Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Friday, 19 April 2024, 7:53 AM
Integrated Management of newborn and Childhood Illness Module: 1. An Introduction to the Integrated Management of Newborn and Childhood Illness (IMNCI)
Study Session 1. An Introduction to the Integrated Management of Newborn and Childhood Illness (IMNCI)
Introduction
Every year about 9 million children in developing countries die before they reach their fifth birthday, many of them during the first year of life. Ethiopia has one of the highest under-five mortality rates with more than 321,000 children under the age of five dying every year. More than 70% of these child deaths are due to five diseases, namely pneumonia, diarrhoea, malaria, measles and malnutrition, and often to a combination of these conditions.
These diseases are also the reasons for seeking care for at least three out of four children who come to health facilities. As children usually present with more than one of these conditions, it was recognised that there was a need for an integrated approach in order to manage the child in a holistic manner (taking into account all of the child’s problems including the major childhood illnesses in the assessment and treatment of illness). This led to the development of the Integrated Management of Newborn and Childhood Illness (IMNCI) strategy.
IMNCI is an integrated approach to child health that focuses on the wellbeing of the whole child. IMNCI aims to reduce death, illness and disability, and to promote improved growth and development among children under five years of age. IMNCI includes both preventive and curative elements that are implemented by families and communities as well as by health facilities. In summary, the IMNCI strategy includes three main components:
- Improving case management skills of healthcare staff.
- Improving the health systems.
- Improving family and community health practices.
In health facilities, the IMNCI strategy:
- promotes the accurate identification of childhood illnesses in out-patient settings
- ensures appropriate combined treatment of all major illnesses
- strengthens the counselling of caregivers
- speeds up the referral of severely ill children.
In the home setting, IMNCI:
- promotes appropriate care-seeking behaviours
- helps to improve nutrition and preventative care, and
- supports the correct implementation of prescribed care.
The integrated case management process taught in this Module will help you to quickly consider all of a child’s symptoms and not overlook any problems. You will learn how to determine if a child is severely ill and needs urgent referral. You will also learn how to treat a child’s illness and how to counsel caregivers to treat a child at home for those infants and children who do not need to be referred urgently. This study session outlines the guidelines for counselling mothers and other caregivers, something which you will also look at in more detail in Study Session 14 of this Module.
Learning Outcomes for Study Session 1
When you have studied this session, you should be able to:
1.1 Define and use correctly all of the key words printed in bold. (SAQs 1.1, 1.2 and 1.3)
1.2 Define the importance and objectives of the IMNCI strategy. (SAQ 1.1)
1.3 Summarise the main steps of the IMNCI assessment. (SAQ 1.2)
1.4 Describe the general danger signs (GDS). (SAQs 1.1 and 1.3)
First, you are going to look into the importance of the IMNCI strategy and the diseases that are addressed by this strategy.
1.1 The IMNCI strategy
IMNCI is a strategy that integrates all available measures for health promotion, prevention and integrated management of childhood diseases through their early detection and effective treatment, and promotion of healthy habits within the family and community.
1.2 Importance and objectives of the IMNCI strategy
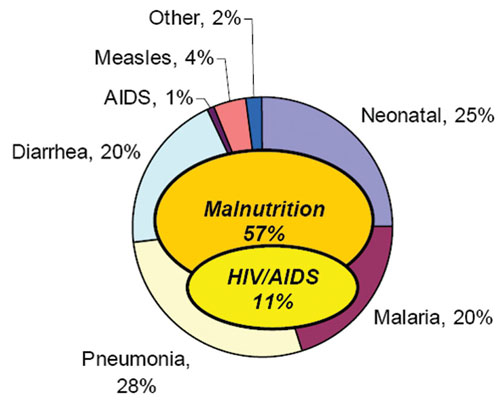
The importance of having an Integrated Management of Newborn and Childhood Illness strategy is that it enables a consistent and standardised approach that addresses the major causes of under-five morbidity and mortality which are responsible for more than 90% of the mortality in this age group in Ethiopia. As shown in Figure 1.1 below, the major causes of under-five mortality have been estimated as follows: pneumonia 28%, neonatal problems 25%, malaria 20%, diarrhoea 20%, measles 4%, AIDS 1% and other causes 2%. As you can also see in Figure 1.1, malnutrition is associated with nearly 60% of mortality in under-five children.
