Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Tuesday, 10 March 2026, 8:28 AM
Health Education, Advocacy and Community Mobilisation Module: 4. Human Behaviour and Health: 1
Study Session 4 Human Behaviour and Health: 1
Introduction
In this study session you will be able to learn about the various levels of disease prevention activities. You will also learn about the role of health education in preventing diseases and promoting health at the various levels of disease prevention.
The study session will help you define your role as a health educator and consider the impact of your health education work in maximising the gains from preventive measures at each level of disease prevention. It will also help you learn about the various phases of assessment to be conducted and how you can make assessments within your community.
Three broad categories of determinants of human behaviour will be discussed in this study session and you will have an opportunity to learn about the influence of these factors in determining human behaviour.
Learning Outcomes for Study Session 4
When you have studied this session, you should be able to:
4.1 Define and use correctly all of the key words printed in bold. (SAQs 4.1, 4.2 and 4.3)
4.2 List the levels of disease prevention. (SAQ 4.1)
4.3 Define the impact of health education and define your role as a health worker in maximising the effects of the various preventive measures at each level. (SAQ 4.1)
4.4 Explain the various phases of assessment to be conducted before identifying the determinants of human behaviour. (SAQ 4.2)
4.5 Describe predisposing factors and explain their influence in determining human behaviour. (SAQs 4.2 and 4.3)
4.6 Describe enabling factors and explain their influence in determining human behaviour. (SAQ 4.3)
4.7 Describe reinforcing factors and explain their influence in determining human behaviour. (SAQ 4.3)
4.1 Levels of disease prevention
Prevention, as it relates to health, is really about avoiding disease before it starts. It has been defined as the plans for, and the measures taken, to prevent the onset of a disease or other health problem before the occurrence of the undesirable health event. There are three distinct levels of prevention, which you already met briefly in Study Session 2.
4.1.1 Primary prevention
Primary prevention — those preventive measures that prevent the onset of illness or injury before the disease process begins. Examples include immunization (Figure 4.1) and taking regular exercise.

4.1.2 Secondary prevention
Secondary prevention — those preventive measures that lead to early diagnosis and prompt treatment of a disease, illness or injury to prevent more severe problems developing. Here health educators such as Health Extension Practitioners can help individuals acquire the skills of detecting diseases in their early stages. Examples include screening for high blood pressure and breast self-examination; you will learn about both of these in the Module on Non-Communicable Diseases, Emergency Care and Mental Health.
4.1.3 Tertiary prevention
Tertiary prevention — those preventive measures aimed at rehabilitation following significant illness. At this level Health Extension Practitioners can work to retrain, re-educate and rehabilitate people who have already developed an impairment or disability.
Read the list of the three levels of prevention again. Think about your experience of health education, whether as an educator or recipient of health education. How do you think health education can help with the prevention of disease? Do you think it will operate at all these levels? Note an example of possible health education interventions at each level where you think health education can be applied.
Health Education can be applied at all three levels of disease prevention and can be of great help in maximising the gains from preventive behaviour. For example at the primary prevention level — you could educate people to practice some of the preventive behaviours, such as having a balanced diet so that they can protect themselves from developing diseases in the future. At the secondary level, you could educate people to visit their local health centre when they experience symptoms of illness, such as fever, so they can get early treatment for their health problems. At the tertiary level, you could educate people to take their medication appropriately and find ways of working towards rehabilitation from significant illness or disability.
4.2 Determinants of human behaviour
Before identifying the various determinants of human behaviour, you should consider the following four types of assessment: social diagnosis, epidemiological diagnosis, educational diagnosis, and environmental and behavioural diagnosis. Below is a brief description of each of these phases of assessment.
4.2.1 Social diagnosis
The focus of social diagnosis is to identify and evaluate the social problems which impact on the quality of life within your population. Doing a ‘social diagnosis’ will help you to gain an understanding of the social problems which affect the quality of life of people in your community, and how local people see those problems. This understanding is followed by the establishment of a link between the social problems and specific health problems that will become the focus of your health education activities.
Research methods are taught in the Module on Health Management, Ethics and Research.
Methods used for social diagnosis may be one or more of the following: community forums, focus groups, surveys and interviews.
An example of a social diagnosis would be that in a community the quality of life of the people may be very low as a result of poverty, malnutrition and the poor quality of drinking water.
4.2.2 Epidemiological diagnosis
Epidemiological diagnosis will help you to determine the specific health issues that affect the people in your community. The focus of this phase is to identify both the health problems and the non-health factors which are associated with a poor quality of life. Describing these health problems can help establish a relationship between health problems and the quality of life. It can also lead to the setting of priorities which will guide your health education programmes and show you how to best use your resources.
