Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Sunday, 8 March 2026, 7:37 AM
Health Education, Advocacy and Community Mobilisation Module: 3. Factors Affecting Human Health
Study Session 3 Factors Affecting Human Health
Introduction
In this study session, you will learn about some of the key words that are commonly used to describe health and human behaviour. Understanding these will help you in your work with your local community. In this session you will be able to learn about some of the different types of health behaviours and be able to describe their application in your work when you are promoting health and preventing disease.
In this session you will also learn about the Health Field Concept and some of the determinants of health.
Risk factors are those inherited, environmental and behavioural influences which are considered to increase the likelihood of physical or mental health problems in the future. After studying this session you will be able to describe health risk factors and explain their association with human health. You will be able to identify the different health risk reduction models for communicable and non-communicable diseases and describe the role of health education in reducing the risks for such diseases.
Learning Outcomes for Study Session 3
When you have studied this session, you should be able to:
3.1 Define and use correctly all of the key words printed in bold. (SAQ 3.1)
3.2 List some of the different types of health behaviours. (SAQ 3.1)
3.3 Understand the Health Field Concept and the determinants of health. (SAQ 3.2)
3.4 Describe some health risk factors and explain their association with human health. (SAQ 3.3)
3.5 Identify the different health risk reduction Models for communicable diseases and for non-communicable diseases, and describe the role of health education in reducing risks for both types of disease. (SAQ 3.4)
3.1 Health and human behaviour
Behaviour is an action that has a specific frequency, duration and purpose whether conscious or unconscious. It is what we do and how we act.
People stay healthy or become ill often as a result of their own action or behaviour.
Think about the following behaviours. Which ones do you think are health behaviours?
- Reading a newspaper every day
- Singing while you walk
- Using mosquito nets to protect oneself from mosquito bites
- Planting cassava.
Health behaviours are those personal behaviour patterns, actions and habits that people perform in order to stay healthy, in order to restore their health when they get sick and in order to improve their health status. So, in the above list, using a mosquito net is a health behaviour because it reduces the risk of getting malaria.
3.1.1 Types of health behaviours
In this section, you will learn about six different types of health behaviour that people may perform — from the initial stages of preventing diseases up to their actions that may be associated with attempts to rehabilitate themselves after a bout of illness.

Preventive health behaviours: These are actions that healthy people undertake to keep themselves or others healthy and prevent disease or detect illness when there are no symptoms. Examples include handwashing with soap (Figure 3.1), using insecticide treated mosquito nets and exclusive breastfeeding to age six months.
Illness behaviours: These include any activities undertaken by individuals who perceive themselves to be ill. This would include recognition of early symptoms and prompt self referral for treatment. For example a person who feels that they are ill might visit the nearby health centre, while another person might go the church for a cure with holy water (tebel).
Sick-role behaviours: These include any activity undertaken by individuals who consider themselves to be ill, for the purpose of getting well. It includes receiving treatment from medical providers and generally involves a whole range of potentially dependent behaviours. It may lead to some degree of exemption from one’s usual responsibilities. For example a person who feels that he is ill might visit the nearby health centre and receive tablets to be taken home, and might then not do as much work as normal.
Compliance behaviours: This means the person will be following a course of prescribed treatment according to the instructions that the health worker has given them.

Utilisation behaviours: This is the sort of behaviour that is described when people use their health services such as antenatal care, family planning, immunization, taking a sick person for treatment (Figure 3.2), etc.
Rehabilitation behaviours: This is what people need to do after a serious illness to get themselves better and prevent further disability.
Think of one example of each of the health behaviours in the list above.
There are, of course many examples. Below we list a few for each behaviour. As you will have realised from doing this ITQ the range of health behaviours is broad and varied.
Preventive: Eating a balanced diet, exclusive breast feeding for the first six months of life, drying swampy areas in the village to prevent malaria.
Illness: Consulting with the doctor or other health worker, taking a pain killer if you have a headache.
Sick role: Ceasing work, withdrawing from family life temporarily.
