Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Thursday, 22 January 2026, 6:01 AM
Health Management, Ethics and Research Module: 8. Ethical Dilemmas in Health Service Delivery
Study Session 8 Ethical Dilemmas in Health Service Delivery
Introduction
In Study Session 7 of this Module you learnt about some of the basic concepts and principles of healthcare ethics that you will meet in your work with individuals, groups and communities. In this study session you are going to learn more about some of the ethical dilemmas that you may well face in your day-to-day activities while providing healthcare services as a Health Extension Practitioner.
This study session will also help you to identify some of the common ethical conflicts that may arise in your day-to-day practice and hopefully learn how to resolve them. You will be able to learn additional useful ethical theories and a specific method of decision making that should help you resolve ethical problems that arise in your work.
Learning Outcomes for Study Session 8
When you have studied this session, you should be able to:
8.1 Define and use correctly all of the key words printed in bold. (SAQ 8.1)
8.2 Identify the ethical dilemmas that exist in a case study presented to you. (SAQs 8.2, 8.3 and 8.4)
8.3 Describe two theories that can help you resolve ethical dilemmas that may arise in your health work. (SAQ 8.3)
8.4 Understand a decision making process that may be able to help you to resolve ethical conflicts. (SAQ 8.4)
8.1 Ethical dilemmas and conflicts
In the previous study session you learnt about some of the core ethical concepts. You will remember that these are autonomy, beneficence, nonmaleficence and justice. In this section you will study more about ethical dilemmas, sometimes called ethical conflicts.
Ethical dilemmas arise when a difficult problem cannot be solved in a way that will satisfy everyone who is involved. The same dilemma might occur when a situation arises that involves a choice between equally unsatisfactory alternatives.
In ethical conflicts, the decision maker is confronted with more than one course of action that respects personal, professional and societal morality, but by deciding on one course of action the other course is harmed in some way. For example, as a Health Extension Practitioner you may face confidentiality conflicts. You are morally and legally obliged to keep patient information confidential; at the same time, you may be required to disclose sensitive information because breaking the rules of confidentiality would benefit the family or the wider community. You will be able to understand the subject better when you go through each of the following common ethical issues listed in Box 8.1. For each of these issues you will be presented with a case study to think about.
Box 8.1 Common ethical issues
- Practitioner–client relationship.
- Privacy and confidentiality.
- Shared decision making.
- Allocation of scarce resources.
- Stigma and illness.
- Reproductive health care.
8.2 Practitioner–client relationship
In the previous study session you learnt about the core ethical concepts of autonomy, beneficence, nonmaleficence and justice. These basic principles should always form the basis for your working relationships. In addition to the above principles there are issues like confidentiality, privacy and trust that you also have to think about at all times.
The following case study will help you to explore some ethical conflicts and ways it might be possible to resolve these conflicts.
Case Study 8.1 Difficult patients
Lemlem, a Health Extension Practitioner at Laelay Michew kebele, Central Zone, Tigray Regional State, is approached by Hailemariam, the son of Ato Gebregziabher, a well known Gena player in his locality. Hailemariam asks Lemlem to provide him with some paracetamol tablets because of pain in his knees. In fact Hailemariam doesn’t have any pain, but he is trying to accumulate enough tablets to commit suicide. He has also bought additional tablets at a market and asked another Health Extension Practitioner for even more tablets. Sometime later Hailemariam swallowed all the tablets at one time and for a while he was very ill, near to death. Hailemariam didn’t die and when he recovered he didn’t want others in the community to discover that he had attempted suicide. He began to spread rumours that Lemlem, the Health Extension Practitioner, was incompetent and had prescribed medication that she does not know how to use and that she had harmed him.
Although this is quite a complicated situation, and hopefully you will never be faced with such a difficult case, people in the community may make false accusations against you. For poor Lemlem the dilemma is something like this: she has done nothing wrong at all. She has prescribed some painkilling tablets with the best of intentions when Hailemariam pretended to have some pains. It is Hailemariam who has deceived her, but then gone on to accuse her, falsely, of being an incompetent practitioner. If she does not defend herself then her position in the community may be damaged. People might believe Hailemariam and start to think that she is not very good at her job. But how can she defend herself while still being professional and ethical in relation to her relationship with her patient Hailemariam?
