Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Saturday, 11 May 2024, 1:03 AM
Integrated Management of Newborn and Childhood Illness Module: 12. Immunization and Related Interventions
Study Session 12 Immunization and Related Interventions
Introduction
Full details of the vaccines in the EPI, their cold storage, stock control and organisation of vaccination campaigns and routine clinics are given in the Immunization Module.
In this study session, you will learn about the types of vaccines routinely given in the Expanded Programme of Immunization (EPI) and the schedule of their administration. Immunization is known as the single most cost-effective strategy to decrease childhood morbidity and mortality. The objective of the EPI is to reduce and control illness, death and disability among children caused by vaccine-preventable diseases. You will also learn about the routine administration of vitamin A and deworming of children.
Learning Outcomes for Study Session 12
When you have studied this session, you should be able to:
12.1 Define and use correctly all of the key words printed in bold. (SAQs 12.1 and 12.3)
12.2 Describe the type of vaccines covered under the EPI and their schedule of administration. (SAQs 12.1 and 12.2)
12.3 Describe how to check for immunization status and when the child needs immunizing. (SAQs 12.1, 12.2 and 12.3)
12.4 List the contraindications to vaccine administration. (SAQs 12.1 and 12.2)
12.5 Describe the schedule of vitamin A administration and deworming for children. (SAQ 12.3)
12.1 The Expanded Programme of Immunization
In this study session you are going to look at the vaccines covered in the Expanded Programme of Immunization (EPI) and their schedule of administration. You will then go on to learn how to check a child’s immunization status and understand when it is necessary to provide a child with a vaccine on the same day of the visit. You should be aware that the terms ‘immunization’ and ‘vaccination’ can be used interchangeably, so you will see both terms used in this study session.
Every child should complete his or her full vaccination before the age of one year.
Ideally, every child must complete his or her full vaccination before celebrating their first birthday. Therefore you must check every child when you meet them in their home or at the health post. You need to check whether they have been vaccinated against the EPI diseases and if not, you should give any missed vaccinations on the same day of the visit.
12.2 Vaccines covered under EPI and their schedule of administration
Currently, the EPI delivers eight vaccines to protect children against the following serious childhood illnesses: tuberculosis, poliomyelitis, diphtheria, pertussis, tetanus, Haemophilus influenzae-B (Hib) infections, hepatitis B disease and measles.
- Haemophilus influenzae type B and the hepatitis B vaccines are new vaccines introduced into the EPI programme in Ethiopia in 2007.
- Haemophilus influenzae type B vaccine prevents meningitis, pneumonia, epiglottitis and other serious infections caused by Haemophilus influenzae type B bacteria. The vaccine will not protect against these conditions if they are caused by other infectious agents such as viruses.
- Hepatitis B vaccine protects against liver disease. Hepatitis B infection in young children is usually asymptomatic (they don’t develop symptoms). However, a larger proportion of children than adults may become chronic carriers who can transmit the hepatitis B virus to others for many years without showing symptoms themselves. Chronic carriers are more likely to develop severe chronic liver disease or liver cancer in later life.
Table 12.1 shows the recommended immunization schedule and the mode of administration of the eight childhood vaccines. The recommended vaccine should be given when the child reaches the appropriate age for each dose. If the vaccination is given too early, protection may not be adequate. If there is any delay in giving the appropriate vaccine, this will increase the risk of the child getting the disease. If you see a child who has not been immunized at the recommended age, you should give the necessary immunizations as soon as possible. Most vaccines (except BCG and measles) require administration of repeated doses, usually three times. For these vaccines, after the first dose, give the remaining doses at least four weeks apart.
| Age of vaccination | Type of vaccination | Dose | Mode of administration |
|---|---|---|---|
At birth | BCG | 0.1 ml | Upper right arm; intradermal |
OPV0 | 2 drops | Oral | |
6 weeks | DPT1-HepB1-Hib1 | 0.5 ml | Front outer side of the thigh muscle (intramuscular) |
OPV1 | 2 drops | Oral | |
10 weeks | DPT2-HepB2-Hib2 | 0.5 ml | Front outer side of the thigh muscle (intramuscular) |
OPV2 | 2 drops | Oral | |
14 weeks | DPT3-HepB3-Hib3 | 0.5 ml | Front outer side of the thigh muscle (intramuscular) |
OPV3 | 2 drops | Oral | |
9 months | Measles vaccine | 0.5 ml | Upper right arm; subcutaneous |
- BCG vaccine protects against tuberculosis (TB) and is given once only.
- OPV is the oral polio vaccine, given in four doses numbered 0 to 3.
- DPT is the diphtheria, pertussis, tetanus vaccine, combined in a single preparation with the Hepatitis B vaccine and the Haemophilus influenzae type B vaccine. Together, these five vaccines are known as the pentavalent vaccine (‘penta’ means five). Children get three doses.