Compliance: Washing your hands after going to the latrine as suggested by the health worker; taking your medicine regularly in the case of HIV/AIDS.
Utiliisation: Might include using antenatal care, family planning or immunization services and also the use of services such as HIV testing or voluntary counselling and testing (VCT) services.
Rehabilitation: Practising walking after injuring your leg or practising talking after a stroke.
3.2 The Health Field Concept
The health field is a term used to include all the factors that affect health in addition to the healthcare system. Such a framework was developed and called the Health Field Concept. The health field concept has divided the health field into four elements: human biology, environment, lifestyle and healthcare organisation. These are referred to as the determinants of health.
- Human biology includes all those aspects of health, both physical and mental, which are developed within the human body as a consequence of the basic biology of human beings and the organic make-up of an individual. For example, age is one of the biological determinants of health — because older people are more at risk of developing non-communicable diseases such as cancer.
- Environment includes all those matters related to health which are external to the human body and over which the individual has little or no control. Some examples of matters included in this element include geography, climate, industrial development and the economy. For example, people living in the lowland areas (geographic factors) are more exposed to malaria than people living in the highlands. If the economic environment gets worse then more people will have to live in poverty — and this is very bad for their health.
- Lifestyle is made up of the habits and usual practices of human beings which affect their health and over which they more or less have control. For example people who are not sleeping under insecticide treated bed nets are at more risk of acquiring malaria.
- Health care organisation consists of the arrangement and resources that are used in the provision of healthcare — often referred to as the healthcare system. For example if someone is sick from malaria and there are no health facilities nearby to treat the patient, the patient is more likely to develop a severe complication and may even die.
Match the examples below with the four elements in the Health Field Concept:
- a.Economic conditions
- b.Age
- c.Healthcare system
- d.Insecticide regimes.
1b, 2a, 3d, 4c.
The important thing here is to be clear about the sorts of things that crop up in each element. Here we have only given one example for each element. Before you go on, in your head add another couple of examples to each element. Be sure this concept is familiar to you.
3.3 Risk factors and human health and behaviour
Risk factors are those inherited, environmental and behavioural influences which are known or thought to increase the likelihood of physical or mental health problems. Risk factors increase the probability of illness and of dying early — but do not guarantee that people with the risk factors will suffer any harmful consequences. Risk factors are worked out across a large population of people, so although they are relevant to us all not everyone will be equally affected. For example someone might drive dangerously and never have an accident, or drink too much alcohol and never get any of the illnesses associated with alcohol excess.
Risk factors can be divided into two categories:
- Modifiable (changeable or controllable) risk factors. These are things that individuals can change and control such as their sedentary lifestyle, smoking, drinking alcohol (Figure 3.3), or poor dietary habits.
- Non-modifiable (non-changeable or non-controllable) risk factors. These are factors such as age, sex and inherited genes and are things that individuals cannot change or do not have control over.
These two categories of risk factors may be interrelated and in fact the combined potential for harm from a number of risk factors is greater than the sum of their individual parts. If an old person (old age – as a non-modifiable factor) smokes and drinks (smoking and drinking are modifiable risk factors) to excess as well they are especially likely to become ill with problems related to smoking and drinking.
Over the years, knowledge about the impact of risk factors has continued to grow. In developed countries approximately 40% of deaths are caused by behaviour patterns that could be modified by preventive interventions. In developing countries like Ethiopia, more than 80% of the disease burden and its related morbidity and mortality is due to communicable diseases and malnutrition — which are largely preventable through appropriate preventive measures. Therefore, much of the focus of your health education work as a Health Extension Practitioner needs to be helping individuals identify and control their modifiable risk factors.
Make a list of three modifiable health risk factors and three non-modifiable health risk factors.
Modifiable risk factors are those we can do something about such as smoking and drinking as individuals, and malaria and TB prevention as whole communities.
Non-modifiable risk factors are those we can do nothing about such as age, gender and our genetic inheritance.