Can Lemlem’s ethical principles help her in this situation? Perhaps there are principles of justice involved? Lemlem is certainly in the right and should have the opportunity to defend herself against these charges. But defending herself might harm her patient. If she successfully wins her struggle against Hailemariam he might lose face in the community and feel that he has to try to commit suicide again. He does sound as though he is very troubled. He has deep psychological problems and has already tried to kill himself - and now he’s making trouble for Lemlem. Lemlem doesn’t want to harm him (nonmaleficence), but she also feels that she should keep her job and continue to help lots of people in the community (beneficence).
Which of the following actions do you think that it would be ethical and appropriate for Health Extension Practitioner Lemlem to do? Explain your reasons.
- a.Nothing, but let the accusations pass without further comment.
- b.Attack Hailemariam publicly and make sure that everyone knows about his psychological troubles.
- c.Ask for help from an experienced healthworker at the hospital or health centre.
It would be a really good idea for Health Extension Practitioner Lemlem to get some help from an experienced practitioner. They will be able to help clarify her ideas and support her in any action she takes in the future to clear her name. If she responds to her patient in any public way then this could be considered to be a breach of confidentiality and may bring about a complaint against her that would be hard to defend.
8.3 Privacy and confidentiality
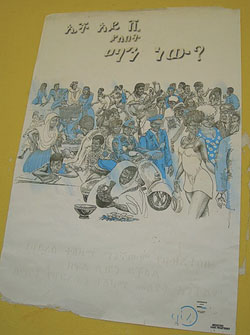
The professional relationship between a Health Extension Practitioner and a client in a rural community is frequently long-term, and may involve the wider families and mutual friends. This closeness may well affect professional responsibilities (Figure 8.1). In this section you will study the ethical conflicts involving privacy and confidentiality in rural healthcare relationships. Confidentiality may involve more complex issues in rural rather than urban settings. People who live in rural areas may well know many of the details of each other’s lives and this intimacy makes ethical conflicts related to privacy and confidentiality more challenging compared to urban settings.

Case Study 8.2 Confidentiality and trust
Ali has been a soldier for the last five years. He’s now returned to his rural village and started to help his father on their farm. He’s a strong and handsome man and soon starts to see a new girlfriend Kedija. Ali comes to the Health Post and shows the Health Extension Practitioner, Workinesh, the results of his recent HIV test – which is positive. Workinesh also has information through her work that neither Kedija nor Ali have asked for, or been given any, condoms. What should Workinesh do?
Almost anything that Workinesh does actively will risk breaking confidentiality. But doing nothing will potentially harm one of her patients, Kedija. If she doesn’t warn Kedija that Ali is HIV positive then Kedija might become infected and become seriously ill and even die (Figure 8.2). Several ethical principles are at stake here including trust, confidentiality and autonomy. Nobody can force Kedija or Ali to act in a particular way because they each have their own autonomy.
Which of the following actions do you think that it would be ethical and appropriate for the Health Extension Practitioner to do? Explain your reasons.
- a.Do nothing and hope that her patient Kedija doesn’t get infected.
- b.Make sure that Ali is aware of his responsibilities and also offer him condoms.
- c.Go round to Kedija’s house and tell her that Ali is HIV positive and that she should use condoms.
- d.Ask for help from an experienced healthworker at the hospital or Health Centre.
Although answer d. is appropriate in this case and Workinesh should always seek appropriate support and assistance in difficult matters, perhaps she can also use her ethical principles to help her decide what else to do. Answer a. is not appropriate ethically. This course of action risks harming her patient. If she does make sure that Ali is made aware of his responsibilities (answer b.), and that he will always use condoms in the future, then she has followed ethical principles and protected her patients to the best of her abilities. Answer c. is probably only possible ethically if she also does b. To tell Kedija the test results of her partner is not ethically acceptable unless this is cleared by the person who has been tested.
8.4 Shared decision making
The key feature of the shared decision making process is a dialogue in which both client and practitioner share information, leading to a decision regarding the client’s healthcare. Shared decision making is based on trust, truthfulness and respect for the client’s choice. For this to be effective, good communication skills are crucial. If some decisions have to be made, for example about transfer to a hospital for further treatment, the patient might be concerned about their own issues, such as their values, religious and cultural beliefs and finances (Figure 8.3). For the Health Extension Practitioner, the discussion should include the risks and benefits of being transferred for better treatment as well as the likely outcome of no treatment. How information is shared, and what information is shared, may influence the patient’s choice. At an ethical level, there is a tension between client autonomy, beneficence and confidentiality that may not be easily resolved. Ethical conflicts, especially involving family members, should be anticipated in shared decision making.