1.2.1 Objectives and advantages of IMNCI
The objectives of the IMNCI strategy are:
- to reduce mortality and morbidity associated with the major causes of disease in children less than five years of age, and
- to contribute to the healthy growth and development of children.
The IMNCI guidelines are designed for the management of sick children from birth up to five years old.
As you read in the introduction, the core of the IMNCI strategy is integrated case management of the most common childhood problems, with a focus on the most important causes of death. The clinical guidelines are designed for the management of sick children aged from birth up to five years. They include methods for assessing signs that indicate severe disease; assessing a child’s nutrition, immunization and feeding; teaching parents how to care for a child at home; counselling parents to solve feeding problems; and advising parents about when to return to a health facility. The guidelines also include recommendations for checking the parents’ understanding of the advice given and for showing them how to administer the first dose of treatment.
Why is IMNCI an important strategy for you to know as a Health Extension Practitioner?
IMNCI will enable you to help reduce the number of babies and children in your community who become ill or die. It will also help you to promote the healthy growth and development of babies and children in the community.
When correctly applied, IMNCI has the following advantages:
- Promotes the accurate identification of childhood illnesses in out-patient settings
- Ensures appropriate combined treatment of all major childhood illnesses
- Strengthens the counselling of mothers or caregivers
- Strengthens the provision of preventive services
- Speeds up the referral of severely ill children
- Aims to improve the quality of care of sick children at the referral level.
1.3 The IMNCI assessment
When you are assessing a sick child, a combination of individual signs leads to one or more classifications, rather than to a diagnosis. IMNCI classifications are action-oriented illness categories which enable a healthcare provider to determine if a child should be urgently referred to a health centre, if the child can be treated at the health post (e.g. with oral antibiotic, antimalarial, ORS, etc.), or if the child can be safely managed at home.

The IMNCI guidelines describe how you should care for a child who is brought to your health post with an illness, or for a scheduled follow-up visit to check the child’s progress. The guidelines give instructions for how to routinely assess a child for general danger signs (or possible bacterial infection in a young infant), common illnesses, malnutrition and anaemia, and to look for other problems. In addition to treatment, the guidelines incorporate basic activities for illness prevention.
This module will help you learn to use the IMNCI guidelines in order to interview caregivers, accurately recognise clinical signs, choose appropriate treatments, and provide counselling and preventive care.
1.4 IMNCI case management
Case management can only be effective to the extent that families bring their sick children to a trained health worker such as you for care in a timely way. If a family waits to bring a child to a health facility until the child is extremely sick, or takes the child to an untrained provider, the child is more likely to die from the illness. Therefore, teaching families when to seek care for a sick child is an important part of the case management process and is a crucial part of your role as a Health Extension Practitioner.
The complete IMNCI case management process involves the elements listed in Box 1.1.
Box 1.1 The IMNCI case management process
Assessment
- Assess a child by checking first for general danger signs (or possible bacterial infection in a young infant), asking questions about common conditions, examining the child, and checking nutrition and immunization status. Assessment includes checking the child for other health problems.
Classification
- Classify a child’s illnesses using a colour-coded classification system. Because many children have more than one condition, each illness is classified according to whether it requires:
- urgent pre-referral treatment and referral (pink), or
- specific medical treatment and advice (yellow), or
- simple advice on home management (green).
Identify treatment and treat
- After classifying all conditions, identify specific treatments for the child. If a child requires urgent referral, give essential treatment before the patient is transferred. If a child needs treatment at home, develop an integrated treatment plan for the child and give the first dose of drugs in the clinic. If a child should be immunized, give immunizations.
- Provide practical treatment instructions, including teaching the caregiver how to give oral drugs, how to feed and give fluids during illness, and how to treat local infections at home. Ask the caregiver to return for follow-up on a specific date, and teach her how to recognise signs that indicate the child should return immediately to the health post.
- Assess feeding, including assessment of breastfeeding practices, and counsel to solve any feeding problems found. Then counsel the mother about her own health.
Follow-up care
- When a child is brought back to the health post as requested, give follow-up care and, if necessary, reassess the child for new problems.
All these steps are clearly presented in the IMNCI chart booklet and you need to refer to it throughout this Module. You should always use the chart booklet whenever you manage under-five children.
Whenever a sick baby or child under five comes to your health post you should use the IMNCI chart booklet to help you know how to assess, classify and treat the child.