3.4 The role of health education in risk reduction
Various models of disease causation and disease transmission have been developed. In this section you will learn about the chain of infection model and the communicable disease model that apply to communicable diseases. Also you will be able to study about the multi-causation disease model for non-communicable diseases. But, no matter which model is applied to explain disease causation and spread, health education has a very important role in reducing the spread and transmission of diseases through helping people reducing their health risks.
3.4.1 The chain of infection model
This model explains the spread of a communicable disease from one host (or person) to another. The basic idea represented in the chain of infection is that individuals can break the chain (reduce the risk) at any point, thus the spread of the disease can be stopped. Figure 3.4 shows the basic links in the chain and Table 3.1 explains the links in detail.
| Component of the model | Definition | Preventive measures |
|---|---|---|
| Communicable disease | Disease caused by an infectious agent | Pasteurization, chlorination, antibiotics, disinfectants, hand washing, etc. |
| Human reservoir | The human being who is harbouring the infectious agent | Isolation, surveillance, treatment with medications, etc. |
| Portal of exit | The body part through which the infectious agent is exiting from the reservoir, for example the mouth or the anus | Utilisation of handkerchiefs, condoms, hair nets, insect repellents, hand washing and latrines, etc. |
| Transmission | The spread of the infectious agent from the reservoir to the host | Isolation, hand washing, mosquito control, sexual abstinence, condom users, etc. |
| Portal of entry | The body part through which the infectious agent will enter the new host, for example the skin after a mosquito bite, the mouth | Condoms, hair nets, insect repellents, hand washing, etc. |
| Establishment of disease in new host (susceptible person) | The host develops signs and symptoms of the new disease | Immunizations, health education, nutrition promotion; sexual abstinence, condom use, etc. |
Now look at Table 3.1 carefully again. There are two sets of components that have some similar preventive measures. As a way of helping yourself become familiar with this chart see if you can spot which these are.
The portal of entry and exit both involve preventive measures such as hand washing, condoms, hair nets and insect repellents, while the human reservoir and transmission measures both involve isolation. Be sure you have a clear picture of the definition and prevention of each element before you continue.
With the application of such information, health education can help to create programmes that are aimed at breaking the chain and reducing the risks of infection in other people. As a Health Extension Practitioner, you will be able educate individuals and your community about these interventions and help to implement many of them.
3.4.2 The communicable disease model
The communicable disease model presents three elements; infectious agent, host and environment, as the minimal requirements for the presence and spread of a communicable disease in a population.
The infectious agent is the element that must be present for the disease to occur and spread. Bacteria, viruses and parasites are examples of infectious agents.
The host is any susceptible organism. Plants, animals or humans can be invaded by the infectious agent and become the host.
The environment includes all other factors that either promote or prohibit disease transmission.
Communicable disease transmission occurs when a susceptible host and an infectious agent exist in an environment that allows disease transmission.
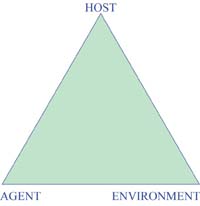
According to the communicable disease model, the role of health education and health promotion in reducing the occurrence and transmission of diseases can be brought about by specific actions.
Think of tuberculosis (TB), malaria and intestinal infections as examples, and then answer the following questions:
- Note one way to reduce the susceptibility of hosts.
- Note one way to destroy infectious agents.
- Note one way to reduce the contact between the host and the agent.
- Note one way to modify the environment so that it is not conducive for disease transmission.
You may have answered with the following examples:
- Good nutrition will build a person’s defences against infection and reduce their risk of developing TB.
- Cooking food properly destroys infectious agents that could cause intestinal infections.
- Wearing a mask or holding your hand in front of your mouth while coughing will reduce the contact between the agent that causes TB, and other human beings. Using a bed net will reduce contact with malaria — carrying mosquitoes (Figure 3.6).
- Drying swampy and marshy areas will make the environment less easy for mosquitoes to breed in and therefore reduce the incidence of malaria.

