Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Monday, 9 March 2026, 6:21 AM
Integrated Management of Newborn and Childhood Illness Module: 8. Treatment of a Child with Malnutrition and Anaemia
Study Session 8. Treatment of a Child with Malnutrition and Anaemia
Introduction
In the previous study session you learned how to assess and classify a sick child suffering from malnutrition and anaemia. This session is more practice focused and equips you with knowledge and skills that build on what you learned from Study Session 7, so that you will be able to treat and manage severe uncomplicated malnutrition and anaemia. In addition, you will be taught when and how to refer a sick child with uncomplicated malnutrition or anaemia for hospital treatment, and how to give advice to parents/carers of a sick child with one of these conditions.
Learning Outcomes for Study Session 8
When you have studied this session, should be able to:
8.1 Define and use correctly all of the key words printed in bold. (SAQs 8.1, 8.2, and 8.3)
8.2 Correctly treat children with severe uncomplicated malnutrition and anaemia. (SAQs 8.1, and 8.3)
8.3 Correctly identify when to refer children who need referral to the next health care level. (SAQs 8.1, 8.2, and 8.3)
8.4 Give advice to the caregiver of a child with severe uncomplicated malnutrition, moderate acute malnutrition and anaemia. (SAQ 8.2)
8.1 Treatment of a child with malnutrition or anaemia
After assessing and classifying a child with malnutrition or anaemia it is critically important that you treat the child correctly. Identifying and managing the treatment of a malnourished child will help you to promote a healthy life and may even help to save a child’s life.
8.1.1 Treatment of severe complicated malnutrition
![]() A child with severe complicated malnutrition is at risk of death and must always be referred urgently to hospital.
A child with severe complicated malnutrition is at risk of death and must always be referred urgently to hospital.
Children classified as having severe complicated malnutrition are at risk of death from pneumonia, diarrhoea, measles, and other severe diseases. Children with severe complicated malnutrition must always be referred urgently to hospital. They may need special feeding, antibiotics or blood transfusions which cannot be provided at the health post. Before the child leaves for hospital, you should treat the child to prevent low blood sugar. You should also give the child the first dose of vitamin A if you do not identify any oedema, and the child has not received vitamin A in the past six months.
8.1.2 Treatment of severe uncomplicated malnutrition

If a child has severe uncomplicated malnutrition (Figure 8.1), and there is an out-patient therapeutic programme (OTP) service in your health post, then you can manage the child according to the OTP protocol. You will read more about the OTP below. If the service is not available in your health post you should refer the child to a health facility where there is one.
You should give all children with a classification of severe uncomplicated malnutrition the following treatment:
- Vitamin A (unless there is presence of oedema or they have already received vitamin A in the past six months)
- Amoxicillin for seven days
- A dose of folic acid 5 mg
- Ready-to- use therapeutic food (RUTF) such as Plumpy’nut® or BP-100®.
If the child is aged two years or above, you should also give mebendazole or albendazole, preferably at the second out-patient visit which should take place seven days after the first visit to your health post. You will need to advise the mother that she should return for a follow-up visit within seven days, so that you can see whether the child has made progress.
8.1.3 Treatment of moderate acute malnutrition
A child classified as having moderate acute malnutrition has a higher risk of severe disease. You would need to assess the child’s feeding and counsel the mother about the best way to feed her child (you can find the recommendations for feeding children in the Food Box on the Counsel the Mother chart in your chart booklet).
If there is a supplementary feeding programme in your area you should refer the child to this. You should advise the mother that she should come back to the health post with the child for a follow-up visit after 30 days.
8.1.4 Treatment when there is no moderate acute malnutrition
If the child is below two years of age, you should assess for feeding and then counsel the mother about feeding her child. There is more information about this in the Nutrition Module. (You can also look at the recommendations in the Food Box on the Counsel the Mother chart in your chart booklet.) Children below two years of age have a higher risk of feeding problems and malnutrition than older children.
8.1.5 Treatment of severe anaemia
![]() Children who have severe anaemia must be referred urgently to hospital.
Children who have severe anaemia must be referred urgently to hospital.
Children classified as having severe anaemia are at risk of death from congestive heart failure, hypoxia (acute shortage of oxygen in the blood), or severe bacterial infections. All children with severe anaemia must be referred urgently to hospital. They may need blood transfusions or antibiotics. You need to explain to the mother the reasons for and the advantages of the child going to the hospital and do everything you can to facilitate the referral. Look back at Study Session 4 in this Module if you need reminding how to refer a child to hospital.