Case Study 8.3 Managing your own decisions
Tadelech is a member of your local community. She is usually a strong woman who is a good mother to her seven children and an active member of the community. Recently she has become seriously ill with a chest infection that has turned into pneumonia. Although the Health Extension Practitioner, Hadas, has tried to convince her that she needs to go to hospital, Tadelech is determined to stay in her own home.
Hadas is in a difficult position. Of course Tadelech should be able to decide about her own health and her own body – this is the basic ethical value of autonomy. But the healthworker knows that without proper treatment she might die and then all Tadelech’s children would suffer. Indeed the whole community would lose one of their important members.
Which of the following actions do you think that it would be ethical and appropriate for Hadas to do? Explain your reasons.
- a.Do nothing and hope that Tadelech recovers from the pneumonia.
- b.Force Tadelech to go to the hospital by carrying her there against her will.
- c.Explain to Tadelech’s husband and parents about the serious nature of her chest infection and hope that they will be able to persuade her to take up the offer of hospital treatment.
- d.Ask for help from an experienced healthworker at the hospital or health centre.
Answer d. will always be appropriate if you are having problems with an ethical dilemma. Seeking the advice of someone more senior or more experienced is almost always helpful. But before seeking advice, answer c. would be well worth trying. Doing extra tasks in order to try to save a life (beneficence) is an ethical principle that is always worth pursuing. Using force, as in answer b., is not correct. This would certainly be against the ethical principle of autonomy. However ill the person is, they still have rights to decide about their own issues.
8.5 Allocation of scarce resources
Health resources, such as financial or human resources, are always scarce whether you are working in developed or developing countries. Using resources to their best effect needs appropriate planning and allocation of resources to areas where they bring about the best outcomes. As a manager and healthcare provider in the Health Post you may be faced with a scarcity of resources (Figure 8.4) and need to make judgements to use your resources wisely so that you are able to satisfy the healthcare needs of the majority of your community (the principle of utility). As a manager and healthcare provider in your community, you may face ethical conflicts with regard to resource allocation.
Following some simple steps for decision making may help you resolve these difficulties (Box 8.2).
Box 8.2 Steps for decision making
- Identify the nature of the problem.
- Gather information and consider the possible ways to resolve the problem.
- Communicate openly and honestly with the community served.
- Involve an expert if possible.
- Implement the decision.

Case Study 8.4 Deciding priorities
Imagine that you are a Health Extension Practitioner in a rural area and you are planning to conduct a vaccination campaign and also a malaria control campaign. Both are necessary to improve the health of your local community, but there are only limited human resources available and it is not possible to do both of these campaigns immediately.
In this situation you need to decide: should you continue with the malaria campaign or the vaccination campaign, or share your resources in some way between both campaigns? There may be ethical principles that you can use to help you make your decision. Both campaigns may be beneficial for members of the community (beneficence), and none of the decisions seem to involve potential breaches of confidentiality. You may need to gather more information about the situation in order to be helped to make the correct decision.
Box 8.2 sets out the steps that can be used in decision making over ethical issues. How might following these steps help you to make the best decision about how to proceed in Case Study 8.4?
Following these steps might give you additional information that will help you take the decision. For example, you might find out that doing both campaigns using reduced resources would make both campaigns ineffective. When you consult both the community and the expert it might become apparent that you should give priority to the malaria control campaign, because this disease cannot wait. If it is not controlled speedily it may kill, or make many people in the community ill within a short period of time. Vaccination of children, on the other hand, can be postponed for another time because if the children are not vaccinated right away this will not necessarily bring about a disastrous health outcome. Remember that there will always be other people who can help you make important decisions, including ethical problems. Often it will help you if you ask your community what they prefer when there are options.
8.6 Stigma and illness
As a Health Extension Practitioner, you will be working in the rural areas where 80–85% of the population of Ethiopia lives. The healthcare practice in rural areas is different from that of urban centres. The closeness you create with individuals, families and the community may make it difficult to decide about any ethical conflicts (dilemmas) that may occur in your day-to-day practice.
