Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Monday, 3 November 2025, 9:01 AM
Integrated Management of Newborn and Childhood Illness Module 10. Infant and Young Child Feeding
Study Session 10: Infant and Young Child Feeding
Introduction
Adequate feeding is essential for growth and development. Poor feeding during infancy can have a lifelong effect. Therefore one of the important tasks you have as a Health Extension Practitioner is to assess a young infant’s feeding and weight so that feeding can be improved if necessary.
The best way to feed a young infant is for the mother to breastfeed exclusively. Exclusive breastfeeding means that the infant takes only breastmilk, and has no additional food, water or other fluids (medicines and vitamins are exceptions) for the first six months of life.
Exclusive breastfeeding gives a young infant the best nutrition and protection from disease possible. If mothers understand that exclusive breastfeeding gives the best chances of good growth and development, they may be more willing and motivated to breastfeed. As a Health Extension Practitioner you can help the mother to understand this, encourage her to breastfeed her infant and overcome any difficulties she might be experiencing.
In this study session you will learn how to assess feeding problems, in particular in relation to breastfeeding, and how to support the mother so she can breastfeed her infant as effectively as possible. You will look at feeding recommendations for infants and young children in a range of age groups and how to counsel the mother to feed her child both during illness and when the child is well.
Learning Outcomes for Study Session 10
When you have studied this session, you should be able to:
10.1 Define and use correctly all of the key words printed in bold. (SAQs 10.1 and 10.2)
10.2 Assess feeding problems in infants and young children, and determine weight for age. (SAQs 10.1 and 10.2)
10.3 Assess breastfeeding. (SAQs 10.1 and 10.2)
10.4 List signs of correct positioning and attachment for optimum breastfeeding. (SAQ 10.2)
10.1 Assessing feeding problems
Assessing feeding problems in infants and children is a two-stage process. First, there are some important questions that you need to ask the mother. Remember that she may be feeling anxious about her baby’s feeding, so you should try asking questions in different ways if you feel that you are not getting the information you need to be able to complete your assessment. You should ask the mother if she is having difficulty feeding the infant, what the young infant is fed and how often. Secondly, you need to assess if the infant has any problems with breastfeeding or if the infant is low weight for their age (underweight).
Table 10.1 below sets out the questions you should ask the mother.
| Ask | Look, listen, feel: |
|---|---|
● Is there any difficulty feeding? ● Is the infant breastfed? If yes: ◦ How many times in 24 hours? ◦ Do you empty one breast before switching to the other? ◦ Do you increase frequency of breastfeeding during illness? ◦ Does the infant receive any other foods or drinks? If yes, how often? ◦ What do you use to feed the infant? |
●Determine weight for age |
ASK: Is there any difficulty feeding?
Any difficulty mentioned by the mother is important. She may need counselling or specific help with a difficulty and as a Health Extension Practitioner you have an important role to play in helping the mother overcome any problems she is experiencing. For example, the mother may mention difficulties in breastfeeding. These may include that her infant feeds too frequently, or not frequently enough; that she does not have enough milk; that her nipples are sore; that she has flat or inverted nipples; or that the infant does not want to take the breast.
![]() An infant who can’t feed may have a life-threatening problem. Refer urgently to hospital.
An infant who can’t feed may have a life-threatening problem. Refer urgently to hospital.
If a mother says that the infant is not able to feed, you should assess breastfeeding or watch her try to feed the infant with a cup to see what she means by this. An infant who is not able to feed may have a serious infection or other life-threatening problem and should be referred urgently to hospital.
ASK: Is the infant breastfed? If yes, how many times in 24 hours?
Young infants should be breastfed as often and for as long as the infant wants, day and night. This should be eight or more times in 24 hours.
ASK: Does the infant receive any other foods or drinks? If yes, how often?
A young infant should be exclusively breastfed. Find out if the young infant is receiving any other foods or drinks such as other milk, juice, tea, thin porridge, dilute cereal, or even water. Ask the mother how often the infant receives it and the amount that the infant is eating. You need to know if the infant is mostly breastfed, or mostly fed on other foods.
ASK: What do you use to feed the infant?
If an infant takes other foods or drinks, find out if the mother uses a feeding bottle, cup or something similar to give her infant food and drink.