The IMNCI guidelines address most, but not all, of the major reasons a sick child is brought to a health facility. A child returning with chronic problems or less common illnesses may require special care which is not described in this Module. For example, the guidelines do not describe the management of trauma or other acute emergencies due to accidents or injuries.
You are now going to look at the case management process in more detail.
1.4.1 The IMNCI case management process
You need to know the age of the child in order to select the appropriate chart and begin the assessment process. The IMNCI case management process is presented on two different sets of charts: one for managing sick young infants aged from birth up to two months and a separate one for managing sick children aged from two months up to five years. First decide which chart to use depending on the age of the child. Up to five years means the child has not yet had his or her fifth birthday. If the child is not yet two months of age, the child is considered a young infant. A child who is two months old would be in the group two months up to five years, not in the group birth up to two months. When you look the IMNCI chart booklet you will see the different charts for the two age groups.
Since management of the young infant aged from birth up to two months is somewhat different from the management of older infants and children, it is described on a different chart:
- Assess, classify and treat the sick young infant.
The case management process for sick children aged two months up to five years is presented on three charts:
- Assess and classify the sick child
- Treat the child
- Counsel the mother.
If this is the child’s first visit for this episode of an illness or problem, then this is an initial visit. If the child was seen a few days before for the same illness, this is a follow-up visit. A follow-up visit has a different purpose from an initial visit. You will learn more about follow-up visits in all of the study sessions in this Module. Whether it is an initial or follow-up visit, the mother may well be feeling anxious and it is important that you put her at her ease. This will increase the likelihood of you being able to obtain important information about her child.
For each visit, when you see the mother, or the child’s caregiver, with the sick child:
- Greet the mother appropriately and ask about the child
- Take the child’s weight and temperature and record the measurements
- Ask the mother what the child’s problems are
- Determine if this is an initial or follow-up visit for this problem.
Which IMNCI process should you follow when a mother visits your health post with her sick child?
There are two sets of charts, one for babies up to the age of two months and one set of three charts for babies and children from two months to five years. Therefore you should find out the age of the child from the mother or from a record chart if this is a follow-up visit and there is already information available to you. This will tell you which chart you should use to assess, classify and determine the correct treatment and follow-up care.
So you can provide the best advice, you need to know what the general danger signs are in sick infants and children. You are going to learn about these next.
1.5 General danger signs (GDS)
Since IMNCI takes a holistic approach to assessing, classifying and treating childhood illnesses it is important to look for general danger signs as well as symptoms and signs of specific childhood illnesses.
The general danger signs are signs of serious illness that are seen in children aged two months up to five years and will need immediate action to save the life of the child. There are five general danger signs and these are set out in Box 1.2 below (reproduced from the IMNCI Assess and Classify Chart Booklet, FMOH Ethiopia, June 2008). Make sure that any infant or child with any danger sign is referred after receiving urgent pre-referral treatment.
Box 1.2 Checking for general danger signs
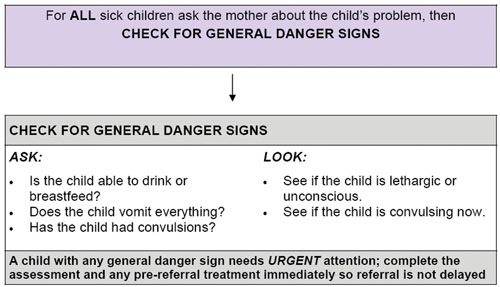
As you can see in Box 1.2, there are key questions you need to ask and signs you need to look for.
![]() You should assess all sick children who come to your health post for general danger signs. Most children with a general danger sign need urgent referral to hospital.
You should assess all sick children who come to your health post for general danger signs. Most children with a general danger sign need urgent referral to hospital.
A child with a general danger sign has a serious problem. Most children with a general danger sign need urgent referral to hospital. They may need lifesaving treatment with injectable antibiotics, oxygen or other treatments that may not be available in the health post. You should complete the rest of the assessment immediately and give urgent pre-referral treatments before sending the patient to the next facility. You will learn more about this later in this study session.
You are first going to look in more detail how you check for general danger signs.
ASK: Is the child able to drink or breastfeed?
A child has the sign ‘not able to drink or breastfeed’ if the child is not able to suck or swallow when offered a drink or breastmilk.
When you ask the mother if the child is able to drink, make sure that she understands the question. If the mother replies that the child is not able to drink or breastfeed, ask her to describe what happens when she offers the child something to drink. For example, is the child able to take fluid into his mouth and swallow it?