8.1.6 Treatment of anaemia
A child with some palmar pallor (which you read about in the previous study session) may have anaemia and should be given iron (see Table 8.1 below). When there is a high risk of malaria, an antimalarial drug should also be given to a child with signs of anaemia. A child should also receive treatment for hookworm and whipworm where these infections are common.
| Give one dose daily for 14 days | ||
|---|---|---|
| AGE or WEIGHT | IRON TABLET Ferrous sulphate 300 mg (60 mg elemental iron) | IRON SYRUP Ferrous fumarate 100 mg per 5 ml (20 mg elemental iron per ml) |
| 2 months up to 4 months (4‒6 kg) | 1.00 ml (15 drops) | |
| 4 months up to 12 months (6‒10 kg) | 1.25 ml (20 drops) | |
| 12 months up to 3 years (10‒14 kg) | ½ tablet | 2.00 ml (30 drops) |
| 3 years up to 5 years (14‒19 kg) | ½ tablet | 2.5 ml (35 drops) |
8.1.7 Treatment when there is no anaemia
There is no specific action or additional treatment that you need to give the child for this classification. Reassure the mother and praise her for good care of the child.
8.2 The out-patient therapeutic programme (OTP)
An OTP is a programme that provides home-based treatment and rehabilitation for children with severe uncomplicated malnutrition. These children can be admitted directly into an OTP, treated with routine drugs, and as you read in the previous study session, given ready-to-use therapeutic food (RUTF) to eat at home. The children attend the OTP every week for a medical check-up, receive additional medical treatments if required and are given a one-week supply of RUTF. Box 8.1 below describes RUTF.
Box 8.1 Ready-to-use food (RUTF)
RUTF is therapeutic food that can be consumed easily by children straight from the packet or pot without any cooking. It is a high-energy, nutrient-dense food. It is easy to use and store. It can be kept in simple packaging for several months without refrigeration. It can be kept for several days even when opened.
BP-100® and Plumpy’nut® are the commonly known RUTF preparations. If you have both products available, you should give children under two years of age either Plumpy’nut, or crush BP-100 and make this into porridge for the child. Children above the age of two years can take the BP-100 biscuit and you may not need to make porridge. The amount of RUTF that should be given to severely malnourished children is based on their weight as indicated in Table 8.2 below.
| Class of weight (kg) | PLUMPY’NUT® | BP-100® | ||
|---|---|---|---|---|
| sachet per day | sachet per week | bars per day | bars per week | |
| 3.0–3.4 | 1¼ | 9 | 2 | 14 |
| 3.5–4.9 | 1½ | 11 | 2½ | 18 |
| 5.0–6.9 | 2 | 14 | 4 | 28 |
| 7.0–9.9 | 3 | 21 | 5 | 35 |
| 10.0‒14.9 | 4 | 28 | 7 | 49 |
| 15.0–19.9 | 5 | 35 | 9 | 63 |
Box 8.2 below summarises the key messages for mothers and caregivers of children admitted to an OTP.
Box 8.2 Key messages for caregivers of children in OTP
- RUTF is a food and medicine for malnourished children only. It should not be shared.
- For breastfed children, breastmilk should always be given before the RUTF and on demand.
- RUTF should be given before other foods. The child should have small regular meals of RUTF and be encouraged to eat often, every three to four hours.
- Plenty of clean water to drink should always be offered to the child when he or she is eating RUTF.
- The caregiver should wash their hands with soap and water before feeding the child.
- Food must be kept clean and covered.
- A sick child gets cold quickly so should be kept covered and warm.
A child with severe uncomplicated malnutrition should also receive routine drugs. These drugs are very important for the child to recover quickly. Table 8.3 sets out what routine medicines should be given to severely malnourished children and the correct dosage according to their age and previous treatment history.
| Drug | Treatment |
|---|---|
| Vitamin A | 1 dose at admission for all children except those with oedema or those who received vitamin A in the past six months |
| Folic acid | 1 dose at admission |
| Amoxicillin | 1 dose at admission + give treatment for seven days to take home. The first dose should be given in the presence of the supervisor |
| Deworming | 1 dose on the second week (second visit) |
Measles vaccine (from nine months old) | 1 vaccine dose on the fourth week (fourth visit) |
The following four tables refer specifically to vitamin A, folic acid and Amoxicillin and show what dose should be given to severely malnourished children and when.
| Age in months | Vitamin A IU orally |
|---|---|
| 6–11 | One blue capsule (100,000 IU) |
| 12 (or 8 kg) and more | Two blue capsules (200,000 IU) |
| When | Amount |
|---|---|
At admission | 5 mg |
| Weight in kg | Dosage twice per day | 250 mg capsule/tablet |
|---|---|---|
| <5 kg | 125 mg | ½ |
| 5‒10 | 250 mg | 1 |
| 10‒20 | 500 mg | 2 |
| 20‒35 | 750 mg | 3 |
| >35 | 1000 mg | 4 |
| Age up to 2 years | |
|---|---|
| Albendazole 400 mg | 1 tablet once |
| Mebendazole 100 mg | 5 tablets once |
8.3 Follow-up care of the child with malnutrition and anaemia
In this section you are going to look about what you need to do at a follow-up visit for a child who has been in the Outpatient Therapeutic Programme (OTP) for severe malnutrition or who has been assessed as having anaemia.

