Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Wednesday, 3 December 2025, 2:42 AM
Integrated Management of Newborn and Childhood Illness Module: 7. Assessment of Malnutrition and Anaemia in the Sick Child
Study Session 7. Assessment of Malnutrition and Anaemia in the Sick Child
Introduction
This study session provides you with the knowledge and skills to undertake the accurate assessment and classification of children suffering from malnutrition and anaemia. This session will help you integrate the theory of assessment and classification of these diseases with the practice of treating these diseases. It also provides you with the knowledge of how to recognise signs of malnutrition and anaemia. You will need this information for Study Session 8 which will teach you how to manage and treat malnutrition and anaemia in a sick child.
Learning Outcomes for Study Session 7
When you have studied this session, you should be able to:
7.1 Define and use correctly all of the key words printed in bold. (SAQs 7.1, 7.2 and 7.3)
7.2 Correctly assess the sick child for the presence of specific signs of acute malnutrition and anaemia. (SAQs 7.1, 7.2 and 7.3)
7.3 Correctly classify the sick child for malnutrition and anaemia based on the presence or absence of specific signs. (SAQ 7.2)
7.4 Identify and distinguish moderate, severe and acute malnutrition. (SAQs 7.1 and 7.3)
7.5 Classify the different causes of malnutrition. (SAQs 7.1 and 7.3)
7.1 Malnutrition
Malnutrition is a condition that occurs when a person does not get enough nutrients. Malnutrition mainly affects children under five in developing countries and results in poor health. The malnourished child will also perform poorly at school and will be a less productive adult in the future.
7.1.1 Causes of malnutrition
There are several causes of malnutrition that can vary from country to country. They can be classified as root causes, underlying causes and immediate causes. Immediate causes of malnutrition are:
Inadequate dietary intake: this is when a child is not getting enough nutrients from his or her food to meet the nutritional needs of its body.
Frequent attacks of illness: a child who has had frequent illnesses can develop malnutrition. During illness the child’s appetite decreases; the food eaten might not be absorbed or it may be vomited; the food that the child eats is not used efficiently, or it may not be enough for the increased metabolic need of the child’s body.
7.1.2 Types of malnutrition
There are two types of malnutrition:
- Protein-energy malnutrition
- Micronutrient malnutrition or deficiency.
Protein-energy malnutrition
Protein-energy malnutrition, as its name implies, is lack of adequate protein and/or calories in the body. This can be acute or chronic.
Chronic protein-energy malnutrition is manifested by stunting, which means short height or length for age. Stunting occurs as a result of lack of food, or an illness which has been there for a long period of time.
Acute protein-energy malnutrition is the term used to cover both moderate and severe wasting and nutritional oedema, which is swelling of parts of the body due to fluid building up in the tissues (also known as kwashiorkor). Acute protein-energy malnutrition occurs as a result of a recent lack of nutrients or illness. This study session focuses in particular on acute malnutrition.
Micronutrient malnutrition or deficiency
A child whose diet lacks the recommended amounts of essential vitamins and minerals can develop micronutrient malnutrition. The child may not be eating enough of the recommended amounts of specific vitamins (such as vitamin A) or minerals (such as iron). Examples of foods that are rich in vitamin A include liver, egg yolk, milk and milk products from animals, as well as green leaves and yellow fruits and vegetables from plants. Foods that are rich in iron include animal sources such as flesh or meat, and foods prepared from blood and organs such as the liver of birds and fish.
Other causes of anaemia
A child can also develop anaemia as a result of:
- Infections
- Parasites such as hookworm or whipworm: these parasites can cause blood loss from the gut and lead to anaemia
- Malaria: often anaemia is a result of a combination of malnutrition and malaria.
7.2 Checking the sick child for malnutrition and anaemia
All children who are brought to the health post for consultation with you should be checked for malnutrition and anaemia. A mother may bring her child to the health post because the child has an acute illness and specific complaints that may point to malnutrition or anaemia. A sick child can be malnourished, but the child’s family may not have realised this problem.
A child with malnutrition has a higher risk of disease and death. Even children with mild and moderate malnutrition have an increased risk of death. Identifying children with malnutrition and treating them is therefore a critically important part of your role as a Health Extension Practitioner. Some malnutrition cases can be treated at home, while severe cases need treatment in an out-patient therapeutic programme (OTP), or referral to a health centre or hospital for special feeding, blood transfusion, or specific treatment of a disease contributing to malnutrition (such as tuberculosis or HIV).
You are now going to learn how you should assess all sick children for malnutrition and anaemia.
