3 The importance of a One Health approach to tackling AMR
AMR is a wicked problem
AMR, together with climate change, is considered to be one of the world’s ‘wicked problems’. Wicked problems are threats to human existence that are very complex to understand, solve or manage. Addressing wicked problems (van Woezik et al., 2016) depends on:
- compromises between competing values
- a multidisciplinary approach
- collaboration between those parties involved .
Wicked problems do not have easy solutions.
A complex interaction of factors drives the emergence and spread of AMR
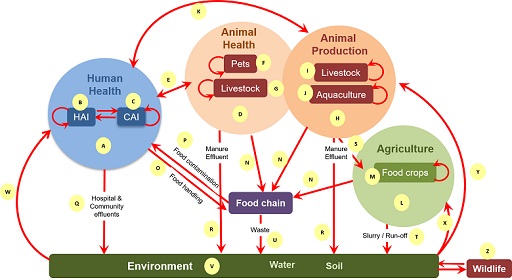
Interaction of an extremely complex mix of factors drives the emergence and spread of AMR within and between populations and their environments, as shown in Figure 1. The figure illustrates the main drivers for emergence of AMR in the different sectors, as well as the transmission pathways within and between sectors.
AMU in humans, animals and plants drives the emergence of resistance within bacterial populations carried by individuals within these populations. Once AMR has emerged it can spread due to poor hygiene, poor waste management or inadequate farm
AMR spread through transmission of resistant bacteria and resistance genes
Bacteria can become resistant to antimicrobials through mutations or through the transmission of
Movement of these elements between bacteria in the host and/or in the environment result in previously non-resistant bacteria becoming resistant. Plasmids are a type of mobile genetic element consisting of circles of DNA that may carry several ARGs. (You were introduced to ARGs and other mobile genetic elements in the Introducing antimicrobial resistance module.) Spread of AMR can therefore be via transmission of the resistant bacteria themselves, or transmission of resistant genes that cause previously susceptible strains to become resistant.
Activity 2: Looking at the complex mix of factors associated with AMR in all sectors
To help understand this complex mix of factors shown in Figure 1, an explanation associated with each letter in the figure is available as a separate PDF file [Tip: hold Ctrl and click a link to open it in a new tab. (Hide tip)] .
Now spend some time exploring Figure 1.
The role of antimicrobial residues in AMR.
Another contributor to AMR are
- excreted by animals and people to whom antimicrobials have been administered and enter rivers from wastewater treatment plants or farm effluent
- present in animal food products if withdrawal periods for antimicrobials used in animals are not adhered to
- enter waterways from pharmaceutical industry waste associated with the manufacturing of antimicrobials.
Antimicrobial residues may contribute to the emergence of AMR in bacteria carried by host populations other than those in which they were initially used. For example, people may consume antimicrobial residues in food derived from treated animals if withdrawal periods are not adhered to, or in water that contains antimicrobial residues from a range of sources (human, agricultural, animal). Exposure to low levels of antimicrobial residues in this way provides a selective pressure that can result in the development of resistance.
In addition, low levels of antimicrobial residues in the environment contribute to the emergence of AMR in naturally occurring environmental bacteria, making the environment a potential reservoir of ARB and ARGs.
AMR management requires a collective effort from all sectors
The management of AMR therefore requires a collective effort from people working with humans, animals, agriculture and the environment to effectively address it.
Activity 3: Reflecting on the complex mix of factors associated with AMR in all sectors
Now that you have explored Figure 1, use the space below to reflect on your own professional experience with AMR. You may find it helpful to refer to Figure 1 and its supplementary PDF file for ideas when you consider sectors you are less familiar with.
- Which sector are you working in? (For example, is it human health, pet animal health, livestock health, aquaculture, wildlife health, plant health, food quality, environmental management or something else?)
- Give an example of an important bacterial AMR problem in the sector that you work in.
- What do you think led to the emergence of this bacterial AMR problem? How is it spreading?
- Can you give an example of an important bacterial AMR problem in another sector?
- Can you describe how AMR in the sector you work in contributes to AMR in populations in another sector?
- Can you describe how AMR in populations in another sector contributes to AMR in populations in the sector you work in?
2 Misconceptions about a One Health approach to AMR