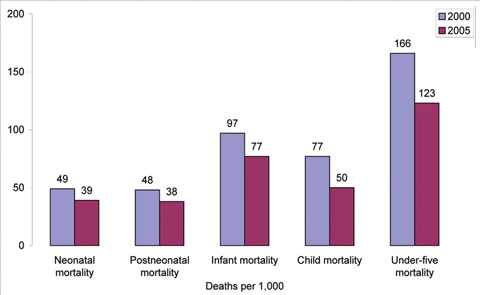
Examples of epidemiological data include mortality and morbidity statistics (see Figure 4.2) and the prevalence and incidence of diseases.
An example would be that in your community the specific health problems that have resulted in poor quality of life. These may be malaria, HIV/AIDS, TB, malnutrition and others. At this phase you will identify which ones are the most important ones.
4.2.3 Educational diagnosis
This phase of assessment pinpoints the factors that must be changed to initiate and maintain behavioural change. Educational diagnosis looks at the specific features that hinder or promote behaviour related to the health issues that are important in your community. An example would be to identify why people are behaving in a way that is dangerous to their life? As you will see later in the study session there are a number of ways of examining these sorts of questions as they relate to predisposing, enabling and reinforcing factors.
4.2.4 Environmental and behavioural diagnosis
Environmental diagnosis is a parallel analysis of factors in the social and physical environment that could be linked to health problems.
Behavioural diagnosis is the analysis of behavioural links to the health problems that are identified in the epidemiological or social diagnosis.
This phase focuses on the systematic identification of health practices or behaviours which cause health problems in your community. If you take the example of HIV/AIDS, once you reach this stage your focus will be to examine why people in your community are highly affected by HIV/AIDS. Is it because of their behaviours — or is it due to other environmental factors such as lack of HIV prevention and counselling services? At this stage you need to be able to identify the factors — and as in many societies the most important factor responsible for higher level of HIV/AIDS in your community may be high-risk sexual behaviours.
Read again the list of different diagnoses that precede and underpin preventive heath education work. Of these various processes which one do you think you are most likely to need to consult with other health colleagues over?
As a health worker you are likely to undertake social diagnosis, behavioural diagnosis and education diagnosis yourself. You will also collect some statistical data yourself, from your own community. But you are likely to depend at least as much if not more on statistics from other colleagues. The reason for this is that epidemiological data has to be collected from large numbers of people in order to be able to see trends, and looking at a small sample from your community may not enable to you understand what happens at the level of a whole population.
4.3 Factors affecting behaviour
Three factors affecting behaviour can be identified:
- Predisposing factors
- Enabling factors
- Reinforcing factors.
4.3.1 Predisposing factors
Predisposing factors are those characteristics of a person or population that motivate behaviour before the occurrence of that behaviour. Peoples’ knowledge, beliefs, values and attitudes are predisposing factors and always affect the way they behave. Predisposing factors are motivational factors subject to change through direct communication or education. All of these can be seen as targets for change in health promotion or other public health interventions. We will look at each of them in turn.
Knowledge
Knowledge is usually needed but is not enough on its own for individuals or groups to change their behaviour. At least some awareness of health needs and behaviour that would address that need is required. Usually, however, for behaviour change some additional motivation is required. For example, even if a mother knows in general about using oral rehydration salts (ORS) when her child is dehydrated due to diarrhoea, she may need a reinforcing message from you before she will actually use them.
Beliefs
Beliefs are convictions that something is real or true. Statements of belief about health include such negative comments as, ‘I don’t believe that exercising daily will improve my health’. More positive health beliefs might include statements such as, ‘If I use an insecticide treated bed net at night I will probably not get malaria.’
Often a potent motivator related to beliefs is fear. Fear combines an element of belief with an element of anxiety. The anxiety results from beliefs about the severity of the health threat and one’s susceptibility to it, along with a feeling of hopelessness or helplessness to do anything about the threat.
Values
Values are the moral and ethical reasons or justifications that people use to justify their actions. They determine whether people consider various health-related behaviours to be right or wrong. Similar values tend to be held by people who share generation, geography, history or ethnicity. Values are considered to be more entrenched and thus less open to change than beliefs or attitudes. Of interest is the fact that people often hold conflicting values. For example, a teenage male may place a high value on living a long life; at the same time, he may engage in risky behaviours such as chewing khat and drinking alcohol. Health promotion programmes often seek to help people see the conflicts in their values, or between their values and their behaviour.
Attitudes
Attitudes are relatively constant feelings directed toward something or someone that contains a judgment about whether that something or someone is good or bad. Attitudes can always be categorised as positive or negative. For example, a woman may feel that using contraception is unacceptable. Attitudes differ from beliefs in that they always include some evaluation of the person, object or action.