8.3.1 Follow-up care for severe malnutrition
Follow-up care for a child assessed as having severe malnutrition is an important part of the OTP and the mother or caregiver should be advised to come to the health post every week for two months, so that follow-up care can be provided.
You should remember that the mother or caregiver may be feeling very anxious about her child’s health. Ask questions and praise the mother when she tells you about the positive things she is doing to help the child. You can base your assessment of the child’s progress on a number of signs and these are set out in Box 8.3 below.
Box 8.3 Checklist for follow-up of a child with severe uncomplicated malnutrition
Follow-up should be done every seven days for at least two months as follows:
Ask about
- Diarrhoea, vomiting, fever or any other new complaint or problem
- Whether the child is finishing their weekly RUTF ration.
Check for
- Complications
- Temperature, respiration rate
- Weight, MUAC and oedema
- Appetite (do the appetite test).
Decide on action
Refer if there is any one of the following:
- Development of any new complication
- Failed appetite test
- Increase/development of oedema
- Weight loss for two consecutive visits
- Failure to gain weight for three consecutive visits
- Major illness or death of the main caregiver so that the child can’t be managed at home.
If there is no indication for referral, give:
- De-worming and measles vaccination
- Weekly ration of Plumpy’nut® or BP-100®
- Appointment for next follow-up and record the information on the OTP card.
If the child is absent for any follow-up visit:
- Ask the community volunteer to do a home visit and report back to you as the Health Extension Practitioner.
Discharge
A child stays in the programme until they meets the discharge criteria or have been in the programme for a maximum of two months. The discharge criteria depend on the admission criteria.
- For those who were admitted based on oedema: discharge if there is no oedema for two consecutive visits (14 days)
- For those who were admitted without oedema: discharge when the child reaches the discharge target weight (as indicated in your chart booklet).
The child who fails to reach the discharge criteria after two months of OTP treatment, must always be referred to a hospital.
On discharge make sure:
- Counselling on child feeding and care is given to the mother or caregiver
- A discharge certificate is given to the mother or caregiver and referral to the Supplementary Feeding Programme is made (whenever one is available)
- A child is registered appropriately in the registration book on date of discharge.
8.3.2 Follow-up care for moderate acute malnutrition
If a child was classified with moderate acute malnutrition and referred to a supplementary feeding centre, or the mother has been given counselling to help her improve feeding and care of her child, she should be advised to return for a follow-up visit after 30 days. If there was a feeding problem as judged by the feeding recommendations in your chart booklet, the mother should be advised to return with the child earlier than 30 days.
You may have specially scheduled sessions for nutritional counselling, and mothers with a malnourished child can be asked to come for a follow-up visit at this time. A special session allows you to devote the necessary time to discuss feeding with several mothers and perhaps demonstrate some good foods for young children.
When the mother attends your health post for a follow-up visit after 30 days for a child with moderate acute malnutrition, you should take the steps set out in Box 8.4. As you read above, you should praise the mother and encourage her to continue good home care for her child. This will ensure that she feels supported by you.
Box 8.4 Follow-up care for moderate acute malnutrition
After 30 days
- Measure the child’s MUAC and determine if the child still has moderate acute malnutrition
- Reassess feeding.
Treatment
- If the child no longer has moderate acute malnutrition, praise the mother and encourage her to continue her good care of the child
- If the child still has moderate acute malnutrition, counsel the mother about any feeding problems you have identified. Ask the mother to return again in one month. Continue to see the child monthly until the child is feeding well and no longer has moderate acute malnutrition.
Exception
A child for whom you do not think that feeding will improve, or whose MUAC is not improving, must always be referred to a health centre or hospital for better management.
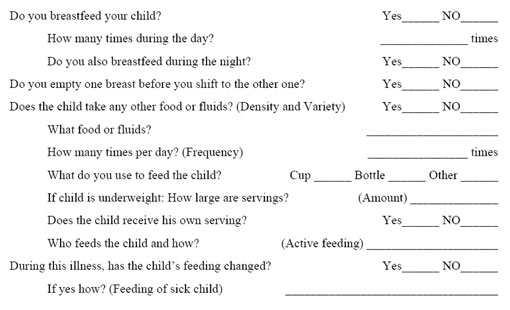
Box 8.5 below sets out the steps you need to follow to assess the child’s feeding. It will help you judge what advice and support you can give the mother or caregiver of the child.
