Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Thursday, 20 November 2025, 12:50 AM
Health Management, Ethics and Research Module: 1. Health Services in Ethiopia
Study Session 1 Health Services in Ethiopia
Introduction
In this first study session of the Health Management, Ethics and Research Module you will be able to learn about the current healthcare delivery system within Ethiopia, the historical development of Primary Health Care (PHC) and its application to the Ethiopian situation. This will help you become aware of your place as a healthworker within the Ethiopian Health Service which is currently going through rapid change and development. You will also learn about the overall concepts of Primary Health Care (PHC) and the implementation of the Ethiopian Health Extension Programme, and find out about some of the successes that the country has achieved in improving the health service and the health of its communities.
Ethiopia is committed to working towards the Millennium Development Goals (MDG) and this study session will include some information about the way that the MDG health-related goals are being focused on.
Later in this Module you will be able to learn about the concepts and principles of leadership and management and their application for Health Extension Practitioners as part of their work in rural communities. You will also have an opportunity to study basic healthcare ethics as well as some simple research methods that will be useful in your work.
Learning Outcomes for Study Session 1
When you have studied this session, you should be able to:
1.1 Define and use correctly all of the key words printed in bold. (SAQ 1.1)
1.2 Describe the principles of Primary Health Care that Ethiopia has implemented to date in order to improve the health status of its people. (SAQ 1.2)
1.3 Describe the major components of the Health Service Extension Programme that are relevant to your practice in rural communities. (SAQ 1.3)
1.4 Describe the role that you as a Health Extension Practitioner have in a case study presented to you. (SAQ 1.4)
1.1 Historical development of Ethiopian Health Services
Although you are currently studying this course in comparatively modern times it is important for you to understand the way that the Health Service you will be working in has developed over previous years. This section will also help you understand how recent changes in health policy have helped the development of Primary Health Care in rural areas. Ethiopia is a country with 85% of its population living in rural areas. Between 70% and 80% of the diseases that affect its population are preventable by using simple methods. Despite this, Ethiopia previously had a health policy that focused on curative and urban-centred health services until the Government of the Federal Democratic Republic of Ethiopia launched its new health policy in 1993.
The new health policy gives much more emphasis on prevention and the health promotion components of healthcare that should be able to resolve most of the health problems of the population. The main features of this policy include a focus on decentralisation, expanding the PHC system, and encouraging partnerships as well as the participation of the whole community in health activities. The strategy of the policy has been to expand healthcare delivery at the grass roots level through the implementation of the Health Service Extension Programme (HSEP). The primary aim of the HSEP approach is to bring health service delivery to the rural community at family level where such a big percentage of the total population lives.
1.2 Organisation of health service delivery
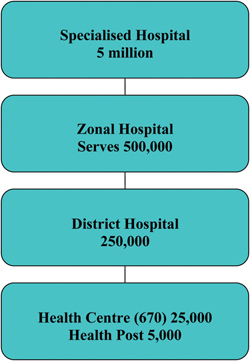
In this section you will learn about the current organisational structure of the healthcare system. The healthcare service has always consisted of a mixture of public, private and nongovernmental healthcare sectors. However, for this session you will mainly focus on the public sector organisational structure. In the mid-1990s, prior to the implementation of Health Sector Development Programme I (HSDP I), the public healthcare system was structured into a six-tier system. Currently, it is a four-tier healthcare system (Figure 1.1), which is organised into Primary Health Care Units (PHCUs), District Hospitals, General Hospitals and Specialised Hospitals. The PHCU is a Health Centre surrounded usually by five satellite Health Posts. Each Health Post serves approximately 5,000 people and the five together total 25,000 people who are looked after by each Health Centre.
At which level do Health Extension Workers and Health Extension Practitioners work?
Health Extension Workers and Health Extension Practitioners work in Health Posts, which are in the fourth tier of the Health Service.
1.3 Concepts of Primary Health Care
The term ‘Primary Health Care’ (PHC) is the name given to the essential healthcare that is universally accessible to individuals and is acceptable to them at a cost that the country and community can afford. Often, as in Ethiopia, this level of healthcare is free for people living in rural areas. Primary Health Care gained the world’s attention after the 1978 International Conference on PHC held at Alma Ata in the USSR (now called Almaty in the country that has become Kazakhstan). Since then many countries have started to follow the approach of PHC to reach rural communities where most of the health problems exist. PHC focuses on disease prevention and health promotion. It is the type of healthcare delivery sometimes described as ‘by the people, of the people and for the people.’ It involves the community in the whole process of healthcare delivery and encourages them to maintain their own health.