LOOK: Determine weight for age
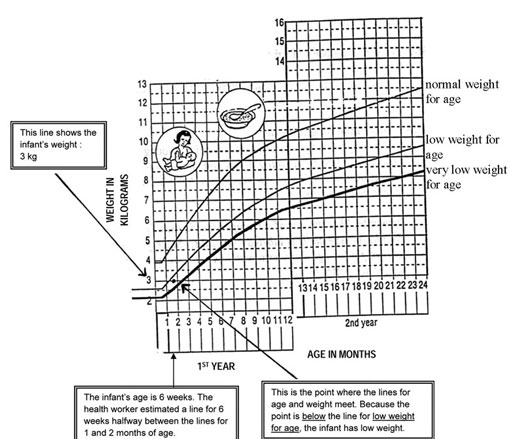
Use a weight for age chart to determine if the young infant is low weight for age. Notice that for a young infant you should use the low weight for age (underweight) line, instead of the very low weight for age (severely underweight) line, which is used for older infants and children. You decide low weight for age in young infants and very low weight for age in older infants and children in the following ways.
To determine weight for age:
- For young infants calculate their age in weeks; for older infants and children you should calculate their age in months.
- Weigh the infant/child if they have not already been weighed today. Use a scale that you know gives accurate measurements. The infant/child should wear light clothing when they are weighed. You should ask the mother to help remove any coat, sweater, or shoes.
- Use the weight for age chart to determine the child’s weight for age (see Figure 10.1).
- Look at the left-hand axis to locate the line that shows the infant’s/child’s weight.
- Look at the bottom axis of the chart to locate the line that shows the infant’s/child’s age in weeks or months.
- Find the point on the chart where the line for the infant’s/child’s weight meets the line for the infant’s/child’s age.
- Decide where the point is situated.
In young infants, if the point is situated below the low weight for age line then the infant has low weight. If the point is above or on the low weight curve then the young infant is not low weight for age.
Example: A young infant is six weeks old and weighs 3 kg. Figure 10.1 shows you how the Health Extension Practitioner checked if the infant was low weight for age.
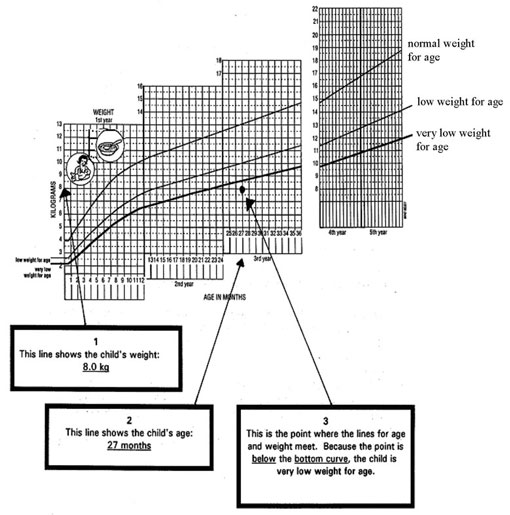
In older infants and children, if the point is below the line for very low weight (below the bottom curve) then the child has very low weight for age. If the point is above or on the bottom curve, the child is not very low weight for age.
Example: Look at Figure 10.2. This is a chart for a child who is 27 months old and weighs 8.0 kilograms. Look at how the Health Extension Practitioner determined the child’s weight for age.
-
What is the best way to get information from the mother about her child’s feeding?
-
You should ask the mother questions to find out whether the child is feeding easily and, if under six months, whether breastfed exclusively. The mother may be feeling anxious about her child, so you should ask questions in a way she understands. This might mean you have to ask for the information you need in different ways. You should ensure she feels you are being supportive, rather than critical.
10.2 Assess breastfeeding
Not all infants need to be assessed for breastfeeding. For example, you will not need to do a breastfeeding assessment in the following cases:
- If the infant is exclusively breastfed without difficulty and is not low weight for age
- If the infant is not breastfed at all
- If the infant has a serious problem requiring urgent referral to a hospital.
In these situations, classify how the infant is feeding based on the information that you have already obtained.
If the mother’s answers to your questions about breastfeeding indicate a difficulty, or if the infant is low weight for age, you should observe a breastfeed (how you do this is described below). Low weight for age in an infant is often due to low birth weight. Low birth weight infants are likely to have a problem with breastfeeding.