Self-efficacy
The most important predisposing factor for self-regulating one’s behaviour is seen to be self-efficacy, that is the person’s perception of how successful he or she can be in performing a particular behaviour. Self-efficacy is learning why particular behaviours are harmful or helpful. It includes learning how to modify one’s behaviour, which is a prerequisite for being able to undertake or maintain behaviours that are good for your health. Health education and behavioural change programmes help a person to bring the performance of a particular behaviour under his or her self-control.
Make a list of some health beliefs that you think that some people in your own community have which affect the way they behave — in other words beliefs which pre-dispose them to have certain health behaviours.
Of course beliefs can cover a huge range. They could equally be ‘I don’t believe that smoking harms my health’ through to ‘I do believe that smoking harms my health’. The same may be true of people’s beliefs about exercise, alcohol and so on. The important thing is that beliefs don’t always coincide with facts. For example the evidence is that smoking does harm health. But many people believe that it doesn’t affect their health.
4.3.2 Enabling factors
Enabling factors are factors that make it possible (or easier) for individuals or populations to change their behaviour or their environment. Enabling factors include resources (Figure 4.3), conditions of living, social support and the development of certain skills.

Among the factors that influence use of health services are two categories of enabling resources: community-enabling resources (health personnel and facilities must be available), and personal or family-enabling resources (people must know how to access and use the services and have the means to get to them).
Enabling factors refer to characteristics of the environment that facilitate or impede healthy behaviour. They also include the skills and resources required to attain a behaviour. For example enabling factors for a mother to give oral rehydration salts to her child with diarrhoea include having time, a suitable container and the salt solution itself.
Skills
A person or population may need to employ a number of skills to carry out all the tasks involved in changing their behaviour. For some positive health behaviours it might be necessary to learn new skills. For example if a breast feeding mother is not well trained on positioning and attachment of her baby she may have difficulty in properly breastfeeding her child. Similarly, if the mother is not well trained at a later stage on the preparation of complementary feeding, the child may not get the nutrition they require.
Healthcare resources
A number of healthcare resources may also need to be in place if an individual or population is to make and sustain a particular health-related behaviour change. The availability, accessibility and affordability of these resources may either enable or hinder undertaking a particular behaviour. For example, in a given health post the lack of availability of the family planning method of choice for a mother may discourage her from utilisation of the service in the future.
Changing behaviour may also be easier if other aspects of one’s environment are supportive of that change. For example policy initiatives or even laws might be in place that create a positive atmosphere for change.
From your experience as an educator or receiver of health education make a list of some of the enabling skills and enabling resources you have seen or experienced that support health education.
Enabling factors make it possible (or easier) for individuals or populations to change their health-related behaviour. Enabling skills, of course, include making sure people know how to do things. We used the example of breast feeding but knowing about how to identify healthy food would be another, or how to recognise a dehydrated child. In regard to resources we mentioned family planning facilities, but there are many others, such as facilities for the prevention of malaria, development of hygienic latrines (Figure 4.4) and so on.

4.3.3 Reinforcing Factors
Reinforcing factors are the positive or negative influences or feedback from others that encourage or discourage health-related behaviour change. The most important reinforcing factors are usually related to social influences from family, peers, teachers or employers.
Social influence
Social influence is the positive or negative influence from those influential people around us that might encourage or discourage us from performing certain health-related behaviours. For example a mother who is planning to start family planning (FP) might be influenced by negative attitudes from her peer group and think, ‘Most of my friends do not use FP methods and I may lose friends in the neighbourhood if I use the methods’. She might also be influenced by her family: ‘My family members do not all support the idea of using FP methods, especially my husband and my mother-in-law. They would really be mad at me if I use FP’. She may also be aware that her community society or culture generally may not be supportive: ‘Everyone in our community is against FP and it is seen as a sin in our society’.
An individual’s behaviour and health-related decision making — such as choice of diet, condom use, quitting smoking and drinking, etc. — might very well be dependent on the social networks and organisations they relate to. Peer group, family, school (Figure 4.5) and workplace are all important influences when people make up their minds about their individual health-related behaviour.

Choose either smoking or alcohol use among young men and think about some of the reinforcing factors, or reinforcing people, that might encourage them to stay smoking or give up smoking or alcohol.
Reinforcing factors are the positive or negative influences or feedback from others that encourage or discourage the behaviour change. The most important reinforcers in a given community include family, peers, teachers and employers. In the case of young men, their own peer group may be the strongest reinforcer to stay smoking or using alcohol. They may think they look grown up, or that others will think they look childish if they don’t smoke or drink a lot. But perhaps employers may say that it is not professional to smoke or teachers may say it is childish to smoke.
Summary of Study Session 4
In Study Session 4 you have learned that:
- Primary prevention includes those preventive measures that come before the onset of illness or injury and before the disease process begins. Examples include immunization and taking regular exercise to prevent health problems developing in the future.