One of the serious ethical issues that you may encounter is stigma. Stigma is defined as a negative perception that is assigned to an individual because of any feature that, in the view of others, discredits and diminishes them from other people. The stigmatised person becomes a person who is discounted. In rural healthcare settings, stigma takes on special importance because of the close relationships that exist in small communities. To be viewed negatively by others, to be avoided, and to be seen as less than a full member of the community is a major burden for a person in a rural community.
Case Study 8.5 HIV and stigma
Jemila, a Health Extension Practitioner who is working at one of the Health Posts in Gambella Regional State, attends Ato Ojul’s family. When she visited Ato Ojul’s family she found that W/ro Hawa, the wife of Ato Ojul, is very depressed and tearful. Jemila tried to reassure her but Hawa was not willing to tell her the reason why she was depressed and crying. Later in the course of their discussion, Hawa told Jemila that she is HIV positive and that she is worried what will happen to her because of the stigmatising effect of HIV. If people in the wider community find out that she is HIV positive she fears that she will be an outcast and treated badly.
This is a complicated situation for Jemila to cope with, but there are some ethical principles that she can use to help her. Firstly, Hawa is her patient and must not be harmed by anything that Jemila does now or in the future. She must reassure Hawa about total confidentiality and establish a situation of trust between the two of them. Hawa’s status is safe with Jemila and she can get treatment for her HIV without anyone else being aware.
What steps could Jemila take to address a stigmatising illness such as the HIV that has infected Hawa?
In the short term it is important that trust is established and that Hawa knows that she can rely on Jemila to support her without her problem becoming widely known. In the longer term Jemila can put in place a series of community-based educational activities designed to reduce stigma about diseases such as HIV. When the correct facts about HIV are known by the community they should be able to accept Hawa and not fear or reject her.
8.7 Reproductive healthcare
One of the primary healthcare services that Health Extension Practitioners are expected to provide is reproductive healthcare. During this part of your work it is essential to develop trust with each individual and with the community as a whole. This service requires appropriate levels of care, confidentiality and truth-telling– possibly more than any other part of the health services. However, you may face conflicting situations and ethical issues that hinder you from providing appropriate reproductive healthcare services.
Case Study 8.6 Conflict in the family
Leila, a Health Extension Practitioner, works in a Health Post within the Southern Nations, Nationalities and People’s Region (SNNPR) and provides community health services including family planning support. One Friday she had made a visit to Ato Olano’s family to discuss family planning issues with Ato Olano’s wife, W/ro Abebech. When she finished her discussion, Ato Olano’s oldest daughter, Bekelech (aged 15), came over to Leila and talked about something that was obviously worrying her. She confided in Leila that she has started a loving relationship with Wajo, a student, over the last six months. She says that she really likes him a lot. However she has not started sexual relations, but she has been thinking about it. She is wondering if she could start taking birth control pills. Bekelech also explained that her parents do not know anything about this relationship. She says her mother would be very upset if she knew about it, and asked that this information should not be told to her parents. At the doorway on the way out Abebech and Olano ask Leila what their daughter has been talking about with her.
Although this is a potentially difficult situation for Leila to deal with, this is a common problem and Leila will be able to use some ethical principles to work out the way that she should act in these circumstances. There is definitely a conflict of ethical principles involved in this situation. Ato Olano and his wife Abebech need to be sure that Leila, their healthcare worker, will always tell the truth. Truthfulness is a very important part of all health work. However, Bekelech has been discussing issues that she wants to keep secret from her parents who might be angry. Confidentiality should be expected of all health workers. If Leila tells Bekelech’s parents about the content of the discussion then this is a clear breach of confidentiality whatever the age of the client. Bekelech is exhibiting her own autonomy that is separate from that of her parents.
In this situation how should Leila react? Explain your reasons.
- a.Say nothing and just walk past Bekelech’s parents at the door.
- b.Tell the parents the truth about the discussions she has been having with their daughter.
- c.Tell the parents that they will have to find out what the conversation has been about from their daughter themselves.
- d.Tell the parents that their daughter was worried about some spots on her face or some other common problem to avoid telling them the truth.
