Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Thursday, 5 February 2026, 8:27 AM
Supporting children with complex needs
Introduction
Sometimes I think it would help to start with a blank piece of paper instead of sharing so much information about what they can and cannot do. Just get to know the child and you’ll learn what they like to do.
This quote is taken from an interview with Pamela, the parent of a child with complex medical needs. Pamela’s words highlight that the usual approach to learning how to support a child with complex needs often starts with discussions about the child and involves completing extensive reports and plans. Of course, it’s important to include these forms of communication, but Pamela’s view is that it may be more productive to take a different approach. She suggests that by meeting and observing the child, practitioners will be able to learn about the child and make their own assessment of what a child can do and what he or she may need support with doing.
Working with children with complex medical needs can be daunting – it may seem that you have a great deal to learn and you may lack confidence in your knowledge and ability at first. However, it’s important to remember that you will be part of a team that is likely to include other health professionals who will help you build your knowledge.
Working with parents and other health professionals involved in the care of children with complex medical needs is especially important. It will also be important that you and other practitioners in your setting can work together as a team. Teamwork involves developing good communication skills and listening carefully is a key skill that you may need to develop.

The content of Week 5 links to module learning outcomes (LO) 4 and 5:
- LO4 Be aware of the sources of support for ELC staff working with children with ASN.
- LO5 Identify the specialist and cross-professional support that is available to support children with complex ASN.
By the end of Week 5 you will be able to:
- know more about meeting the additional support required by children with complex medical needs
- identify how you can show leadership in meeting the needs of children with complex needs.
Continue to 5.1 Children with complex needs.
5.1 Children with complex needs
What do we mean by describing children as having complex needs? Before we answer that question, it may be helpful to consider the reasons that children may have complex medical needs.
Babies and children can have complex medical needs for any of the following reasons:
Genetic conditions, meaning an inherited condition from one or both parents. Such conditions include cystic fibrosis, Down’s syndrome and sickle-cell anaemia.
Congenital conditions, that is, conditions present at birth. They can be genetic conditions (as described above) or could be caused by an interruption to the growth and/or development of the embryo (up to the first three months of pregnancy) or foetus (from the third month of pregnancy). An example of a congenital birth condition caused by interruption to growth and development is spina bifida.
Birth trauma – a lack of oxygen to the brain during birth, for example, can lead to brain damage and
cerebral palsy .Injuries and trauma can cause damage to the brain or body that can result in the child developing complex medical needs.
Treatment for life-threatening conditions, which are conditions that require surgery, or ongoing medical conditions that can mean that a child will have complex medical needs. Examples of such conditions include cancer treatment or kidney failure that requires
dialysis or akidney transplant .

The number of children with complex medical needs is increasing. There are many reasons for this, including:
- improvements in antenatal care for mother and babies (Blair et al., 2010)
- increased survival rates of babies born early – the average length of pregnancy is 40 weeks, however 60 per cent of babies survive at 24 weeks of pregnancy (Tommy’s, 2019)
- improvements in surgery or medicine, including treatments for cancer (Blair et al., 2010)
- improvements in health professionals’ knowledge of treatment and management of complex cases (Blair et al., 2010)
These reasons explain why babies and children are surviving when previously they may not have. As such, this has led to an increase in the number of children with disabilities, some of which result in the child having complex medical needs.
Defining complex additional support needs
As the previous section highlighted, there are many reasons why a child may have complex medical needs. Each condition has complex contributing factors, and the effects on each child and family is unique. Therefore, having one definition that addresses all children is difficult to do.
How to define what is meant by ‘complex medical needs’ was discussed in detail in The Right Help in the Right Place at the Right Time: Strategic Review of Learning Provision for Children and Young People with Complex Additional Support Needs (2012). In the review, the author Peter Doran stated that:
The conclusion was that there was no neat and easy definition, because of the many factors which came into play and the range of support needs so wide and diverse. The term however was recognised as having value as it recognised that some children and young people required a complex set of arrangements and input from a numbers of specialist practitioners to allow them to progress. The review resisted defining complexity by condition in recognition that the need for complex support and specialist professional inputs can change or develop over time.