You should assess breastfeeding in the following circumstances:
If the infant:
- Has any difficulty feeding
- Is breastfeeding less than eight times in 24 hours
- Is taking any other foods or drinks
- Is low weight for age.
And/or the mother is:
- Switching the breast frequently without emptying one breast first, and
- Has not increased feeding if the infant is ill.
You should not try to assess breastfeeding if the infant needs to be referred urgently.
However, if the infant has any need for urgent referral then you should not try to assess breastfeeding. In this situation, you should just refer the infant.
10.2.1 Assessing breastfeeding

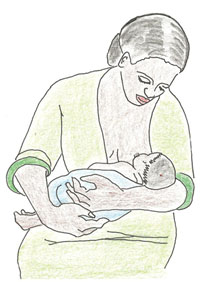
Assessing breastfeeding requires careful observation (Figure 10.3). Ask the mother when she last fed her infant and then, when the infant is ready to feed again, you should help the mother to feel relaxed and comfortable.
ASK: Has the infant breastfed in the previous hour?
If the infant has already been fed in the last hour, ask the mother to wait and tell you when the infant is willing to feed again. In the meantime, complete the assessment by checking the infant’s immunization status. You may also decide to begin any treatment that the infant needs, such as giving an antibiotic for local bacterial infection or ORS solution for some dehydration.
If the infant has not fed in the previous hour, he or she may be willing to breastfeed. Ask the mother to put her infant to the breast. Observe a whole breastfeed if possible, or observe for at least four minutes.
Sit quietly and watch the infant breastfeed.
LOOK: Is the infant well positioned?
The four signs of good positioning are:
- The infant’s body is straight
- The infant’s head and body are facing the breast
- The infant’s body is close to the mother’s
- The mother is supporting the infant’s whole body.

LOOK: Is the infant able to attach?
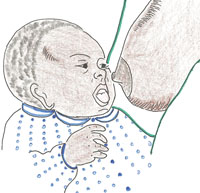
The four signs of good attachment (see Figure 10.4) are:
- The infant’s chin is touching the breast (or is very close)
- The infant’s mouth is wide open
- The lower lip is turned outward
- More areola is visible above than below the infant’s mouth (the areola is the dark area of the breast around the nipple).
If all of these four signs are present, the infant has good attachment. This is also illustrated in Figure 10.5.

If attachment is not good (see Figure 10.6), you may see:
- The infant’s chin is not touching the breast
- The mouth is not wide open with the lips pushed forward
- The lower lip is turned in, or
- More areola (or an equal amount) is visible below the infant’s mouth than above it.
If you see any of these signs of poor attachment, the infant is not well attached. This is also illustrated in Figure 10.7.

If a very sick infant cannot take the nipple into his mouth and keep it there to suck, he has no attachment at all. He is not able to breastfeed at all.
You can support a breastfeeding mother to overcome attachment problems.
If an infant is not well attached, the results may be pain and damage to the mother’s nipples. Or the infant may not remove breastmilk effectively, which may cause engorgement (swelling) of the breast. The infant may be unsatisfied after breastfeeds and want to feed very often or for a very long time. The infant may get too little milk and not gain weight, or the breastmilk may dry up. All these problems may improve if attachment can be improved.
LOOK: Is the infant suckling effectively?
The infant is suckling effectively if he suckles with slow deep sucks and sometimes pauses. You may see or hear the infant swallowing. If you can observe how the breastfeed finishes, look for signs that the infant is satisfied. If satisfied, the infant releases the breast spontaneously (that is, the mother does not cause the infant to stop breastfeeding in any way). The infant appears relaxed, sleepy, and loses interest in the breast.
An infant is not suckling effectively if he is taking only rapid, shallow sucks. You may also see in-drawing (inward movement) of the cheeks. You do not see or hear swallowing. The infant is not satisfied at the end of the feed, and may be restless. He may cry or try to suckle again, or continue to breastfeed for a long time.
An infant who is not suckling at all is not able to suck breastmilk into his mouth and swallow. Therefore, he is not able to breastfeed at all.
If a blocked nose seems to interfere with breastfeeding, you should clear the infant’s nose. Then check again whether the infant can suckle more effectively.