3.5 Health risk reduction for non-communicable diseases
Both the chain of infection and communicable disease models are helpful in trying to prevent disease caused by an infectious agent. However, these models are not applicable to non-communicable diseases, which include many of the chronic diseases such as heart disease and cancers. Most of these diseases become apparent in people over a period of time and are not caused by a single factor, but by a combination of factors. The concept of ‘caused by many factors’ is often called the multi causation disease model. For example, it is known that heart disease is most likely to be a problem for individuals who are older, who smoke, who do not exercise, who are overweight, who have high blood pressure, who have high blood cholesterol and who have a family history of heart disease.
Note that within the list of factors you have just read there are both modifiable and non-modifiable risk factors. Look at the list again and put an M against the modifiable factors and an NM against the non-modifiable factors.
Individuals who:
- Are older: NM
- Smoke: M
- Do not exercise: M
- Are overweight: M
- Have high blood pressure: M
- Have high cholesterol: M
- Have a family history of heart disease: NM.

According to this model, health education will be useful in risk reduction and disease prevention if you can create programmes that help people control as many of the multi causative risk factors as possible (Figure 3.7).
Summary of Study Session 3
In Study Session 3, you have learned that:
- Behaviour is an action that has a specific frequency, duration and purpose whether conscious or unconscious. It is what we do and how we act. People stay healthy or become ill often as a result of their own actions or behaviour. One such example is using mosquito nets at night to protect oneself from mosquito bites.
- Preventive health behaviours are actions that healthy people undertake to keep themselves or others healthy. Examples include good nutrition and exclusive breastfeeding until the age of six months. Illness behaviours include any activities undertaken by an individual who perceives him or herself to be ill. Compliance behaviours are to do with following a course of prescribed treatment regimes. Utilisation behaviours involve the utilisation of health services such as antenatal care or family planning. Rehabilitation behaviours are the ways that people behave after a serious illness to get themselves better again.
- Determinants of health are the biological, environmental, behavioural, organisational, political and social factors that contribute either positively or negatively to the health status of individuals, groups and communities.
- Risk factors are those inherited, environmental and behavioural influences which are known or thought to increase the likelihood of physical or mental health problems. Risk factors increase the probability of morbidity and premature mortality, but do not guarantee that people with the risk factors will suffer the consequences.
- Modifiable (changeable or controllable) risk factors are things that individuals can change and control — such as sedentary life style, smoking or poor dietary habits. Non-modifiable (non-changeable or non-controllable) risk factors include factors such as age, sex and inherited genes — things that individuals cannot change or do not have control over.
- The chain of infection model is a model used to explain the spread of a communicable disease from one host to another. Individuals can break the chain (reduce the risk) at any point, thus the spread of the disease can be stopped. Health education can help to create programmes that are aimed at breaking the chain and reducing the risks.
- The communicable disease model shows that communicable disease transmission occurs when a susceptible host and an infectious agent exist in an environment suitable for disease transmission. According to the communicable disease model the role of health education and health promotion in reducing the occurrence and transmission of diseases will be by reducing the susceptibility of hosts, destroying infectious agents, reducing the contact between the host and the agent and through modifying the environment so that it is not conducive for disease transmission.
- With regard to the non-communicable disease model, health education activities will be able to provide programmes to help people reduce the risk of disease by controlling as many of their multi-causative risk factors as possible.
Self-Assessment Questions (SAQs) for Study Session 3
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 3.1 (tests Learning Outcomes 3.1 and 3.2)
Now that you are clear about the various health behaviours consider your own community as a whole. Write down some examples from your observations about these behaviours in your community:
- a.Preventive behaviours towards childhood illnesses
- b.Illness behaviours when children get diseases such as measles
- c.Compliance behaviours towards anti-tuberculosis treatment
- d.Utilisation behaviours in relation to antenatal clinics
- e.Rehabilitation behaviour after someone gets a severe injury following a car accident.
Answer
- a.Preventive behaviours towards childhood illnesses might include providing good nutrition for the child, taking the child for immunization and exclusive breastfeeding until six months.
- b.Illness behaviours towards childhood illnesses include taking the child to the health post, possibly taking the child to some traditional healers in the community (although these may be dangerous actions).