The National Strategic Commissioning Group (NSCG) therefore uses a working description rather than a definition.
Complex additional support needs may arise as the result of:
the severity of one or more factors resulting in need, and/or
the combined impact of a number of separate factors, one or more of which may be severe.
A rigorous, clearly bounded and universally accepted definition is extremely difficult to formulate because of the multiplicity of factors and the impact of specific contexts in different local authorities. For that reason the National Strategic Commissioning Group (NSCG) is using a working description rather than a definition of children and young people with complex additional support needs:
Those in receipt of a Co-ordinated Support Plan as defined in the Education (Additional Support for Learning) (Scotland) Act 2009, i.e. where:
a.an education authority are responsible for the school education of the child or young person,
b.the child or young person has additional support needs arising from
i. one or more complex factors, or
ii. multiple factors,
c.those needs are likely to continue for more than a year, and
d.those needs require significant additional support to be provided
i. by the education authority in the exercise of any of their other functions as well as in the exercise of their functions relating to education, or
ii. by one or more appropriate agencies (within the meaning of section 23(2)) as well as by the education authority themselves.
Children and young people aged 3–18 who do not have a co-ordinated support plan but who have been assessed as stage 3 or 4 by a local authority under a staged intervention model as recommended by the Supporting Children’s Learning Code of Practice.
Children and young people aged 3–18 who attend a grant aided or independent special school.
Exceptional healthcare needs
A smaller group of children require even more support and are described as having exceptional healthcare needs. You can read about this definition on NHS Scotland’s specialist website. (Look at the link in the further reading section for more detail.)
Each child is unique
When a child is described as having complex needs, we are also referring to the complexity of support that adults need to provide. As outlined in Doran’s quote in Section 5.1, their complex medical needs do not refer to a diagnosis or condition. Children with complex needs will have very varied experiences and are unique, competent and active learners whose potential needs to be encouraged and supported.
In Week 4 we heard about the importance of diagnosis and acknowledged the balance to strike between the usefulness of a diagnosis compared with how it might limit how we view a child. This can be even more challenging when a child has complex medical needs. It can sometimes feel that the child and all their personality is lost behind many medical labels. In this section we will look at the importance of providing appropriate support and the need to put medical information into perspective and focus on the whole child.
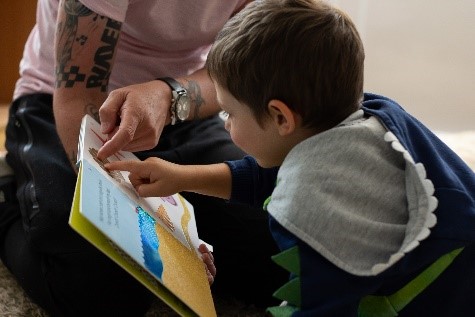
Watch this short film where Pamela, a parent, describes how she supported her daughter’s transition from home to nursery.

Transcript: Video 5.1 Transition from home to nursery
Imagine someone writing a description about you to someone else before you met them. Written information can be very useful but is no substitute for meeting the real person. Getting to know someone – whether it’s a child, a parent or another professional involved in a child’s care – requires listening skills that you will look at in the next section.
5.2 Communicating with children with complex needs
As discussed in Week 1, you already have tools to help you gain confidence when working with children who have complex medical needs and their families. Everyday skills such as the ability to listen carefully will help you learn about the child, and the ability to assess a child will help you to plan appropriately.
Children will communicate in different ways and as practitioners you should be alert to any attempts at communication. Practitioners should offer a variety of ways for children to communicate and should respond accordingly. A visual picture, an eye gaze or a sign are all ways of communicating and the approach – which accepts of all forms of communication – is referred to as ‘total communication’.