LOOK for ulcers or white patches in the mouth (thrush)
Look inside the mouth at the tongue and inside of the cheek. Thrush looks like milk curds on the inside of the cheek, or a thick white coating of the tongue. Try to wipe the white off and look to see if this leaves bleeding spots or a raw area.
-
What are the signs of good attachment?
-
There are four ways that you can tell if an infant is attached well during a breastfeed. The infant’s chin should either touch or be very close to the mother’s breast and the infant’s mouth should be wide open, with the lower lip turned outwards. You should see if there is more areola visible above than below the mouth. If the infant’s body is twisted away from the mother, there is unlikely to be good attachment.
10.3 Teach correct positioning and attachment for breastfeeding
You are now going to look at reasons for poor attachment and ineffective suckling and learn how you can help a mother position and attach her infant better during feeding.
10.3.1 Reasons for poor attachment and ineffective suckling
There are several reasons that an infant may be poorly attached or not able to suckle effectively. He may have had bottle feeds, especially in the first few days after delivery. His mother may be inexperienced. She may have had some difficulty and nobody to help or advise her. For example, perhaps the infant was small and weak, the mother’s nipples were flat or there was a delay starting to breastfeed.
The infant may be poorly positioned at the breast. As you read above, correct positioning is important because poor positioning often results in poor attachment, especially in younger infants. If the infant is positioned well, the attachment is likely to be good.
10.3.2 Improving positioning and attachment
If in your assessment of breastfeeding you found any difficulty with attachment or suckling, you can help the mother position and attach her infant better. Make sure that the mother is comfortable and relaxed, for example, sitting on a low seat with her back straight. Then follow the steps in Box 10.1.
Box 10.1 Teach correct positioning and attachment for breastfeeding
- Show the mother how to hold/position her infant:
- with the infant’s head and body straight
- facing her breast, with the infant’s nose opposite her nipple
- with the infant’s body close to her body
- supporting the infant’s whole body, not just the neck, shoulder and head.
- Show the mother how to help the infant to attach. She should:
- touch her infant’s lips with her nipple
- wait until her infant’s mouth is opening wide (see Figure 10.8)
- move her infant quickly onto her breast, aiming the infant’s lower lip well below the nipple.
- Look for signs of good attachment and effective suckling. If the attachment or suckling is not good, ask the mother to try again.
Always observe a mother breastfeeding before you help her, so that you understand her situation clearly. Do not rush to make her do something different. If you see that the mother needs help, first say something encouraging, like:
‘She really wants your breastmilk, doesn’t she?’
Then explain what might help and ask if she would like you to show her. For example, say something like:
‘Breastfeeding might be more comfortable for you if your baby took a larger mouthful of breast. Would you like me to show you how?’
If she agrees, you can start to help her.
As you show the mother how to position and attach the infant, be careful not to take over from her. Explain and demonstrate what you want her to do. Then let the mother position and attach the infant herself.
Then look for signs of good attachment and effective suckling again (see Figure 10.8). If the attachment or suckling is not good, ask the mother to remove the infant from her breast and to try again. When the infant is suckling well, explain to the mother that it is important to breastfeed long enough at each feed, and to empty one breast before switching to the other. She should not stop the breastfeeding before the infant wants to stop.
10.3.3 Counselling about other feeding problems
Exclusive breastfeeding in the first six months is optimum for the infant’s health and development.
If a mother is breastfeeding her infant less than eight times in 24 hours, you should advise her to increase the frequency of breastfeeding. Breastfeed as often and for as long as the infant wants, day and night.
If the infant receives other foods or drinks, you should counsel the mother about breastfeeding her infant more frequently, reducing the amount of the other foods or drinks she gives her infant, and if possible, stopping giving alternatives altogether. If she does continue to provide other foods and drinks then you should advise her that any other drinks should be given from a cup, and not from a feeding bottle.
Tell the mother that she should come back for a follow-up visit in two days if the infant continues to have a feeding problem. This is especially important if you are recommending a significant change in the way the infant has been fed up until now.
-
What advice on feeding would you give to the mother of a three-month-old infant?
-
First you would advise and encourage the mother that she should breastfeed her infant exclusively and not give the infant any other foods for another three months. You would also explain to her that if the infant becomes unwell she should increase the frequency of breastfeeding during the illness.
