Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Thursday, 19 February 2026, 12:08 PM
Family Planning Module: 7. Intrauterine Contraceptive Devices (IUCD)
Study Session 7 Intrauterine Contraceptive Devices (IUCD)
Introduction
Intrauterine devices (IUDs) have a long history. The first IUD, developed and marketed around 1900, was designed to occupy both the vagina and the uterus. By 1928 it had been modified to occupy only the uterus, which is the design in use today. An intrauterine device (IUD) is an effective, safe, long-acting, cost-effective contraceptive method used in many countries, including Ethiopia. It consists of a small, flexible plastic device inserted into a woman’s uterus and is left in place for long periods of time, providing continuous protection against pregnancy for a minimum of 10 years. It is also known as an intrauterine contraceptive device (IUCD), and we commonly use this term in the rest of the session. The copper-bearing IUCD brand TCu-380A is widely available in Ethiopia, and is the subject of this session.
In this study session, you will learn about the definitions, types, and mechanism of actions, the advantages and disadvantages, precautions, and the common side effects of IUCDs.
Learning Outcomes for Study Session 7
When you have studied this session, you should be able to:
7.1 Define and use correctly all of the key words printed in bold. (SAQs 7.1 and 7.3)
7.2 Explain the mechanism of action of IUCDs. (SAQs 7.1 and 7.3)
7.3 Discuss the effectiveness of IUCDs. (SAQs 7.2 and 7.3)
7.4 Describe the insertion and removal of IUCDs. (SAQ 7.3)
7.5 Discuss the advantages and disadvantages of IUCDs. (SAQs 7.3, 7.4 and 7.5)
7.6 Explain absolute and relative precautions for IUCDs. (SAQs 7.5 and 7.6)
7.7 Identify common side-effects and their management for IUCDs. (SAQs 7.3 and 7.5)
7.1 Types of IUCD
There are three different types of IUCD. These are:
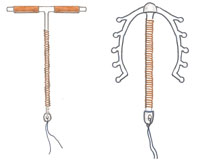
- copper-bearing IUCDs, which are made of plastic with copper sleeves and/or copper wire on the plastic, such as TCu-380A and MLCu-375 (see Figures 7.1 and 7.2).
- hormone-releasing IUCDs, which are made of plastic and steadily release small amounts of progesterone or other progestin hormones, such as LNG-20 and Progestasert.
- inert or unmedicated IUCDs, which are made of plastic or stainless steel only, such as Lippes Loop and Chinese stainless steel rings.
Copper T 380A is one of the three which is most commonly available and widely used in many countries, including Ethiopia. In this study session, you will learn about the Copper T IUCD in detail.
Copper T 380A
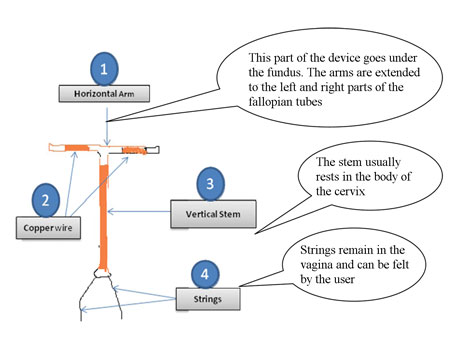
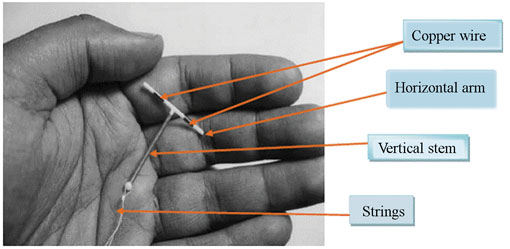
The Copper T 380A IUCD is a T-shaped device made of polyethylene (plastic) and filled with barium sulfate so that it is visible on an X-ray. It is 3.6 cm in length and 3.2 cm in width (see Figures 7.1 and 7.2). There are small copper bands on each horizontal arm of the T, which is placed high in the fundus or highest point of the uterus. The vertical stem is also wound with copper wire, and a thin polyethylene string or thread is attached to the bottom of the stem for easy removal.