Each Health Extension Practitioner will find ways for themselves of dealing with difficult situations. Some people may think that d. is an acceptable solution because they feel that telling a lie (about the spots) will cause less damage for Bekelech than telling the truth in this situation. Solution a. is almost certainly going to lose Leila her good reputation as an approachable healthworker, while b. involves a breakdown in trust between her and her patient, Bekelech. If Leila tells the parents that they will have to find out the subject of the discussion from their own daughter (answer c.), this accepts the autonomy of the daughter herself. Bekelech will be put in a situation of having to decide for herself whether to tell her own parents what she has been thinking about and the reality of her relationship with Wajo. In an ideal world, of course, the parents would come to accept that asking advice about family planning has been a responsible thing for Bekelech to do and support her decision to ask before starting a sexual relationship.
Summary of Study Session 8
In Study Session 8, you have learned that:
- Healthworkers will be faced with difficult decisions during their working lives. Some of these will involve ethical dilemmas or conflicts.
- Using ethical principles may help to resolve some of the complex problems that may occur during your work.
- Confidentiality, privacy and trust are issues that all healthworkers should strive to maintain at all times.
- There are some areas of responsibility in healthworkers’ lives that are more likely to cause ethical dilemmas than other parts of their work.
- Asking for help when difficult ethical matters arise is almost always a good idea.
Self-Assessment Questions (SAQs) for Study Session 8
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the following questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 8.1 (tests Learning Outcome 8.1)
Can you give an example of a stigma that can be caused by a medical condition? How might stigma be avoided?
Answer
There are lots of examples of stigma following medical conditions that you could have chosen. Often people with infectious diseases, such as HIV or AIDS, are stigmatised because of their medical condition. Stigma can be reduced or avoided if proper education is given to the community. If they understand about an infection such as HIV then there is no reason why a person with HIV should be stigmatised.
Read Case Study 8.7 and answer the questions that follow.
Case Study 8.7 Ethical dilemmas
Amarech is providing antenatal care for W/ro Alemach, wife of Ato Feleke. Alemach is 26 weeks pregnant. This is her third pregnancy and the previous two deliveries were safe. When W/ro Alemach comes to the Health Post for her appointment, she complains of a burning sensation during urination and a yellowish discharge from her birth canal. Amarech has told W/ro Alemach that this is almost certainly caused by an infection acquired by sexual intercourse. She asks W/ro Alemach to tell the truth if she has had extra-marital sex because this might be the source of infection and the cause of her symptoms. W/ro Alemach eventually admits that she has had an affair with Ato Tadesse, a well-known community member, who is the likely source of the infection. Her husband does not know about the extra-marital relationship and she does not want him to know. She is certain her husband is the father of the child she is carrying. She asks Amarech to provide treatment for her infection and not to tell her husband about her situation.
SAQ 8.2 (tests Learning Outcome 8.2)
What is an ethical dilemma or ethical conflict? Identify the main ethical dilemmas and conflicts in Case Study 8.7.
Answer
From Case Study 8.7 you can extract a number of ethical issues or conflicts. Amarech has the responsibility to keep W/ro Alemach’s medical secret. Confidentiality is the core ethical principle in this case study. If Amarech tells Ato Feleke about his wife’s infection, W/ro Alemach may end up being divorced. The principle of nonmaleficence would be violated. If Amarech keeps the secret there is a probability of transmitting the infection to Ato Feleke and the principles of beneficence and nomaleficence would be violated. The best solution to those conflicting issues is to encourage Alemach to tell her husband herself. This would involve the principle of autonomy.
SAQ 8.3 (tests Learning Outcomes 8.2 and 8.3)
Which ethical theories might be helpful to resolve the ethical dilemmas that you have identified in Case Study 8.7? Describe at least one theory that might be helpful.
Answer
There are several ethical theories that could be used to resolve the dilemmas that have been identified in Case Study 8.7. Confidentiality and truthfulness are at the centre of the case study, but autonomy, beneficence and nonmalefience may also be useful.
SAQ 8.4 (tests Learning Outcomes 8.2 and 8.4)
Describe how the decision-making steps found in Box 8.2 might help the resolution of the ethical conflicts that you have identified in Case Study 8.7.
Answer
The decision-making steps found in Box 8.2 might help the resolution of the ethical conflicts in Case Study 8.7 because a logical approach to sorting out the problems will help you think clearly about the problem and how to solve it.