The role of the Health Extension Workers and Practitioners is to work with the community and help them acquire the knowledge and skills that enables them to ensure their own health. In the following sections you will study the principles of PHC that will help you to understand its impact on improving health throughout Ethiopia (Figure 1.2).

How would you define Primary Health Care? For whom is it available?
PHC is the lowest tier of the health service. It is where most health services are delivered at village level. Health Extension Workers and Practitioners work at this level. It is available to every member of the community.
1.3.1 Principles of Primary Health Care
The Primary Health Care policy has five principles that have been designed to work together and be implemented simultaneously to bring about a better health outcome for the entire population (Box 1.1). The first principle is accessibility which means universally available healthcare delivery regardless of geographic location. The second principle is public participation which encourages the community to participate in making decisions about their own health, identifying their own health needs and finding solutions to their health problems. The third principle of health promotion involves health education on subjects such as maternal and child health, immunization, nutrition, sanitation and control of endemic disease.
The fourth principle, appropriate technology, emphasises those technologies that are scientifically sound, cost-effective and feasible to be introduced into the community. The fifth principle, inter-sectoral collaboration, emphasises integrated work with other sectors, such as the Ministry of Agriculture and the Ministries of Education, Housing and Water Resources.
Box 1.1 Principles of Primary Health Care (PHC)
- Accessibility (equal distribution): this is the first and most important key to PHC. Healthcare services must be equally shared by all the people of the community irrespective of their race, creed or economic status. This concept helps to shift the accessibility of healthcare from the cities to the rural areas where the most needy and vulnerable groups of the population live.
- Community participation: this includes meaningful involvement of the community in planning, implementing and maintaining their health services. Through the involvement of the community, maximum utilisation of local resources, such as manpower, money and materials, can be utilised to fulfill the goals of PHC.
- Health promotion: involves all the important issues of health education, nutrition, sanitation, maternal and child health, and prevention and control of endemic diseases. Through health promotion individuals and families build an understanding of the determinants of health and develop skills to improve and maintain their health and wellbeing.
- Appropriate technology: technology that is scientifically sound, adaptable to local needs, and acceptable to those who apply it and for whom it is used.
- Inter-sectoral collaboration: to be able to improve the health of local people the PHC programme needs not only the health sector, but also the involvement of other sectors, like agriculture, education and housing.
Which of the five principles of PHC in Box 1.1 is the most important?
None of them is more important than any of the others. They all work together to make a comprehensive and effective policy.
1.3.2 Elements of Primary Health Care
In this section you will learn about the elements or functions of PHC (Box 1.2). These are the essential health services designed to be provided to every community.
Box 1.2 Elements of Primary Health Care
- Education on health problems and how to prevent and control them.
- Development of effective food supply and proper nutrition.
- Maternal and child healthcare, including family planning.
- Adequate and safe water supply and basic sanitation.
- Immunization against major infectious diseases.
- Local endemic diseases control.
- Appropriate treatment of common diseases and injuries.
- Provision of essential basic medication.
Look closely at Box 1.2. Although you haven’t yet studied the roles and responsibilities of Health Extension Practitioners, do you know which of these elements or functions of PHC are your responsibility?
All of these elements are included in the work of Health Extension Practitioners. Of course, some of these functions form a bigger part of your work than others. Remember also that Health Extension Practitioners will get help from other healthworkers and people in their communities.
1.4 Primary Health Care in Ethiopia
Ethiopia is one of the countries in the world which has adopted PHC as a national strategy since 1976. This strategy focuses on fair access to health services by all people throughout the country, with special emphasis on prevention and the control of common diseases, self-reliance and community participation. Since this time the concept of Health Posts (Figure 1.3) and the development of rural health services has been further developed. The government of that time started to construct Health Posts, train Traditional Birth Attendants (TBA) and Community Health Agents (CHA), and assign them to Health Posts. However, this was not sustained due to factors such as insufficient managerial support, lack of in-service training, lack of remuneration and mainly due to centralised health service management and the shift to vertical health programmes.