7.2 How copper-bearing IUCDs work
Copper-bearing IUCDs act primarily by stopping fertilisation. The copper slows down the movement of sperm within the woman’s uterus and so prevents them from reaching the fallopian tubes and fertilising the egg. The device also stimulates a strong reaction in the wall of the uterus, which prevents implantation of the egg (even if it is fertilised).
7.3 Effectiveness of IUCDs
An IUCD is a highly effective, long-term, reversible contraception. Using an IUCD can be as effective as female surgical sterilisation in preventing pregnancy, but unlike sterilisation it is a completely reversible contraceptive method. Among women who use the Copper T 380A IUCD, less than 1% become pregnant (0.6 to 0.8 per 100 women) during the first year of use. Additionally, the cumulative risk of pregnancy over the ten-year service life of an IUCD is less than 3%. In addition, fertility returns soon after removal.
The Copper T 380A can prevent a woman from becoming pregnant for up to 12 years. However, its effect is reduced after seven years of use, after which the likelihood of becoming pregnant increases. Some countries advocate its use for up to ten years, and it should be replaced or removed no later than ten years from the date of insertion. In the case of Ethiopia, you should refer to the National Family Planning Guidelines on recommended years of use.
An important point is that a woman’s fertility returns promptly after an IUCD is removed. You should make this very clear to women having an IUCD removed, i.e. they should have another IUCD inserted immediately after removal (if desired and appropriate), or immediately start another contraceptive method unless they want to get pregnant.
7.4 Insertion and removal
You will not be expected to insert or remove IUCDs. These procedures should be performed only by service providers who have been trained, such as physicians, nurses and midwives. However, it is important to understand the problems associated with IUCDs, such as IUCD expulsion, infection, and uterine perforation. These are not common, but when they do occur they are often due to improper insertion techniques.
Although IUCD insertion and removal procedures are relatively simple, there are several separate steps to be performed in a specific sequence. These steps must be integrated with the appropriate infection prevention and counselling measures, to help ensure the safety and wellbeing of the woman. At your level and setting it may be difficult to perform these procedures, but you need to tell women where to go and when to have such services.
7.4.1 When to start using an IUCD
An IUCD is usually inserted during a menstrual period, when the cervix is slightly open and pregnancy is least likely. There is, however, a greater chance of expulsion if a device is introduced early in the cycle, because the uterus can squeeze the device back out. Therefore, the best time for insertion is just after a period. However, an IUCD may be inserted at any time. Table 7.1 shows the best timing for IUCD insertion for women in different situations.
| Woman’s situation | When to start |
|---|---|
| Having menstrual cycles | • Any time within the first 12 days after the start of menstrual bleeding, preferably after bleeding has stopped, at the woman’s convenience. • Any other time during the menstrual cycle (not just during menstruation) if the woman is not pregnant and has a healthy uterus. • If a woman has been using a reliable contraceptive, or has not been having sex, the best time to insert her IUCD is when she asks for it. |
| After childbirth | • During a hospital or health centre stay following childbirth, if she has decided voluntarily in advance. The IUCD is best inserted within ten minutes of delivery of the placenta. • It can be inserted at any time within 48 hours after childbirth (special training is required). • If not immediately after childbirth, then as early as four weeks after childbirth for Copper T IUCDs, such as TCu-380A. At least six weeks after childbirth for other IUCDs. |
| After miscarriage or abortion | • Immediately, if no infection is present. • If an infection is present, treat it and help the client choose another effective method. • The IUCD can be inserted after three months, if no infection remains and re-infection is not likely, and the woman is not pregnant. |
| Lactating mothers with lactational amenorrhoea (LAM) | • Any time, providing the mother is not pregnant. |
| When stopping another method | • Immediately. |
7.4.2 Checking the IUCD
You should advise women that they can keep track of an IUCD by checking for its strings, and they can feel for the strings by putting a finger into their vagina. Some women prefer to look for the string with a mirror and flashlight. It is generally recommended that women check their IUCD after each period. A shorter than normal string can be a warning sign of a misplaced IUCD. Missing strings may mean that the IUCD has been expelled. If the string is missing, you should advise the woman to visit the health post or health centre in order to have a back-up method of birth control. If the woman misses a period while on an IUCD, she may need to take a pregnancy test.