Because of the variation in ways that children with complex needs can communicate, you may find that you must develop new skills and gain new knowledge in order to be able to understand and care for a child with complex medical needs.
This section looks at some of the skills and knowledge in more detail, starting with the importance of listening skills and active listening.
Active listening
Listening to anyone is important. However, active listening goes beyond simply listening. Active listening involves close attention to what is being said and requires the listener to demonstrate that they have understood what is being conveyed.
Try starting up a conversation with somebody and listening to them for a while. Then try to remember what was said. It’s more difficult than you think, and the chances are you will only remember about half of what was said because we get distracted.
Active listening is a communication technique that requires the listener to concentrate, understand, respond and remember what is being said. To improve your listening skills when networking, practice making a conscious effort to not just hear the words that another person is saying but, more importantly, to understand the complete message. In order to do this you must pay attention to the other person very carefully. You cannot allow yourself to become distracted by anything else that may be going on around you, or by thinking about your reply to them. Nor can you allow yourself to get bored and lose focus on what the other person is saying.
Recognition
Give something back: a little bit of recognition in the form of a head nod or occasional ‘uh-huh’ lets the speaker know that you are still listening and helps keep you focused. As you heard earlier, nodding and maintaining eye contact also do this.
Paraphrasing
Paraphrasing is when you repeat back key pieces of information that the speaker has said, but in your own words. This demonstrates not only that you were listening, but that you have understood the speaker. It helps the speaker to be sure you have got the message and gives them an opportunity to correct any misunderstandings.
If you wish to develop your active listening skills further, you can do the extension activity at the end of this week, or perhaps you could consider doing a course to help you. Details of a free OpenLearn course are included at the end of this week.
Intensive interactions
Children with complex medical needs may benefit from intensive interaction; this is sometimes perceived to be a specialist approach and indeed there are specialist training courses available across the country. However, intensive interaction really refers to one-to-one intensive interaction sessions with children. This kind of approach is frequently used in ELC settings by trained staff, often with guidance from a Speech and Language Therapist.
For more information about this, please look at the NHS Education for Scotland guidance Breaking the barriers (2015).
Total communication approach
A total communication approach (also known as an ‘inclusive communication approach’) is something that everyone can do without specialist training. It is about finding and using the right combination of communication methods for each child. It is a holistic view of communication that considers all means and combinations of communication: signs, pictures or gestures, for example.
The Sense website has further information about total communication.
Building confidence and knowledge
Practitioners may be low in confidence if they have a lack of knowledge or experience in supporting children with complex medical needs. Each condition has a different effect on the child; children with complex needs require adults around them to develop the skills necessary to support them.
Some children may need help with mobility, so physiotherapy may be needed. Children with cystic fibrosis may need chest physiotherapy to help with breathing and reduce the risk of infection. Other children with complex medical needs cannot eat food orally and need to be fed via a tube. Providing the right support for children with complex medical needs can be daunting at first, because many new skills are needed. But learning new skills can be rewarding and will help raise confidence.

The following case study of a practitioner’s experience supporting a child with tube feeding illustrates this.
Case study – tube feeding
Case study – tube feeding
Karen, an ELC practitioner, reflects on how she supported a child who needed to be tube fed.
Jonah’s mum was about to return to work after having maternity leave and she came to visit the nursery to see if she thought that we were going to be the right kind of setting for her son. It was particularly important for her to find out if we were going to be able to support his additional needs.
When Jonah’s mum told me about the gastrostomy tube I started to feel panicky – I wasn’t at all sure that I was prepared to take responsibility for what seemed like such an important need. I didn’t know anything about tube feeding and was concerned that I might get it wrong and cause him pain or damage him in some way – and if that happened, how might the parents react? However, when Jonah’s mum started to tell me about Jonah and the tube, I started to feel less overwhelmed.