10.4 Classify feeding
When you have watched a breastfeed and classified any problems the infant is experiencing, you need to help the mother by giving her clear advice on how to improve feeding. You also need to give her information about caring for the infant if there are problems such as thrush, or if the baby is underweight.
You can compare an infant’s signs with those listed in Table 10.2. This sets out the appropriate classifications and the recommended advice that you should give to the mother.
Feeding problem |
Classification |
Recommended advice |
|---|---|---|
If any one of the following signs:
|
FEEDING PROBLEM OR LOW WEIGHT |
Advise the mother to breastfeed as often and for as long as the infant wants, day and night.
|
Not low weight for age and no other signs of inadequate feeding |
NO FEEDING PROBLEM | Advise the mother to give home care for the young infant. Praise the mother for feeding the infant well. |
10.4.1 Feeding problems or low weight (underweight)
Infants who are underweight (low weight for age), or who have some sign that their feeding needs improvement, are likely to have more than one of the feeding problems set out in Table 10.2.
10.4.2 No feeding problems
An infant in this classification is exclusively and frequently breastfed and the infant’s weight for age is not below the line for ‘underweight’. It is not necessarily normal or a good weight for the infant’s age, but the infant is not in the high risk category that you are most concerned with.
In this study session you have learned that it is important to obtain as much information as possible about how the infant is feeding. You learned that you can do this by asking the mother different questions and by observing breastfeeding. You also learned how to assess whether a young infant is low weight or, in older infants and children, whether they are very low weight for age. As a Health Extension Practitioner, you can provide a lot of support to encourage a mother and help her to overcome any difficulties she may be experiencing in feeding her infant. In the next study session you will look at recommendations you can give a mother for feeding her infant and children in ways that are appropriate to their age and needs.
Summary of Study Session 10
In Study Session 10, you have learned that:
- There are key questions to ask and signs to look for in the assessment of an infant and a child for feeding problems.
- You should do a feeding assessment if an infant has any difficulties feeding, is fed less than eight times in 24 hours, receives other food or is low weight for age.
- Examples of feeding problems include poor attachment or positioning, poor suckling, and thrush.
- You can support a mother by helping her position her infant correctly and counselling her on the best feeding practices for her age.
- There are some simple recommendations you can make to help a mother overcome problems associated with breastfeeding.
Self-Assessment Questions (SAQs) for Study Session 10
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 10.1 (tests Learning Outcomes 10.1, 10.2 and 10.3)
- a.What steps would you take to assess feeding problems for a three-month-old infant?
- b.What advice would you give the infant’s mother?
Answer
- a.First you need to ask the infant’s mother questions that will give you as much information as possible to find out if the mother has any difficulty feeding her infant. You should ask her the following questions:
- Is the infant breastfeeding? If yes, how often?
- Do you empty one breast before switching to the other?
- Do you increase the frequency of breastfeeding when the infant is sick?
- Is the infant being given any other foods or drinks? If so, what do you use to feed the infant?
Then assess whether the infant is low weight or not. If you identify any feeding problem then you should observe the mother while breastfeeding her infant to check for good positioning and attachment and to see if the infant is suckling effectively.
b.It is important that an infant of three months is exclusively breastfed. Praise the mother if she is already doing this. If she is giving the infant other foods, for example, thin gruel, you should advise her that this is not a good replacement for breastmilk.
You should also advise the mother to switch to the other breast during a feed, but ensure that one breast is completely emptied before switching to the other. This will ensure the infant receives the rich breastmilk (hind milk). Finally, you would advise her that when her infant is ill, increasing breastfeeding during and after illness will help the infant maintain weight and prevent malnutrition.
SAQ 10.2 (tests Learning Outcomes 10.1, 10.2, 10.3 and 10.4)
What are the different ways in which you can encourage and support a mother to breastfeed her infant as effectively as possible?
Answer
One of the ways you can advise and support a breastfeeding mother is to teach her correct positioning and attachment. You would also explain to her that if the infant is suckling well, it is important to breastfeed long enough at each feed. Through careful observation of a breastfeeding session, you can identify any problems and then help the mother in positioning her infant in a way that will facilitate attachment. Making encouraging statements, as well as suggestions to improve feeding, is very important for the mother to feel confident.