7.5 Advantages and disadvantages
7.5.1 Advantages of the Copper T 380A IUCD
IUCDs are a highly effective, safe, long-acting contraceptive method. Women need to make only a single decision to use it, whereas the pill requires daily decisions, and condoms and spermicides require decisions with each act of intercourse. Although it is more expensive initially than other contraceptives, the IUCD is less costly over its years of use. Therefore, it is a cost-effective method that can be appropriate in poor countries like Ethiopia.
In addition, the IUCD is a good option for those who have to take medical precautions using hormonal methods, as there are no hormonal side effects with copper-bearing or inert IUDs. It does not interact with any medicine the client may be taking, so it is ideal for those who are taking antiepileptic or antituberculosis medications.
The IUCD is best used by those wanting a long-acting and prompt reversible method. A new device can be inserted without any gap as many times as a woman desires during her reproductive life. The Copper T 380A IUCD also helps prevent ectopic pregnancies (there is less risk of ectopic pregnancy than for women not using any family planning method).
When inserted within five to seven days of unprotected intercourse, the Copper T 380A gives good protection against unintended pregnancy (see Study Session 10, Emergency Contraception). Furthermore, since Copper T 380A IUCD does not affect the quantity and quality of breastmilk, it can be used by lactating women.
What are the main advantages of using IUCDs?
The main advantages are as follows:
- IUCDs are highly cost-effective long-acting contraceptives.
- IUCDs can be used by those who are not able to use hormonal methods.
- IUCDs do not interact with any medicines the client may be taking.
- IUCDs are appropriate for lactating mothers as they do not affect breastmilk.
7.5.2 Disadvantages of the Copper T 380A IUCD
IUCDs are not suitable for all women. Using them carries the following risks:
- Pelvic inflammatory disease (PID): One of the main concerns about using IUCDs is the possibility of developing PID. Both using an IUCD and being at high risk of acquiring sexually transmitted infections (STIs) make women more likely to develop PID. The greatest risk of pelvic infection associated with the use of IUCDs occurs at insertion. This increased risk of infection may be associated with a microbiological contamination of the endometrial cavity at that time.
- Human immunodeficiency virus (HIV): Whether IUCDs increase the risk of acquiring HIV is not known. The effect of IUCDs on the uterine lining may create an environment favourable to HIV transmission. It is possible that the increased bleeding associated with the use of some IUCDs may increase the transmission of the virus from HIV-positive women to their partners.
- Menstrual problems: Increased menstrual pain (dysmenorrhoea) may accompany IUCD use. Between 10%–15% of IUCD users have their IUCD removed because of symptoms or signs associated with bleeding or spotting. However, the amount of blood is usually minor and of little consequence.
- Expulsions: An IUCD may come out of the uterus, possibly without the woman knowing. This is more common when the IUCD is inserted soon after childbirth, or when there are abnormal amounts of menstrual flow or severe dysmenorrhoea (painful cramps during menstruation).
- Pregnancy: Half of intrauterine pregnancies that occur with the IUCD in place end in spontaneous abortion. If the IUCD is removed early in pregnancy, the spontaneous abortion rate drops to about 25%. Leaving the IUCD in place during pregnancy increases the risk that the mother will have severe pelvic infection that could lead to her death. About 5% of women who become pregnant with an IUCD in place will have an ectopic pregnancy.
7.6 Precautions when using IUCDs
7.6.1 Absolute contraindication
Contraindication is a term used to indicate that the administration of a drug, or the carrying out of a medical procedure, is inadvisable. Some women in your community will not be able to use IUCDs because of a medical or health condition, and you will need to advise them accordingly. Women with the following conditions are advised not to use IUCDs.
- Current pelvic inflammatory disease (PID): IUCDs can worsen pelvic infections as a result of microbiological contamination during insertion. A woman having such problems should be advised to use another method.
- Known or suspected pregnancy: Because of its toxic effect on the fetus, IUCDs can cause abortion in pregnant women. So, if you suspect a woman is pregnant, you should not recommend an IUCD.
- Undiagnosed irregular genital tract bleeding: This can be due to uterine cancers. So you should refer the woman to hospital for further investigation.
- Known allergy to any constituent of the device: You should advise a woman with any history of allergy to IUCDs not to use the device. Help her choose a different contraceptive method.