Vertical health programmes are centralised, non-integrated and disease-specific health programmes. They are designed to tackle single diseases, such as malaria. Although vertical programmes used to be popular, it is now widely thought that they are not very effective and may even undermine the rest of the health services by using too many resources. In late 1997, the Federal Ministry of Health in Ethiopia started to decentralise the health delivery system from Regional to woreda and kebele level, while still maintaining the vertical health programme approach. This approach has not brought the required health outcomes. A new initiative, the Health Service Extension Programme (HSEP), was therefore launched in 2003 together with the Health Sector Development Programme II (HSDP II). This new initiative will be discussed in detail in the next section of this study session.
1.5 Health Service Extension Programme
The Health Service Extension Programme, (HSEP) is an innovative, community-based programme that was first introduced in Ethiopia in 2003. This programme was launched after realising that the basic health services were not reaching the majority of the population. The objective of HSEP is to improve equitable access to mainly preventive health services through community (kebele) based services. These services all have a strong focus on health promotion and preventive health activities, as well as increased community health involvement. The principle behind this programme is to transfer ownership and the responsibility of maintaining health to individual households. This programme has required a sustained political commitment from the government and continued investment that has led to the construction of over 14,000 Health Posts and the training of 30,000 female Health Extension Workers (two for each Health Post) and their deployment in each village (Figure 1.4).

1.5.1 Components of Health Service Extension Programmes
The HSEP is an approach that brings healthcare down to the household level. It has been designed to provide a number of health packages which are categorised under four main topics: Disease Prevention, Family Health Service, Hygiene and Environmental Sanitation, and Health Education and Communication. These packages (Box 1.3) have been developed to tackle the main health problems of the country, such as TB, HIV/AIDS, malaria, and maternal and child health, in order to be able to achieve the Millennium Development Goals which the country aspires to achieve by the year 2015 (the year 2008 in the Ethiopian calendar).
Box 1.3 Health Service Packages for the Health Service Extension Programme
- Disease Prevention and Control. Under this component the most dominant communicable diseases are addressed.
- a.TB, HIV/AIDS and other STI prevention and control.
- b.Malaria prevention and control.
- c.First aid and emergency measures.
- Family Health Service.
- a.Maternal and child health.
- b.Family planning.
- c.Immunization.
- d.Adolescent reproductive health.
- e.Nutrition.
- Hygiene and Environmental Sanitation.
- a.Excreta disposal.
- b.Solid and liquid waste disposal.
- c.Water supply and safety measures.
- d.Food hygiene and safety measures.
- e.Healthy home environment.
- f.Control of insects and rodents.
- g.Personal hygiene.
- Health Education and Communication. This is part of all the packages.
Have a look at the packages that are part of the HSEP and which are set out in Box 1.3. If you are a Health Extension Practitioner working in a rural area, on which of these packages do you think you should concentrate most of your time and resources?
The whole idea of HSEP is that all these packages are of importance. In any particular area the balance of resources that are put into different packages will be slightly different. The priorities for each area will be decided by the health problems that are found in that area and will be determined after discussion with the local community (Figure 1.5).

1.5.2 Millennium Development Goals
The Millennium Development Goals were launched in September 2000 by 189 countries with the aim of eradicating poverty by 2015. The eight goals (Box 1.4) are intended to combat poverty, hunger, disease, environmental degradation and gender discrimination. Ethiopia has adopted this initiative and set its own eight goals which are: to reduce maternal mortality from greater than 871 to 392 per 100,000 live births, to reduce the under-five mortality rate by 85% and the infant mortality rate from 77 to 45 per 1,000 live births. Infectious disease targets include: maintaining the relatively low prevalence of HIV, reduction of TB-related deaths from 7% to 4% and malaria-related deaths from 22% to 10%.
The Health Service Extension Programme is an approach that is designed to achieve these goals.
Box 1.4 Millennium Development Goals
Goal 1: End extreme poverty and hunger
Goal 2: Achieve universal primary education
Goal 3: Promote gender equality and empower women
Goal 4: Reduce child mortality
Goal 5: Improve maternal health
Goal 6: Combat HIV/AIDS, malaria and other diseases
Goal 7: Ensure environmental sustainability
Goal 8: Develop a global partnership for development.
Look again carefully at Box 1.4. Which of the Millenium Development Goals do you think may be relevant to the work of Health Extension Practitioners?
Health Extension Practitioners will be mostly involved in the health goals (4, 5 and 6), but of course all the other goals are interconnected as well. For example, health in any community is unlikely to improve unless gender inequality is also tackled.