- c.Compliance behaviours towards anti-TB treatment include adhering to the instructions given by the health workers as to the frequency and duration of the treatment. In any community, some people with TB may adhere to the treatment while others may not adhere so well.
- d.Utilisation behaviours in relation to antenatal clinics are about the extent to which the service is used regularly by women before their babies are born.
- e.Rehabilitation behaviours may include using crutches or other artificial supports so that injured people can walk and attend to their farming or household activities.
SAQ 3.2 (tests Learning Outcome 3.3)
According to the Health Field Concept, what are the four determinants of health?
Answer
According to the Health Field Concept, the determinants of health include human biology, lifestyles, and the environment and healthcare organisations.
SAQ 3.3 (tests Learning Outcome 3.4)
List the risk factors relating to malaria in your community and note which are modifiable and which ones are non-modifiable.
Answer
Risk factors may include the seasons, the extent of marshy and swampy areas in the community, not using bed nets, age, poor nutritional status, sick people not being treated on time, resistance of the mosquitoes to the insecticides, resistance of the parasite to the drugs available, and so on.
The list of factors we’ve included above includes some factors that individuals may be able to modify by themselves, such as not using bed nets or poor nutritional status. Others are beyond the control of the individual, for example the seasons or the greater vulnerability of babies and very old people to die from malaria if they become infected.
If you cannot answer these questions fully at this stage, you will learn full details of malaria and TB in the Communicable Diseases Module, and heart disease in the Non-Communicable Diseases, Emergency Care and Mental Health Module.
SAQ 3.4 (tests Learning Outcome 3.5)
- a.According to the chain of infection model, what is the role of health education in disease prevention and control? Use the example of malaria in your answer.
- b.According to the communicable disease model, what will be the role of health education in disease prevention and control? Use the example of TB in your answer.
- c.According to the multi-causation disease model, what will be the role of health education in disease prevention and control? Use the example of heart disease in your answer.
Answer
(a) Health education has many roles in the prevention and control of malaria. Health Extension Practitioners have several responsibilities in the prevention and control of malaria based on the chain of infection model. Below are some examples in response to each component of the model:
| Component of the model | Examples of preventive measures | Role of health education |
|---|---|---|
| Pathogen | Taking effective anti-malarial drugs | Educating people to take treatment |
| Human reservoir | Reducing the infective period of the disease in each individual | Encouraging early diagnosis and treatment of sick people |
| Portal of exit | Applying mosquito repellents over the skin | Promoting and encouraging people to apply repellents |
| Transmission | Spraying insecticides inside households | Advising families to allow insecticide spraying of their houses |
| Portal of entry | Sleeping under insecticide-treated bed nets | Persuading families to utilise bed nets correctly |
| Establishment of disease in new host | Once the disease occurred, promoting early recovery | Encouraging good nutrition and adherence to treatment |
(b) According to the communicable disease model, the role of health education in reducing the occurrence and transmission of tuberculosis is summarised as follows:
| Component of the model | Role of health education | Advice to community members |
|---|---|---|
| Host | Providing health education in order to reducing the susceptibility of hosts through good nutrition | Please try to get good nutrition based on what is available at home |
| Agent | Facilitating the destroying of the pathogenic agents that causes tuberculosis | If you are a TB patient on treatment, please take your medication regularly |
| Host–agent interaction | Educating people on how to reducing their possible contact with the agent | Please cover your mouth while coughing |
| Environment | Persuading people to ventilate their households so that the environment in the houses is not conducive for the transmission of TB | Please ventilate your houses as much as possible |
(c) According to the multicausation disease model, heart disease is most likely to manifest itself in individuals who are older, who smoke, who do not exercise, who are overweight, who have high blood pressure, who have high cholesterol and who have family history of heart disease.
If you look at the list of risk factors, some of them are modifiable while the others are non-modifiable ones. Hence, your role will be to identify the modifiable risk factors and educate people on what they should do to modify those behaviours in a fashion that will be favourable for their health. For example, for those individuals who smoke you need to advise them to quit smoking and for those who do not exercise and who are overweight, you need to persuade them to do more exercise.