7.3 Assessing for malnutrition
There are a number of indicators which tell you that a child is malnourished.
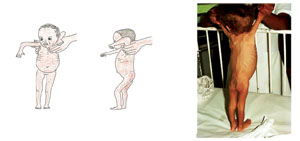
7.3.1 Visible severe wasting in infants less than six months of age
An infant with visible severe wasting has marasmus, a form of severe malnutrition. A child has this sign if he is very thin, has reduced subcutaneous fat, and looks like skin and bones. Some children are thin but do not have visible severe wasting. A child with visible severe wasting needs urgent treatment and you should refer him to a hospital.
Subcutaneous means ‘under the skin’.
To look for visible severe wasting, remove the child’s clothes. Look for severe wasting of the muscles of shoulders, arms, buttocks and legs. Look to see if the outline of the child’s ribs is easily seen. Look at the child’s hips. They may look small when you compare them with the chest and abdomen. Look at the child from the side to see if the fat of the buttocks is missing. When wasting is extreme, there are many folds of skin on the buttocks and thighs. It looks as if the child is wearing baggy pants. The illustrations and photo in Figure 7.1 show you how a child with visible severe wasting looks.
The face of a child with visible severe wasting may still look normal. The child’s abdomen may be large or distended.
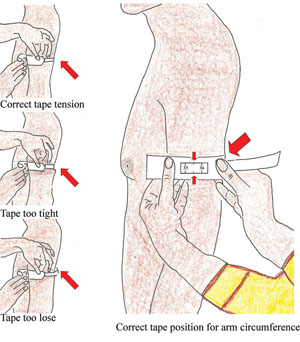
7.3.2 The mid upper arm circumference (MUAC)
For children aged six months or more, the most feasible way to determine wasting or acute malnutrition is by measuring their mid upper arm circumference (MUAC). A MUAC of less than 11.0 cm indicates severe acute malnutrition.
Steps of MUAC measurement
- Ask the mother to remove any clothing that covers the child’s arm. If possible the child should stand erect and sideways to the measurer.
- Estimate the mid-point of the left arm.
- Straighten the child’s arm and wrap the tape around at the mid-point. Make sure that the numbers are right side up. Make sure the tape is flat around the skin.
- Inspect the tension of the tape on the child’s arm. Make sure the tape has the proper tension and is not too tight or too loose. Repeat any step as necessary.
- When the tape is in the correct position and correct tension on the arm, read and call out the measurement to the nearest 0.1 cm.
- Immediately record the measurement.
Figure 7.2 below illustrates how to measure MUAC.
7.3.3 Look and feel for oedema of both feet
A child with oedema of both feet may have kwashiorkor. To determine the presence of oedema, press gently with your thumb on the topside of each foot for at least three seconds (or a count of 101; 102; 103); the child has pitting oedema if a dent remains following the pressing. Look at Figure 7.3 which shows you how a child’s feet look when the dent remains.

7.3.4 Measuring a child’s weight
Knowing the child’s weight will be important for at least three reasons. It will enable you:
- To monitor the growth of a child over time using a standard WHO growth chart, and to counsel the mother on feeding if the child’s weight is found to be low.
- To evaluate the progress of a child who is receiving nutritional treatment in an outpatient therapeutic programme (OTP) or supplementary feeding programme (SFP). Baseline data for and subsequent follow-up of the child’s weight is therefore needed to decide the management of that child.
- To determine the dose of drug for the sick child.

Children are weighed by using a 25 kg hanging spring scale graduated to 0.1 kg (see Figure 7.4). You should not forget to re-adjust the scale to zero before each weighing. A plastic washing bowl should be attached by four ropes that go underneath the bowl. The bowl needs to be close to the ground in case the child falls out, and to make the child feel secure during weighing. If the basin is dirtied, then it should be cleaned with disinfectant. This is much more comfortable and familiar for the child; it can be used for ill children and is easily cleaned.
When the child is steady, record the measurement to the nearest 100 gm (the frame of the scale should be at eye level). Each day, the scales must be checked and calibrated by using a known weight. Suitable items for the calibration include a stone or a standard 5–10 kg weight. If the measure does not match the weight to within 0.01 kg, the scale should be replaced. Spring balance scales should be replaced whenever the springs become too stretched.
As a Health Extension Practitioner you are expected to determine the classification of a child for malnutrition on the basis of visible severe wasting, oedema and MUAC measurements, and to treat the child based on the presence or absence of these signs. Weight in particular is used for monitoring the child and when making a decision whether to discharge a child from an OTP.