Jonah’s mum explained that a gastrostomy tube is fitted under general anaesthetic into the stomach. The outside portion of the tube remains outside the stomach. The feed is commercially produced and supplies the nutrition that Jonah needs. Jonah needs three liquid feeds a day and the feed is inserted into the tube over a ten-minute period. If the correct procedure is followed, which includes flushing the tube before and after the feed is given, the chances of it blocking off are minimal. To keep his tube as safe as possible he wears a close-fitting vest, which closes with poppers over his nappy.
His mum demonstrated how to give the feed and it was very straightforward to do. Jonah hardly took any notice and carried on playing as the feed was being given. I started to see that besides needing the tube feed, Jonah was not different to any other toddler of his age. After discussing the possibility of offering Jonah a place with the other staff, we decided that we would offer Jonah a place for a trial period of a month to see if we could manage.
To help me learn more about tube feeding I looked on the website of the specialist children’s hospital that was looking after Jonah. I felt it was important to speak with a health professional to find out more about Jonah’s additional needs, so Jonah’s mum gave us the contact details of the community paediatric nurse, who agreed to come about to the nursery. Ian was very helpful and demonstrated the procedure to me, which, reassuringly, was exactly how his mum had shown me. Ian also asked the dietitian to give me a call to give advice about care of the tube, and this was another opportunity for me to ask questions.
Now Jonah is a lively little boy who is thriving and is now a normal weight for his age. He loves being at nursery and is very attached to us. I am really proud that we have managed to play such an important part in his development and have met his additional needs.
Now have a go at the activity below.
Activity 5.1 Building confidence
What do you think made a difference in the case study above? Make a few notes in your learning journal.
Discussion
The following quote is Karen’s response to being asked what she thought helped her to successfully take on the task of administering Jonah’s gastrostomy tube feeds.
Firstly, working with his mum was really important, as was working with other health professionals, especially Ian. It was also important for the team to be behind the idea of supporting Jonah and being committed to meeting his additional needs. Most of all, it was important that I appeared confident that we could tube-feed Jonah and that I showed leadership in learning about the tube feeding, because the knowledge I gained helped me to be confident. It was not as scary as I thought it was going to be.
As you can see from this case study, Jonah’s needs were successfully met because of several of Karen’s actions, which included:
- working with and listening carefully to Jonah’s mum
- involving other professionals
- being willing to increase her knowledge and get training about a specific skill
- showing leadership with the nursery team.
It is important to be aware that you don’t need to be a senior staff member to show leadership when you are working with a child with a disability.
Developing knowledge and skills for complex medical needs
There are many pieces of guidance that can help you to increase your knowledge and skills to help you work successfully with children with complex medical needs. There are some sources of information at the end of this section, along with an extension activity that includes videos illustrating the use of tactile books with children who have complex medical needs.
5.3 Working with families, parents and professionals
Working with families of all children is an important part of ELC practice but working with children with complex medical needs requires additional consideration, because these children will require support from other professionals. This section explores some of the issues regarding support for children with complex medical needs by working with their families and other professionals in effective ways.
Working with families
Parenting children with complex medical needs is challenging. They may be feeling a range of emotions about their child’s needs and they may still be coming to terms with the impact that their child’s needs are having on their family.
One of the areas that families of children with complex needs find challenging is that they encounter numerous professionals who are involved in their child’s care.
The National Managed Clinical Network (2016) publishes information for parents and summarises some of the feelings that parents may experience:
Having people in your home can be quite challenging. Parents talk about feeling ‘invaded’ and ‘exposed’. Unlike parents of typically developing children your parenting can feel under regular scrutiny as a range of professionals visit you, often on a weekly basis. Professionals understand that they are essentially guests in your home, but some will be better than others in managing this sensitively.
In Week 4 we learned that one way of supporting children in the transition to nursery is to arrange a home visit. However, for parents of a child with complex medical needs, you may be yet another professional that they need to allow into their home. Therefore, careful consideration needs to be given to how you approach the family to request a home visit.

