrhoea), but this is not harmful. Your client should be aware of these issues before deciding to have the implant. As with other contraceptives, this method does not protect couples from STIs. In this case, the client is advised to use condoms, as well as having an implant.
In addition to the disadvantages listed above, side effects which are associated with the use of contraceptive implants include weight gain, nervousness, anxiety, nausea, vomiting, dizziness, dermatitis/rashes, abnormal or heavy growth of hair over the body (hirsutism), hair loss, headaches, depression and acne. Sometimes pain, itching, or infection at the site of the implant will occur.
Managing side-effects and problems with implants
Listen to your client’s worries and complaints and treat her concerns accordingly, referring her for further help if needed. If the client wishes, it is always possible to change to another method. Side-effects are similar to those of progesterone-only injectable contraceptives (see Box 6.2), and can be managed as instructed in the earlier part of this study session.
Box 6.2 When implants should not be given
Implants should not be given to women who have:
- serious liver disease
- problems of blood clots
- unexplained vaginal bleeding
- and/or had breast cancer.
Timing of contraceptive implant insertion and removal
Implants can be inserted at any time during the menstrual cycle, preferably within seven days of menstruation or post-abortion. It can also be inserted six weeks after delivery if the mother is fully breastfeeding. Generally, it can be inserted at any time, providing it is possible to confirm that the woman is not pregnant.
![]() Contraceptive implant insertion and removal requires special training and should only be practiced under direct supervision.
Contraceptive implant insertion and removal requires special training and should only be practiced under direct supervision.
Implants can be removed:
- at any time during the menstrual cycle.
- at the end of five years of use for Norplant or Jadelle, or three years of use for Implanon, when their effectiveness drops after the intended years of use, and the risk of intrauterine and ectopic pregnancy may increase.
- if the client wishes, at any time it is possible to remove an implant after providing the necessary counselling.
The removal of an implant is not a very complicated procedure, but it does require special training and practice under direct supervision. Following removal of any implants, the level of hormonal prevention drops quickly, and the women’s fertility returns within two to six months.
6.3 Infection prevention procedure
When carrying out any procedure, it is important to prevent the spread of infection by using proper infection prevention procedures. Microorganisms live everywhere in our environment. We normally carry them on our skin and in our bodies. Microorganisms are also found in animals, plants, soil, air and water. Some of these microorganisms can cause infections. Therefore, when you perform any procedure, it is very important to follow the principles of infection prevention precautions detailed in Box 6.3.
Box 6.3 Infection prevention precautions
- Create an infection-free environment by making it very clean, and avoiding the use of unclean materials.
- Handle all items from all clients as if they are contaminated.
- Use barriers such as gloves that serve to break the disease transmission cycle (see your Communicable Diseases Module).
- All disposable materials, such as gloves, syringes and needles, should be discarded into a safety box (Figure 6.9).

When you carry out any invasive procedure, you have to wash your hands thoroughly using water and ordinary soap. You must wear gloves during implant insertion to prevent the transmission of infection. It is mandatory to use an antiseptic, for example Savlon, alcohol or iodine solution, for cleaning wounds or the skin prior to the implant insertion procedure.
Summary of Study Session 6
In Study Session 6, you have learned that:
- Long-acting hormonal contraceptives include injectable contraceptives and contraceptive implants, in which hormones are released slowly to be absorbed into the bloodstream so that the body maintains a constant hormonal level sufficient to provide contraception safely and effectively.
- Injectable contraceptives are administered by a deep intramuscular injection into the muscle of the upper arm or buttock, to be effective immediately.
- DMPA (Depo-Provera) is an artificial progestin preparation (150 mg only) which resembles the female hormone progesterone and gives three month’s protection after injection.
- Noristerat (NET-EN) is an artificial progesterone preparation (200 mg only) which gives two months’ protection after injection.
- Mesigyna is a combined injectable contraceptive, which is a combination of short-acting oestrogen and long-acting progesterone. It gives one month’s protection. For the moment it is not available in Ethiopia.