7.3.5 Assessing appetite
If a child aged six months or above has a MUAC less than 11 cm or pitting oedema of both feet and has no medical complications, you should assess the child’s appetite.
An appetite test is not needed when the child has any one of the following: medical complications that require in-patient care, pneumonia, persistent diarrhoea, watery diarrhoea, dysentery, malaria, measles, low body temperature or high fever, open skin lesions or signs of vitamin A deficiency.
The appetite test
The appetite test has a number of steps you should follow:
- The appetite test should be conducted in a separate quiet area.
- You should explain to the caregiver the purpose of the appetite test and how it will be carried out.
- The caregiver, where possible, should wash their hands.
- The caregiver should sit comfortably with the child on their lap and either offer the child ready-to-use therapeutic food (RUTF) such as Plumpy’nut® or BP-100® from the packet, or put a small amount on her finger and give it to the child.
- The caregiver should offer the child the RUTF gently, encouraging the child all the time. If the child refuses, then the caregiver should continue to quietly encourage the child and take time over the test. The test usually takes 15‒30 minutes but may take up to one hour. The child must not be forced to take the RUTF.
- The child needs to be offered plenty of water to drink from a cup when taking the RUTF.
You interpret the result of the appetite test in the following way:
Pass: a child that takes at least the amount shown in Table 7.1 below passes the appetite test. You should:
- Explain to the caregiver the choices of treatment and decide with the caregiver whether the child should be treated as an out-patient or an in-patient (nearly all caregivers will opt for out-patient treatment).
- Refer the child to the Out-patient Therapeutic Programme (OTP) for registration and initiation of treatment.
Fail: a child that does not take at least the amount of RUTF shown in Table 7.1 below should be referred for in-patient care. You should:
- Explain to the caregiver the reasons for recommending in-patient care; decide with the caregiver whether the child will be treated as an in-patient or an out-patient.
- Refer the child to the nearest therapeutic feeding unit (TFU) or hospital.
The appetite test should always be performed carefully. You should always offer treatment as an in-patient for children who fail their appetite tests. If there is any doubt, however, then you should refer the child for in-patient treatment until their appetite returns.
APPETITE TEST This is the minimum amount that malnourished children should take to pass the appetite test | |||
|---|---|---|---|
| Plumpy’nut® | BP-100® | ||
| Body weight (kg) | Sachet | Body weight (kg) | Bars |
| <4 | ⅛–¼ | <5 | ¼–½ |
| 4 up to 10 | ¼–½ | 5 up to 10 | ½–¾ |
| 10 up to 15 | ½–¾ | 10 up to 15 | ¾–1 |
| >15 | ¾–1 | >15 | 1–1½ |
7.4 Assessing for anaemia
There is one very clear way in which you can assess whether a sick child brought to your health post has anaemia, and this is to look for palmar pallor. Palmar pallor is unusual paleness of the skin of the palms. It is a sign of anaemia.
The steps for this are described below.
To see if the child has palmar pallor, look at the skin of the child’s palm. Hold the child’s palm open by grasping it gently from the side as illustrated in Figure 7.5. Do not stretch the fingers backwards. This may cause pallor by blocking the blood supply.

Compare the colour of the child’s palm with your own palm and with the palms of other children. If the skin of the child’s palm is pale, but has some pink areas, the child has some palmar pallor. If the skin of the palm is very pale or so pale that it looks white, the child has severe palmar pallor.
Box 7.1 below summarises the key points you have learned about how to assess for malnutrition and anaemia.
Box 7.1 Summary of assessment steps for malnutrition and anaemia
Malnutrition
Look and feel:
- For children under six months:
- Look for pitting oedema of both feet
- Look for visible severe wasting.
- For children aged six months or more:
- Look for pitting oedema of both feet
- Determine if the MUAC is less than 11.0 cm
- If the MUAC is less than 11.0 cm or there is oedema of both feet and there is no medical complication, you should assess the child’s appetite.
Anaemia
- Look for palmar pallor. If it is present, is it:
- Severe palmar pallor?
- Some palmar pallor?
7.5 Classification of malnutrition and anaemia
You have now seen how to assess the sick child for malnutrition and anaemia. The next step is deciding the classification of the child’s illness based on the presence or absence of specific signs you have identified during the assessment process.
7.5.1 Classification of malnutrition
There are four possible classifications for malnutrition and these are set out below.
Severe complicated malnutrition
A child will be classified as having severe complicated malnutrition in the following cases:
If the child’s age is below six months and the child has
- Visible severe wasting, or
- Oedema of both feet
OR
If the child’s age is six months or above and the child has
- A MUAC less than 11 cm, or
- Oedema of both feet and
- Any medical complication.