- Secondary prevention includes those preventive measures that lead to early diagnosis and prompt treatment of a disease, illness or injury. This should limit disability, impairment or dependency and prevent more severe health problems developing in the future.
- Tertiary prevention includes those preventive measures aimed at rehabilitation following significant illness. At this level health educators work to retrain, re-educate and rehabilitate the individual who has already had an impairment or disability.
- Health education can be applied at all levels of prevention. Health educators can be of great help in bringing about gains from preventive interventions.
- Before identifying the various determinants of human behaviour, the following assessments need to be done: social diagnosis, epidemiological diagnosis, educational diagnosis, and environmental and behavioural diagnosis.
- Three kinds of behavioural determinants have been identified: predisposing factors, enabling factors and reinforcing factors.
- Predisposing factors are any characteristics of a person or population that motivates behaviour prior to the occurrence of that behaviour, for example their knowledge, beliefs, values and attitudes, and their level of self-efficacy.
- Enabling factors are characteristics of the environment that facilitate action and any skills or resources that are required to carry out a specific health behaviour, for example accessibility, availability or specific skills.
- Reinforcing factors are rewards or punishments following, or anticipated as a consequence of, a health-related behaviour. They serve to strengthen the motivation for behaviour. These may include positive or negative influences from influential people such as the person’s family, peers or significant people in the community.
Self-Assessment Questions (SAQs) for Study Session 4
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 4.1 (tests Learning Outcomes 4.1, 4.2 and 4.3)
Suppose that malaria is one of the most important health problems in your community. What would be the most important preventive measures to be applied at each level of disease prevention? What would be the role of health education in maximising the impacts of the preventive measures?
- a.Primary prevention?
- b.Secondary prevention?
- c.Tertiary prevention?
You will find it helpful to think about what goes on in your own community and any health education you have received yourself, as well as knowledge you may have as a health worker.
Answer
- a.Primary prevention includes those preventive measures that prevent the onset of illness or injury before the disease process begins. Some of the actions to be taken before a person gets malaria include utilisation of bed nets, allowing households to be sprayed with insecticides, applying insect repellents, etc. The role of health education will be to educate people to undertake the preventive actions.
- b.Secondary prevention includes those preventive measures that lead to early diagnosis and prompt treatment of a disease, illness or injury to limit disability, impairment or dependency, and prevent more severe problems developing. Examples for secondary prevention of malaria include enabling people to recognise the symptoms of malaria and to get early diagnosis and treatment. Here health education can help individuals acquire skills of detecting malaria in its early stages and in persuading people to get treatment quickly.
- c.Tertiary prevention includes those preventive measures aimed at rehabilitation following significant illness. In regard to malaria, severe and complicated malaria can sometimes cause severe physical and mental impairments and there is a need to rehabilitate and restore health to the damaged body parts. At this level health education would help in retraining, re-educating and rehabilitating the individual who has already incurred disability or impairment.
SAQ 4.2 (tests Learning Outcomes 4.1, 4.4 and 4.5)
Before identifying the most important determinants of a given human behaviour, there should be some kind of assessment conducted. In this study session four forms have been discussed.
- a.Social diagnosis
- b.Epidemiological diagnosis
- c.Behavioural and environmental diagnosis
- d.Educational diagnosis.
Which of these types of diagnosis is linked with the following methods? Match the letters with the numbers:
- Comparisons of individual behaviours with factors outside individual control
- Focus groups
- Analysis of predisposing, enabling and reinforcing factors
- Statistical analysis.
Answer
1c, 2a, 3d, 4b.
You will have realised that all of these methods fit together. You need to know what people think in your community as well as understand any available statistical data. You also need to understand various local beliefs and environmental factors.
SAQ 4.3 (tests Learning Outcomes 4.1, 4.5, 4.6 and 4.7)
Assume that after conducting the epidemiological assessment you have identified TB as one of the priority health problems in your community. What do you think could be contributing to the transmission of TB in your community? Give your answer under these broad categories of factors.
- a.Predisposing factors
- b.Enabling factors
- c.Reinforcing factors.
Answer
Factors that could be contributing for the transmission of TB in your community could include the following:
- a.Predisposing factors might include lack of knowledge about modes of transmission, wrong beliefs about its treatment or even bad attitudes towards the management of TB patients at the nearby health centre, etc.
- b.Enabling factors include accessibility of TB diagnosis facilities and the availability of free TB treatment in the nearby health centre, etc.
- c.Reinforcing factors include influences from influential people, for example if the family of a TB patient influence him to go to a traditional healer. If he or she does not get cured from the disease promptly they may be responsible for a prolonged period of transmitting the infection throughout the community.