- Contraceptive implants consist of flexible tubes or rods which are inserted under the skin of a women’s upper arm by a trained professional. They contain long-acting progestin, which is similar to the natural hormone progesterone, and their effects are reversible.
- The Norplant implant gives five to seven years of protection. It has been phased out from use and replaced by Jadelle.
- Jadelle is a contraceptive implant consisting of two rods, which give five years’ effective protection.
- Implanon is a single-rod contraceptive implant that gives three years’ protection. It has been introduced for use in Ethiopia, and has been approved by the Ministry of Health to be provided by Health Extension Practitioners at health post level after appropriate training has been given.
- When you are carrying out any invasive procedure, you must be careful to prevent the spread of infection by using proper infection prevention procedures.
Self-Assessment Questions (SAQs) for Study Session 6
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 6.1 (tests Learning Outcome 6.1)
What kind of contraceptive method is good for lactating (breastfeeding) women?
Answer
While non-hormonal methods are better, DMPA and other progesterone-only contraceptives would be the next best choice for lactating women. If the mother is not fully breastfeeding, or if menstruation has resumed, DMPA or a progesterone-only pill can be started as early as six weeks after delivery.
SAQ 6.2 (tests Learning Outcomes 6.1 and 6.2)
Match the correct protective period with each of the hormonal injectables and contraceptive implants.
Two lists follow, match one item from the first with one item from the second. Each item can only be matched once. There are 6 items in each list.
3 months
2 months
5–7 years
5 years
3 years
5 years
Match each of the previous list items with an item from the following list:
a.Implanon
b.DMPA
c.Jadelle
d.Sino-implant
e.Norplant
f.Noristerat
- 1 = b,
- 2 = f,
- 3 = e,
- 4 = c,
- 5 = a,
- 6 = d
SAQ 6.3 (tests Learning Outcome 6.3)
How long does it take to become pregnant after the implants are removed? Why?
Answer
Women who stop using contraceptive implants can get pregnant as quickly as if they had stopped a non-hormonal contraceptive method. This is because contraceptive implants do not delay the return of fertility once they have been removed.
SAQ 6.4 (tests Learning Outcomes 6.1 and 6.2)
How do progesterone-only contraceptive injectables and implants prevent the occurrence of pregnancy?
Answer
Progesterone-only contraceptives prevent the occurrence of pregnancy because they:
- stop the ovaries from releasing an egg each month
- thicken mucus in the cervix, which prevents sperm cell entry to the uterine cavity
- thin the endometrium of the uterus, making it difficult for the fertilised egg to be implanted.
SAQ 6.5 (tests Learning Outcome 6.1)
Describe the best times to start DMPA to prevent pregnancy.
Answer
The best times to start DMPA to prevent pregnancy are:
- During the first seven days after menstrual bleeding begins.
- 6 weeks after childbirth, or at any time once menstruation returns, ensuring that the woman is not pregnant.
- After childbirth if the mother is not breastfeeding.
- Immediately, or in the seventh day after miscarriage or abortion.
- Immediately after stopping another method.
SAQ 6.6 (tests Learning Outcomes 6.2 and 6.3)
W/ro Marta had her Implanon inserted three months ago. She complains that she has been having irregular bleeding since insertion and wants to know what can be done to stop it. Aside from the spotting, she is happy about the method.
Why has she developed this side effect?
How can you help her manage it?
Answer
Menstrual irregularity, or inter-menstrual bleeding, or total absence of menstruation (amenorrhoea) are common side effects of Implanon caused by hormonal imbalance, specifically by excess progesterone in the woman’s body. In the absence of infection, reassure W/ro Marta that her bleeding pattern is very common and is normal, particularly during the first three to six months following insertion. If the bleeding is unacceptably high, refer her for further investigation and management to the nearest health centre or hospital.
SAQ 6.7 (tests Learning Outcome 6.4)
What are the most important infection prevention precautions you should take when doing any invasive procedure?
Answer
These are the most important infection prevention precautions:
- Wash your hands using water and ordinary soap.
- Wear protective barriers such as gloves.
- Use antiseptic prior to insertion/injection.
- Discard all disposable materials into a safety box.