Severe uncomplicated malnutrition
A child will be classified as having severe uncomplicated malnutrition in the following cases:
If a child’s age is six months or above and the child has
- A MUAC less than 11 cm, or
- Oedema of both feet and
- No medical complications and
- Passes the appetite test.
Moderate acute malnutrition
A child will be classified as having moderate acute malnutrition in the following cases:
If a child’s age is six months or above and the child has
- A MUAC of 11 cm to less than 12 cm and
- No oedema of both feet.
No acute malnutrition
A child will be classified as having no acute malnutrition in the following cases:
- No visible severe wasting and
- No pitting oedema of both feet and
- Has a MUAC greater than 12 cm.
7.5.2 Classification of anaemia
A child assessed for anaemia will have one of the following three classifications:
- Severe anaemia: when there is severe palmar pallor
- Anaemia: when there is some palmar pallor
- No anaemia: when there is no palmar pallor.
7.5.3 Classification of malnutrition and anaemia using a classification table
Now you have seen that when a sick child is checked for malnutrition and anaemia there will be at least two classifications: one from the four possible classifications of acute malnutrition, and another one from the three possible classifications of anaemia. Table 7.2 summarises the points you have read in this study session and shows you how to assess and classify the sick child for malnutrition and anaemia using the Assess and Classify chart.
Table 7.2 Assess and Classify chart for malnutrition and anaemia.
This study session equipped you with the knowledge and skills to make an accurate assessment of a child suffering with malnutrition and anaemia. You have also looked at how to identify different types of malnutrition and anaemia and to spot the signs or symptoms of these diseases.
Summary of Study Session 7
In Study Session 7, you have learned that:
- The two main types of malnutrition are protein-energy malnutrition and micronutrient deficiency.
- A sign of chronic protein-energy malnutrition is stunting which is shortness of height for the child’s age
- A sign of acute protein energy malnutrition is severe wasting of the body muscles, which is more visible in the shoulders, arms, legs, and the buttocks; or an oedema, which is swelling of the body due to fluid build-up in the tissues.
- To check for oedema, you have to press your thumbs gently for three seconds on the dorsal part (top) of the feet. If after removing your thumb a dent is visible, then the child has pitting oedema.
- A micronutrient deficiency such as a lack of iron in the blood causes a type of anaemia that can result in increased exposure to infections, fatigue, short attention span and poor concentration
- Monitoring weight is crucial in treating malnutrition and anaemia; it enables you to monitor the growth of a child over time and helps you to evaluate the progress of a child who is under nutritional treatment in an outpatient therapeutic programme (OTP) or a supplementary feeding programme. It also helps you to determine the dose of a drug to give a sick child
- It is necessary to do an appetite test when a child is 6 months or more, has a MUAC less than 11cm or has pitting oedema of both feet, and no medical complications.
- It is not necessary to do an appetite test for a child with severe acute malnutrition when the child’s illness requires inpatient care (for example, if the child has pneumonia, persistent diarrhoea, measles, dysentery, malaria, open lesions or vitamin ‘A’ deficiency, or if the child is less than 6 months of age).
Self-Assessment Questions (SAQs) for Study Session 7
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 7.1 (tests Learning Outcomes 7.1, 7.2, 7.4 and 7.5)
A mother asks you what it means when you say a child is malnourished. How would you explain this term?
Answer
You might say that a child is malnourished if he or she is not getting enough nutrients. (You might want to explain what a nutrient is.) This may be because their diet is inadequate or because they are frequently ill. The nutrients they are lacking may be proteins or micronutrients such as vitamin A or iron. (Again, you might want to explain protein and micronutrient.)
SAQ 7.2 (tests Learning Outcomes 7.1, 7.2 and 7.3)
What is the difference between malnutrition and anaemia? What signs would you look for in each case?
Answer
Malnutrition occurs when a person does not get enough nutrients. Anaemia can be caused by a lack of specific nutrients in the diet (as well as by infections or blood loss). And the signs are different. To assess for malnutrition you would look for signs of severe wasting, measure the MUAC, and look for oedema (depending on the age of the child). But you would check for anaemia by looking for palmar pallor.
SAQ 7.3 (tests Learning Outcome 7.1, 7.2, 7.4 and 7.5)
How can you be sure that a child does not have acute malnutrition?
Answer
You can be sure a child is not suffering from acute malnutrition if there is no visible severe wasting, no pitting oedema of the feet, and the MUAC is greater than 12 cm.