1.6 Achievements of the Ethiopian Health Service Extension Programme
The HSEP has had government support and commitment at all levels, from Federal to kebele administration, from the start. Because of this it has delivered significant improvements in the health status of the people (Box 1.5).
Box 1.5 Achievements and health outcomes of HSEP until the year 2010
- 34,382 female Health Extension Workers have been trained and deployed to date
- 14,192 Health Posts have been constructed so far
- 35.2 million insecticide-treated bed nets (ITNs) have been distributed to families in rural areas
- Under five years old mortality has decreased from 160 per 1,000 live births in 2000, to 109 per 1,000 live births in 2010
- Infant mortality in the first year of life has decreased from 77 deaths per 1000 live births in 2005 to 67 deaths per 1,000 live births in 2009
- The Maternal Mortality Ratio has decreased from 673 to 470 per 100,000 live births
- There has been a decrease in malaria epidemics and a decrease in malaria-related deaths
- Antenatal coverage has increased from 30% in 2002 to 71% in 2010
- Increased childhood immunization rates. DPT3* (a measure of health service utilisation as well as childhood immunization) coverage increased from 38% in 2000 to 86% in 2010
- A total of 9,979,706 Model Households have been trained and graduated by 2010
- Latrine coverage increased from 60% in 2009 to 74% in 2010
- Contraceptive usage rate increased from 56% in 2009 to 62% in 2010
- HIV/AIDS-related deaths have been decreasing.
(Source: Ethiopian Federal Ministry of Health Report, 2010)
*DPT3 refers to completing the three scheduled immunizations against diphtheria, pertussis and tetanus; in Ethiopia these are given combined (in a single pentavalent immunization) with vaccines against hepatitis B and Haemophilus influenza type B.
Look again at Box 1.5. Which of the achievements listed in the box is a health outcome?
Numbers 4, 5, 6, 7 and 13 are all positive health outcomes. These statistics show that the health of people in Ethiopia has been improving since the introduction of the HSEP. All the other statistics show the work that has been done within the HSEP to establish new services and put in place effective preventive measures.
Many elements of the HSEP have been a success and the health of the population has been steadily improving because of the establishment of so many Health Posts and the work of thousands of Health Extension Workers. There have been some particular successes within the programme including:
- Model families
- Community packages
- Interventions at Health Post level.
1.6.1 Implementing the model family package
Health Extension Workers identify and train model families. The selection of model families is criteria-based: model families have been involved in other development work; they are accepted by the community as early adopters, and they enjoy the credibility which comes from having adopted health practices and become role models. As role models, model families help in diffusing health messages (Figure 1.6). This leads to the adoption of improved health practices and behaviours by the community.

1.6.2 Implementing the community package
Health Extension Workers also work with communities to communicate health messages. They involve the community in different stages, from planning to evaluation. Health Extension Workers rely on traditional and modern associations to coordinate and organise the implementation of community packages, e.g. idir, mahber, ekub, schools, women and youth associations.
1.6.3 Implementing interventions at Health Post level
At the Health Post, the Health Extension Workers provide antenatal care, conduct normal and safe deliveries, administer vaccines, conduct growth monitoring, provide nutrition counselling, offer family planning services, and organise referrals for services to the general population of the kebele (Figure 1.7).

Suppose you have planned to undertake a TB eradication campaign within your community. Which of the three Health Post level approaches do you think you should follow to achieve the desired outcome of your plan? Describe the approach you have selected to follow.
Your plan will certainly need the involvement of many people and several other stakeholders–therefore, you should follow the community package approach. This approach allows you to involve the community in all the different stages. Of course a TB eradication campaign will involve all the Model Families in your kebele, but the entire community needs to be involved and therefore the community package approach should be used.
1.7 Development of the Health Service Extension Programme
Despite the improvements in health outcomes achieved through the implementation of HSEP there are still challenges and problems that limit progress in the healthcare services in rural Ethiopia. In Section 1.6 of this study session you learnt about some of the significant improvements in health outcomes throughout Ethiopia and now in this section you will learn about some of the gaps that are apparent and the measures that are being taken to further improve the services.