If you are not sure about the mother’s answer, ask her to offer the child breastmilk or a drink of clean water. Look to see if the child is swallowing the breastmilk or water.
A child who is breastfed may have difficulty sucking when his nose is blocked. If the child’s nose is blocked, clear it. If the child can breastfeed after the nose is cleared, the child does not have the danger sign, ‘not able to drink or breastfeed’.
ASK: Does the child vomit everything?
A child who is not able to hold anything down at all has the sign ‘vomits everything’. A child who vomits everything will not be able to hold down food, fluids or oral drugs. A child who vomits several times but can hold down some fluids does not have this general danger sign.
When you ask the question, use words the mother understands. Give her time to answer. If the mother is not sure if the child is vomiting everything, help her to make her answer clear. For example, ask the mother how often the child vomits. Also ask if each time the child swallows food or fluids, does the child vomit? If you are not sure of the mother’s answers, ask her to offer the child a drink. See if the child vomits.
ASK: Has the child had convulsions?
During a convulsion, the child’s arms and legs stiffen because the muscles are contracting or if the child has repeated abnormal movements. The child may lose consciousness or not be able to respond to spoken directions. Ask the mother if the child has had convulsions during this current illness. Use words the mother understands. For example, the mother may know convulsions as ‘fits’ or ‘spasms’. See also if the child is convulsing now.
LOOK to see if the child is lethargic or unconscious
A lethargic child is not awake and alert when he should be. The child is drowsy and does not show interest in what is happening around him. Often the lethargic child does not look at his mother or watch your face when you talk. The child may stare blankly and appear not to notice what is going on around him. An unconscious child cannot be wakened. He does not respond when he is touched, shaken or spoken to.
Ask the mother if the child seems unusually sleepy or if she cannot wake the child. Look to see if the child wakens when the mother talks or shakes the child or when you clap your hands. However, if the child is sleeping and has cough or signs of difficult breathing, you must count the number of breaths first before you try to wake the child because it is easier to count the exact breathing rate when the child is calm.
When you have completed the above steps, you should record what you have found on the sick child case recording form. You must circle any general danger signs that are found, and check (✓) against the appropriate answer (yes or no) in the classify column. Case study 1.1 below illustrates the assessment process for general danger signs in practice.
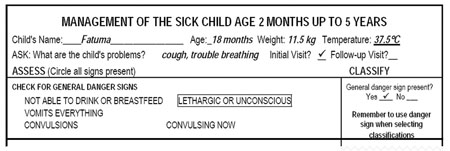
Case Study 1.1 Fatuma’s story
Fatuma is 18 months old. She weighs 11.5 kg. Her temperature is 37.5°C. The health worker asked, ‘What are the child’s problems?’ The mother said ‘Fatuma has been coughing for six days, and she is having trouble breathing’. This is the initial visit for this illness.
The health worker checked Fatuma for general danger signs. The mother said that Fatuma was able to drink. She had not been vomiting. She had not had convulsions during this illness. The health worker asked, ‘Does Fatuma seem unusually sleepy?’ The mother said, ‘Yes’. The health worker clapped her hands. She asked the mother to shake the child. Fatuma opened her eyes, but did not look around. The health worker talked to Fatuma, but the child did not watch her face. Fatuma stared blankly and appeared not to notice what was going on around her.
The top part of the sick child case recording form for the above case is reproduced for you in Figure 1.2 below. You can see the relevant information from the case study has been recorded.
![]() For any child who has a general danger sign you must complete the rest of the assessment process immediately. The presence of a general danger sign indicates a severe classification and the need for urgent referral.
For any child who has a general danger sign you must complete the rest of the assessment process immediately. The presence of a general danger sign indicates a severe classification and the need for urgent referral.
If the child has a general danger sign you should complete the rest of the assessment process immediately. After checking the general danger signs, you should assess the child for cough/difficult breathing, diarrhoea, fever, ear problems, malnutrition, anaemia and HIV. The presence of any one of the general danger signs indicates a severe classification. A child with a general danger sign or a severe classification should be referred immediately to the health centre after giving appropriate pre-referral treatments.