7.6.2 Relative contraindication
Some clients can use IUCDs with caution. If a woman comes to you for an IUCD and she has diagnosed valvular heart disease, a past history of PID (not active PID), abnormalities of the uterus resulting in a distorted cavity, a history of ectopic pregnancy, or a lowered immune response, you should advise her to first see a doctor for further examination.
7.7 Side-effects and managing side-effects
IUCDs cause very few side-effects. The most common are pelvic cramping and menstrual problems, including heavy and prolonged menstrual bleeding, and intermenstrual spotting. Although abnormal bleeding and spotting are the leading reasons for women to discontinue the method, these side-effects do not usually affect their health, and generally decrease in the first few months after insertion.
One potential, though uncommon, complication of IUCD use is device expulsion, which occurs in 2–8% of women. Expulsion occurs most often in the first few months after insertion, and it is most common in young women, and women who have never given birth. The IUCD can only be expelled outward into the vagina or cervix. It cannot travel to any other part of the body. Expulsion is not dangerous for the user; however, if the IUCD is expelled, the woman is no longer protected against pregnancy because the IUCD’s contraceptive effect is immediately reversible.
Although it is a rare event, uterine perforation during IUCD insertion is one of the complications which occurs in 0.5 to 1.5 per 1,000 insertions, and is associated with the level of the provider’s skill and experience.
Several additional IUCD-related complications include PID and ectopic pregnancy, but a woman’s risk of these is minimal, especially if she is free of STIs.
What are two of the key disadvantages of using IUCDs? How can they be overcome?
Uterine perforation during IUCD insertion is one of the complications which occurs in 0.5 to 1.5 per 1,000 insertions, and is associated with the level of the provider’s skill and experience.
The second complication is spontaneous expulsion.
These problems can be overcome through (1) mandatory skill training for the provider to minimise the risks and (2) effective counselling to reassure the woman.
Counselling women about side-effects and their possible complications, either at the time of insertion or at subsequent follow-up visits, is essential to ensure women’s satisfaction with this method.
Summary of Study Session 7
In Study Session 7, you have learned that:
- Three different types of common IUCDs are copper-bearing IUCDs (TCu-380A and MLCu-375), hormone-releasing IUDs (LNG-20 and Progestasert), and inert, or unmediated IUCDs (Lippes Loop). Copper T 380A is one of the most widely available IUCDs in many countries, including Ethiopia.
- Using an IUCD can be as effective as female surgical sterilisation in preventing pregnancy, but unlike sterilisation, it is a completely reversible family planning method.
- Although IUCD insertion and removal procedures are relatively straightforward, there are several separate steps to be performed in a specific sequence by a trained practitioner. These steps must be integrated with the appropriate infection prevention and counselling measures, to help ensure the safety and wellbeing of the woman.
- It is recommended that women check their IUCD after each period. A shorter than normal string can be a warning sign of an embedded IUCD. Missing strings may mean that the IUCD has been expelled.
- The main advantage of IUCDs is that they are a highly effective, long-acting, safe and cost-effective contraceptive method, and the client need make only a single decision to use an IUCD, compared with the daily decisions needed to take oral contraceptives.
- An IUCD is also a good option for those who have medical precautions in response to hormonal methods, as there are no hormonal side effects with copper-bearing or inert IUCDs. They do not interact with any medicine the client may be taking.
- Common disadvantages of IUCDs are that they require trained health personnel to insert and remove them. Also, the client needs to have a number of laboratory tests and pelvic examinations to rule out STIs, including an HIV test and a test for PID.
- IUCDs are absolutely not recommended for women who have the following health problems:
- Current pelvic inflammatory disease
- Known or suspected pregnancy
- Undiagnosed irregular genital tract bleeding
- Known allergy to any constituent of the device.
- One potential, though uncommon, complication of IUCD use is device expulsion. Expulsion occurs most often in the first few months after insertion, and it is most common in young women and women who have never given birth.
- Counselling women about common side-effects and possible complications of IUCD, either at the time of insertion or at subsequent follow-up visits, can ensure client satisfaction with the method.
Self-Assessment Questions (SAQs) for Study Session 7
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 7.1 (tests Learning Outcomes 7.1 and 7.2)
It is important to understand the parts of an IUCD. Make your own drawing of a Copper T IUCD, correctly labelling its parts and explaining its location in the uterus.