Box 8.5 Checklist for feeding assessment
Assess the child’s feeding
Ask questions about the child’s usual feeding behaviour. Compare the mother’s answers against the feeding recommendation for the child’s age.
8.3.3 Follow-up care for anaemia
When a child who had palmar pallor returns for a follow-up visit after 14 days, you should take the steps set out in Box 8.6 below.
Box 8.6 Follow-up care for a child with anaemia
After 14 days:
- Reassess feeding
- Give the child iron and advise the mother to return to your health post in 14 days for more iron
- Continue giving iron to the child every 14 days for two months
- If the child has palmar pallor after two months, refer for assessment.
You have now covered all the important points that deal with proper management of a child with malnutrition and anaemia. Some of the points, such as assessing, feeding and counselling the mother on proper feeding practices, together with specific feeding recommendations, will be dealt with in more detail later in this Module, and are also covered in the Nutrition Module.
Summary of Study Session 8
In Study Session 8, you have learned that:
- Children classified as having severe uncomplicated malnutrition are at risk of death from pneumonias, diarrhoea, measles and other serious diseases. They must be referred urgently to a hospital because they may need specialist care or treatment that cannot be provided at the health post.
- Children classified as having severe anaemia are at risk of death from heart failure, hypoxia or bacterial infection and must be referred urgently to hospital.
- Children classified as having severe uncomplicated malnutrition can be treated at the health post using the OTP service and treatment protocol.
- Children classified as having moderate acute malnutrition have a higher risk of serious diseases. You should address the child’s feeding pattern and advise the parent or caregiver the best way to feed the child.
- Children with some palmar pallor may have anaemia and should be given iron.
- RUTF is a food and medicine for malnourished children only and should not be shared.
- Follow-up care for a child with uncomplicated malnutrition should include a visit to the health post every seven days for two months.
- A child with moderate acute malnutrition should be referred to a complementary feeding centre and the parent or caregiver should be given counselling to help improve the feeding and care of the child.
- Follow-up care for a child with anaemia includes a visit the clinic every 14 days.
Self-Assessment Questions (SAQs) for Study Session 8
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the questions below. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
Read Case Study 8.1 and then answer the questions that follow.
Case Study 8.1 for SAQ 8.1
Negash is a 13-month-old child presenting to the health post with cough. The Health Extension Practitioner assessed him and found the following signs: pitting oedema of both feet; MUAC was 12.5 cm; some palmar pallor. The HEP also identified fast breathing and classified Negash as having pneumonia.
SAQ 8.1 (tests Learning Outcomes 8.1, 8.2 and 8.3)
- a.Describe how you would classify Negash’s type of nutritional problem and explain what you would do to manage him.
- b.Write down what you think might be the concerns of Negash’s mother and two or three things you could say or do to advise and reassure her.
Answer
- a.Negash has severe complicated malnutrition as he has pitting oedema of both feet and a complicating illness — pneumonia. The first thing you would need to do is give Negash a first dose of amoxicillin, or cotrimoxazole if there is no amoxicillin. You would then need to refer him urgently to the health facility with in-patient care. Because Negash has pneumonia you do not need to carry out an appetite test.
- b.Negash’s mother is likely to be very anxious and reluctant to go to hospital. Explain to her that the necessary drugs and care to help her child recover from his health problems are available in a hospital. Tell her that you will give her a referral note that will explain Negash’s problems and that the hospital will give Negash the necessary care.
Read Case Study 8.2 and then answer the questions that follow.
Case Study 8.2 for SAQ 8.2
Jemal is a 22-month-old boy and weighs 6.5 kg. His mother has brought him because he has had swollen feet for three days. When you assessed Jemal, you found pitting oedema of the feet, MUAC of 10 cm, no palmar pallor and no other problems. Jemal passed an appetite test. You are in a facility where there is an OTP, and there is an SFP in your kebele.
SAQ 8.2 (tests Learning Outcomes 8.1, 8.3 and 8.4)
- a.Describe how you would classify Jemal’s illness.
- b.Describe the management you are going to give him.
Answer
- a.In your answer you would have classified Jemal’s nutritional status as severe uncomplicated malnutrition. This is the correct classification for a child aged six months and above, with either pitting oedema of the feet or MUAC less than 11 cm, and no medical complication, and who passes an appetite test.
- b.You would admit Jemal to the OTP and manage him using the standard OTP protocol. You need to advise the mother to return immediately if the child’s condition worsens.
SAQ 8.3 (tests Learning Outcomes 8.1, 8.2, 8.3 and 8.4)
What are the advantages of having an OTP in your area?
Answer
The advantage of an OTP is that a child with severe uncomplicated malnutrition can be treated without having to go to hospital. They can be given the appropriate drugs and also therapeutic food to eat at home. They will also receive follow-up care.