Working with other professionals
A child with complex needs is likely to have additional support from different professionals, which may include a health visitor, speech and language therapist, physiotherapist, dietitian, and/or social worker. In order to help you, the child’s family and all professionals to work together efficiently, it is important for the care to be coordinated. In Scotland, the Supporting Children’s Learning guidance (2017) requires that a ‘
A Child’s Plan
A Child’s Plan will include everything relevant to the child’s overall health and wellbeing.
The following statement comes from the Supporting Children’s Learning (2017, p. 94) statutory guidance.
A Child’s Plan will be unique to each child but in agreement with the child and parents will usually include and record:
- reasons for the plan
- partners to the plan
- the views of the child or young person and their parents or carers
- a summary of the child or young person's needs
- what is to be done to improve a child or young person's circumstances
- details of action to be taken
- resources to be provided
- timescales for action and for change
- contingency plans
- arrangements for reviewing the plan
- Lead Professional arrangements where they are appropriate
- details of any compulsory measures if required.
A child may have a coordinated support plan too. This refers to the support they need for their learning, which may include a physio plan, feeding plan or communication tools. When children have complex needs this is likely to be included as part of the Child’s Plan.
Child’s Plans will vary according to the format set out by each local authority. They will all cover the key points set out in legislation. Below are some key titles that appear in them.
|
|
In order to coordinate the child’s additional support as laid out in the plan, a Lead Professional will be appointed. In order to assess the effectiveness of the support, child planning meetings are important opportunities for the child, their family and professionals to meet.
Child planning meetings will vary but are likely to be chaired by a health visitor (who may be the
While it can be empowering to lead the care and support for their child, it is important that professionals do not assume that parents will take the lead in this way. Professionals need to empower parents to advocate for and with their child without the burden of arranging meetings, negotiating budgets or checking that documents have been shared.
Child planning meetings are intended to streamline communication and planning, reduce the burden on parents having to repeat information to a range of different professionals, and ensure that the child’s best interests are the priority.
Taking part in a child planning meeting
The contribution that ELC practitioners make to a child planning meeting is an important one, but there can be challenges too. In the next activity Pamela and Liz discuss their experience of child planning meetings for Pamela’s daughter, Eilidh. You’ll hear how difficulties were resolved and how positive relationships were built that benefitted everyone.

Activity 5.2 What makes a good child’s planning meeting?
Listen again to Pamela and Liz, this time discussing planning meetings. Make a note in your learning journal of the key points and compare your list with the one in the discussion.
Transcript: Audio 5.1 Liz and Pamela discussing good planning meetings
Discussion
Pamela and Liz thought that a good planning meeting included
- speaking up about which staff should be at the meeting and making changes
- being able to talk about what does and doesn’t work
- having the child present and involved in the conversation, and ensuring that the child has someone to look after and play with them during the meeting (although it may not always be practical or possible for the child to be present)
- deciding, in partnership with families, which professionals it is most helpful to have at the meeting
- ensuring that the family has met the professionals before the meeting
- ensuring that the communication needs of the family have been considered
- having a welcoming and comfortable meeting space, with refreshments available.
- professionals listening to each other
- finding a time that works for everyone, to enable follow-up conversations and relationship-building.
Perhaps you are involved in child planning meetings. Now that you have reflected on what can help a meeting go well, is there anything you would like to improve?
This section has highlighted some of the key points that will help you to conduct a child planning meeting. The next section looks at play for children with complex medical needs and explores resources that will be helpful.
5.4 Play and resources for children with complex medical needs
Books and stories

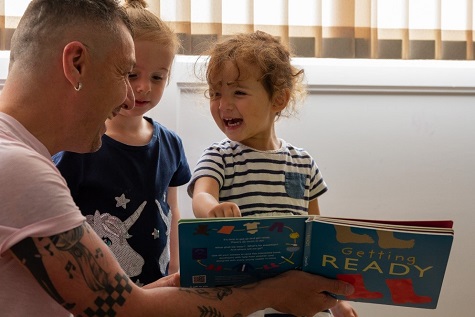
Books are sensory objects. You can touch them, taste them, turn the pages, play peek-a-boo, wear them like a hat or snap them like a crocodile. Many books have sensory elements such as flaps or textures – or even smells!