In Case Study 5.1, Fatuma has the general danger sign ‘lethargic or unconscious’ which is a severe problem. You would complete the rest of the IMNCI assessment and refer her urgently after giving the necessary pre-referral treatments for her classifications, including treatment to prevent low blood sugar. Since she is able to feed, you would ask the mother to breastfeed Fatuma or give her a coffee cup of milk or sugar-water solution. You will learn about the pre-referral treatments in the subsequent study sessions in this Module.
What action should you take if a child has one or more of the general danger signs?
From the materials you have read so far, you know that if a child has any one of the five general danger signs, that child must be considered seriously ill and therefore you should make an immediate referral to a health centre.
This study session has introduced you to the IMNCI case management process and outlined the importance of this in helping to reduce death, illness and disability for babies and children in your community. You have seen that you have an important role to play in this respect. The remaining study sessions in this module will explain to you how to assess and treat children and young infants with a range of conditions, including:
- cough/difficult breathing, diarrhoea, fever, ear problems, malnutrition and anemia, HIV, immunization status and other problems (all sick children)
- serious bacterial infection, diarrhoea, HIV infection, feeding problems or low weight, immunization status and other problems (young infants).
Summary of Study Session 1
In Study Session 1, you have learned that:
- IMNCI aims to reduce death, illness and disability, and to promote improved growth and development among children under five years of age.
- The IMNCI strategy addresses the major causes of under-five morbidity and mortality which are responsible for more than 90% of the mortality, namely pneumonia, neonatal problems, diarrhoea, malaria, measles and malnutrition.
- The IMNCI case management process involves a stepwise approach consisting of the following elements: assessment, classification, treatment, counselling and follow-up.
- All children aged two months up to five years should be checked first for the five general danger signs: inability to drink or breastfeed, vomiting everything, history of convulsions during the current illness, lethargy or unconsciousness and convulsions now.
- A child with any general danger sign should be referred urgently after receiving urgent pre-referral treatment.
Self-Assessment Questions (SAQs) for Study Session 1
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 1.1 (tests Learning Outcomes 1.1, 1.2 and 1.4)
Why is the IMNCI strategy so important for Ethiopia? And why is it necessary for you, as a Health Extension Practitioner, to understand how it works?
Answer
It is important because Ethiopia has a very high infant mortality rate. Most children die from pneumonia, diarrhoea, malaria, measles or malnutrition and the IMNCI strategy is a way of reducing these deaths. The way it does this is by bringing together all the different ways illnesses can be prevented and treated, in the home and the health centre. You need to understand how it works because you will be the person who will be using the strategy and explaining to parents the reasons for everything you do.(Don’t worry if you didn’t say this exactly — there are many ways of explaining your role within the strategy.)
SAQ 1.2 (tests Learning Outcomes 1.1 and 1.3)
What are the four main steps you have to take each time a sick child is brought to you? Try to explain why each of these steps is essential and must not be missed out, using your own words.
Answer
The four main steps are assessment, classification, identify treatment and follow-up care.
Assessment is important in order to get an overall picture of the child’s health. Classification enables you to decide what exactly is wrong with the child. (This may include several illnesses.) Treatment is what will get the child better and may include referral to a hospital. And finally, follow-up is to ensure the child continues to improve.
Read Case Study 1.2 and then answer the questions that follow.
Case Study 1.2 Salem’s story
Salem is 15 months old. She weighs 8.5 kg. Her temperature is 38°C. She lives in a high malaria risk area. The health worker asked, ‘What are the child’s problems?’ The mother said, ‘Salem has been coughing for four days, and she is not eating well’. This is Salem’s initial visit for this problem. The health worker checked Salem for general danger signs. She asked, ‘Is Salem able to drink or breastfeed?’ The mother said, ‘No. Salem does not want to breastfeed’. The health worker gave Salem some water. She was too weak to lift her head. She was not able to drink from a cup. Next she asked the mother, ‘Is she vomiting?’ The mother said, ‘No’. Then she asked, ‘Has she had convulsions?’ The mother said, ‘No’. The health worker looked to see if Salem was convulsing or lethargic or unconscious. She was not convulsing but was lethargic.
SAQ 1.3 (tests Learning Outcomes 1.1 and 1.4)
- a.Does Salem have any danger signs? If so, what are they?
- b.What do you need to do next and why?
Answer
- a.Salem has the general danger signs of ‘not being able to feed’ and ‘lethargic and unconscious’.
- b.You need to complete the rest of the IMNCI assessment and refer her urgently after giving the necessary pre-referral treatments for her classifications, including treatment to prevent low blood sugar.