According to the Federal Ministry of Health’s Health Sector Development III Performance Evaluation Report, there are problems with reading and writing skills amongst some Health Extension Workers, particularly those recruited in pastoralist and semi-pastoralist areas. There have also been requests from the rural community for more curative services to be provided at Health Post level. A lack of in-service training has also been noted. These and other factors have urged the government to improve the knowledge and skills of Health Extension Workers at least to the level that enables them to provide safe and competent preventive and health promotion activities, as well as basic curative services. For this to be realised, these cost-effective blended learning training modules have been created. This module-based training helps you to get your education without having to leave your workplace. Furthermore, this type of learning makes it possible to train significant numbers of Health Extension Workers at the same time.
This study session is the first one that you will study in the Health Management, Ethics and Research Module. It will serve as an introduction to all the other study sessions in the Module.
Summary of Study Session 1
In Study Session 1, you have learned that:
- Ethiopia has radically changed the structure of its health service in order to focus on Primary Health Care and preventive services in the rural communities where most people live.
- Ethiopia’s health delivery system is organised into a four-tier system. Its first level is the Primary Health Care Unit which is based around one Health Centre and five Health Posts serving a total of 25,000 rural people.
- Primary Health Care is the lowest level of essential health care that is provided to the majority of the population of Ethiopia at a cost that the country and the community can afford. It mainly focuses on prevention and control of communicable diseases, and the promotion of health and wellbeing of individuals and families.
- The Health Service Extension Programme (HSEP) is an innovative community-based programme. It is a country-specific health delivery system designed to reach the rural communities where most of the people live. It uses trained and salaried Health Extension Workers/Practitioners to help the community maintain its own health.
Self-Assessment Questions (SAQs) for Study Session 1
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 1.1 (tests Learning Outcome 1.1)
What do you understand by the following terms?
- a.Primary Health Care.
- b.Millennium Development Goals.
- c.Vertical health programmes.
Answer
- a.Primary Health Care is the name given to the essential healthcare that is universally accessible to individuals and is acceptable to them at a cost that the country and each community can afford.
- b.Millennium Development Goals are the goals which the country aspires to achieve by the year 2015 (the year 2008 in the Ethiopian calendar).
- c.Vertical health programmes are designed to tackle single diseases such as malaria.
SAQ 1.2 (tests Learning Outcome 1.2)
During this study session you have learned that Primary Health Care has five principles including a. accessibility, b. community participation and c. health promotion. Why do you think that each of these principles is important? Give examples if you can.
Answer
- a.Accessiblity: Every person needs to be able to get to the health services that will help them maintain their own health, or treat them when they become ill. In Ethiopia the construction of 14,000 Health Posts and the deployment of two trained female Health Extension Workers for each kebele have dramatically improved access in rural areas.
- b.Community participation: The HSEP relies on involving the community in different health and health-related campaigns. For instance, draining swampy areas in the malaria control programme relies on community participation. The Health Extension Practitioner alone cannot achieve these results.
- c.Health promotion: HSEP is focused mainly on prevention and health promotion. For example, selecting model families and educating them in health-related issues has enabled many communities to maintain their own health.
SAQ 1.3 (tests Learning Outcome 1.3)
Suppose you are a newly assigned Health Extension Practitioner who is about to work in a rural Health Post. Before you start your work you have completed an assessment to identify the priority health problems in the community. From your assessment you have identified the following health problems: tuberculosis, nutrition-related health problems of children, pregnant woman seeking support, malaria, and little use of latrines. Please categorise these health problems under the four major components of HSEP. Remember that these are: Disease Prevention and Control, Family Health Service, Hygiene and Environmental Sanitation, and Health Education and Communication.
Answer
Health Education and Communication covers all the four components and should be part of the work dealing with all these health problems. Tuberculosis and malaria are categorised under Disease Prevention and Control, while nutrition-related health problems and pregnant women seeking support will be categorised under Family Health Services. If there is little use of latrines in the community, work to improve uptake will be categorised under Environmental Hygiene and Sanitation.
SAQ 1.4 (tests Learning Outcome 1.4)
Asmera is a Health Extension Worker in Tensyie. When she first came to Tensyie there were no latrines. Two years later, she had managed to convince all 785 households to construct their own latrines. She also improved family planning coverage from 3% to 25%. Her efforts also led to a 72% increase in breastfeeding within two years. What principles of PHC do you think she might have used to bring about these improvements?
Answer
Asmera will have used most of the principles of PHC to have achieved such excellent results. For example, she would have got help from other agencies (inter-sectoral collaboration). She will have also used many community resources (community participation), and made sure that all her services were equally available to everyone in her community (accessibility). None of her work would be possible without effective health promotion and the use of appropriate technology.