Answer
Your hand-drawn Copper T IUCD drawing should look something like this. See Figure 7.3.
SAQ 7.2 (tests Learning Outcome 7.3)
You have learnt that IUCDs are very effective in preventing pregnancies. Note down at least two ways in which a copper-bearing IUCD can interfere with fertilisation.
Answer
A copper-bearing IUCD can interfere with fertilisation in two main ways:
- The copper slows down the movement of sperm within the woman’s uterus to prevent sperm from reaching the fallopian tubes and fertilising the egg.
- The device can stimulate a strong reaction in the wall of the uterus, which prevents implantation of the egg even if it is fertilised.
SAQ 7.3 (tests Learning Outcomes 7.1, 7.2, 7.3, 7.4, 7.5 and 7.7)
Which of the following statements are false? In each case explain why it is incorrect.
A Loops and Copper T IUCDs are quite different in shape and size. Moreover, when compared with T IUCDs, loops are not widely used nowadays.
B The main purpose of the impregnated barium sulfate in an IUCD is that it interferes with fertilisation.
C Copper-bearing IUCDs can lose their effect when inserted into a woman who is taking anti-tuberculosis medication.
D The Copper T is a U-shaped, highly flexible device that any health professional can insert.
E If inserted and placed appropriately, expulsion of the Copper T IUCD is rare.
Answer
A is true. Loops and Copper T IUCDs are quite different in shape and size.
B is false because the main function of impregnated barium sulfate in IUCDs is to illuminate the location of the device in the uterus when an x-ray image is taken. It has nothing to do with fertilisation.
C is false because the copper-bearing IUCD acts locally and has no systemic effect in reacting with other drugs. Therefore it can be safely used as a contraceptive method by a woman who is taking antituberculosis medication.
D is false because in spite of its flexibility, it is not easy to insert a copper T IUCD into the uterus. You need special skills and training to do so. Therefore, health professionals who are not trained in such skills should not insert the device.
E is true. Expulsion of the Copper T IUCD is rare, if inserted and placed appropriately.
SAQ 7.4 (tests Learning Outcome 7.5)
A woman who is currently on oral contraceptives but wants to change her method to an IUCD comes to your health post and asks for information about the advantages of using IUCDs compared with oral contraceptives. What is your response?
Answer
IUCDs have the following advantages compared to oral contraceptives:
- They contain no hormones, so do not cause blood clots and heart attacks. Although it is very rare, oral contraceptives can have these side-effects.
- IUCDs act locally and do not affect other drugs. Therefore, an IUCD can be safely used as an optional contraceptive method by a woman taking anti-tuberculosis and/or anticonvulsion drugs.
- IUCDs can be a good choice for lactating mothers, as they do not affect breastmilk .
SAQ 7.5 (tests Learning Outcomes 7.5, 7.6, 7.7)
What are the advantages of IUCDs compared with oral contraceptives? You may find it helpful to refer back to Study Session 5, which covers the disadvantages and common side-effects of oral contraceptives for comparison.
Draw a table and list the disadvantages and side-effects of oral contraceptives in the left column, and try to match them against the relative advantages of IUCDs in the right column. This will help you to remember them.
Answer
The following table depicts the relative advantages of IUCDs compared with oral contraceptives.
| Disadvantages/side effects of oral contraceptives | Relative advantages of IUCDs |
|---|---|
|
|
SAQ 7.6 (tests Learning Outcome 7.6)
There are several groups of women who cannot use IUCDs at all. List them and explain why.
Answer
The following is a list of groups of women who cannot use IUCDs at all:
- Women with active PID cannot use IUCDs as they can worsen any pelvic infection as a result of microbiological contamination during insertion.
- Women who are known to be pregnant should not use IUCDs because they can cause toxicity to the fetus, which may result in abortion.
- Women who are suffering from undiagnosed irregular genital tract bleeding must consult a doctor before using an IUCD, as the bleeding could be due to uterine cancer. Using an IUCD with this condition can worsen the bleeding.
- Women who are known to be allergic to any constituent of the device should avoid using an IUCD because it may result in an undesirable health problem.