You can explore the information or stories in books in many ways.
The short films in the link below show sensory books being used in different ways. While you are watching, think about the different ways that books are experienced. If you incorporate sensory experiences and use books in varied ways in your setting as part of your everyday practice, then you’ll be helping all children to understand that books and stories can be experienced in different ways. This will help you create a more inclusive environment that welcomes a child with a disability.
Tactile book videos from Bookbug:
Off to the Beach
Off to the Park
Getting Ready
There is more information on the Bookbug website about ensuring that all children can access the Bookbug Explore pack by using images and recordings for Big Mack switches and GoTalk. If you’ve never heard of either of those before, then it’s time to be the explorer yourself!
Another way to share stories is by using the senses. The simplest or most familiar stories can be made exciting and inviting to all children. Think about how you might experience a story through your senses. If you told the story of the three little pigs, you could make pig noises or use a recording of a pig snort; you could include straw, sticks and some small bricks to touch and share. You could use a balloon pump to huff and puff like a wolf and a bowl of water for him to land in as climbs down the chimney.
Remember: it is very straightforward to create your own story that will be exciting to all children. Experiment! Pressing a big button to make a sound is something that all children love to do.
Activity 5.3 Resources for children with complex medical needs
Sensory activities
Children with complex medical needs may find that sensory activities are especially enjoyable. The movement of sunshine and wind on some special fabric outside can lead to all kinds of songs and peek-a-boo games. These are games and play that can draw all children into a shared game and of course, some children have strong sensory preferences and dislikes.

Make a list of objects and resources that provide a sensory experience and are likely to appeal to all children.
You may like to refer back to the Loose Parts Play Toolkit mentioned in Week 2.
Discussion
What did you come up with? Here are some examples:
|
|
Sharing books
As stated above, books are sensory objects. You could also bring a book to life by using some of the sensory items you listed in the activity above: crunching silver foil or a space blanket makes a sound like crunching on snow, and an ice cube is something cold that the children could touch.
When you work with a child with complex needs, you may be very focused on their needs and your support for them. However, you need to be aware of how you support their relationships with other children. One-to-one support does not mean you need to be the only person interacting with a child. You need to facilitate different ways of ensuring the child you are supporting gets the chance to play, laugh and experience everyday life alongside other children. Sometimes your support needs to be almost invisible.
Summary
This week’s content focused on improving your confidence and knowledge when meeting additional support requirements for children with complex medical needs. By drawing on your previous skills and knowledge you will have been able to identify how you can show leadership when supporting children with complex needs.
Reflection activity
Use your saved learner journal to make notes about this week’s content and consider how it can positively impact your practice to improve the experience for children with ASN. (You can also type into the box below and then copy and paste it into your learner journal.)
After making notes, remember to save your learner journal to use again for the final week of study.
Reflection table for Week 5
| Source of knowledge | |
| Key point | |
| How has this made me think? | |
| So what have I learned? | |
| Next steps: what can I improve or what more do I need to know? | |
| Next steps: what improvements can I make to my practice? |
(Adapted from Appleby and Hanson, 2017)
Next week
In Week 6 you will look at Scottish legislation and policy relating to working with children who require additional support. The content looks at the links between national and local policy, and how policy influences practice.
Now have a go at the Week 5 practice quiz.
Extension activity
Extension activity – Active listening
Understanding your own level of active listening can be a really important step to becoming a good active listener.
Click on the image below and then work through the active listening checklist to evaluate how good you are at listening. Try to be as honest as you can. Your answers are not recorded anywhere but the ‘Reveal discussion’ button will give you feedback based on your answers.