- Measles vaccine is given only once.
You should not give OPV0 (the first dose of oral polio vaccine) to an infant who is more than 14 days old. Therefore, if an infant has not received OPV0 by the time he or she is 15 days old, you should wait until the child is four weeks old to give OPV-1. Then also give DPT1-HepB1-Hib1 at four weeks.
Children with diarrhoea who are due for OPV (any dose) should still receive the prescribed dose. However, you should not count this as it may be passed through the body. You should tell the mother to return with the child in four weeks’ time so that you can give the child an extra dose of OPV.
12.3 How to check for immunization status
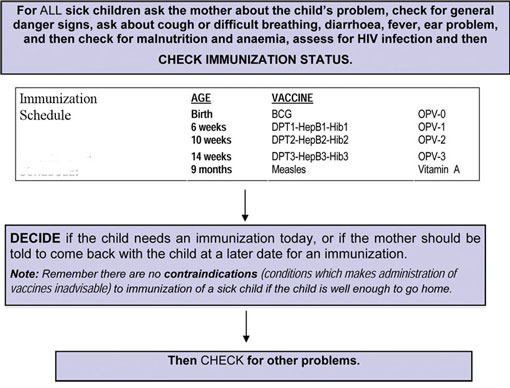
You must check the immunization status of all the children who visit your health post or when you visit them at home. You can use the Assess and Classify chart to help you find the recommended immunization schedule. Box 12.1 outlines the steps you need to take to check the immunization status of each child.
Why is it important to check the immunization status of all children under 24 months old?
Immunization is the most effective strategy for decreasing childhood morbidity and mortality. It can reduce and control illness, disability or death caused by vaccine-preventable diseases.
What dose of OPV would you give to a six-week-old baby who did not receive OPV when born? What are the reasons for your answer?
You would give OPV1. OVPO should not be given to an infant who is more than 14 days old. You would also give the six-week-old infant the DPT1-HepB1-Hib1 vaccination.
In order to decide whether the child needs immunizing right away, you should look at the child’s age on the clinical record. If you do not have this, ask the mother about the child’s age.
ASK the mother if the child has an immunization card. If the mother answers yes, ask her if she has brought the card with her to the health post.
- If she has brought the card with her, ask to see the card.
- Compare the child’s immunization record with the recommended immunization schedule. Decide whether the child has had all the immunizations recommended for the child’s age.
- On the recording form, check all immunizations the child has already received. Write the date of the immunization the child received most recently. Circle any immunizations the child needs in the current visit. These will be any vaccines the child should have already received but has not. For example, if a nine-week-old infant has not yet been vaccinated with DPT1-HepB1-Hib1 and OPV1 (which he should have received at six-weeks-old), you should give the child these vaccines while he is at the health post.
- If the child is not being referred, the mother needs to be advised that the child should receive the relevant immunization (or immunizations) during the visit.
If the mother does not have an immunization card and you have any doubts about what vaccines the child has received, immunize the child.
If the mother says that she does not have an immunization card with her:
- Ask the mother to tell you what immunizations the child has received.
- Use your judgement to decide if the mother has given a reliable report. If you have any doubt, immunize the child. Give the child OPV, DPT-HepB-Hib and the measles vaccine according to the child’s age.
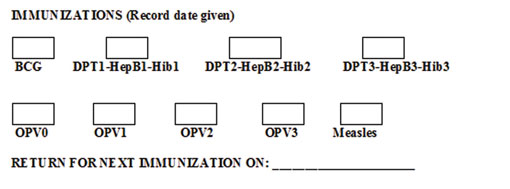
Give an immunization card (as shown in Box 12.2) to the mother and ask her to bring it with her each time she brings the child to the health post.
Box 12.2 Example of immunization card
So far, you have gone through the eight EPI vaccines, their schedule of administration and how to check immunization status of children. In the next section you will learn the contraindications for vaccination.
12.4 Contraindications to vaccine administration
A contraindication is one or more conditions which makes administration of vaccines inadvisable due to some potential side effects. Common illnesses are not contraindications for immunization, so no sick child, including the malnourished child, should miss immunization, unless there is a clear contraindication.
There are only three situations which are considered to be contraindications to immunization:
- Do not give BCG to a child known to have AIDS
- Do not give DPT2-HepB2-Hib2 or DPT3-HepB3-Hib3 to a child who has had convulsions or shock within three days of the last dose of the vaccine
- Do not give any doses of DPT-HepB-Hib to a child with recurrent convulsions or another active neurological disease of the central nervous system.
If a sick child is well enough to go home, there are no contraindications to vaccine administration.
In all other situations, here is a good rule to follow:
- There are no contraindications to immunization of a sick child if the child is well enough to go home
- If you are referring a child, you do not need to give him or her a vaccine before referral. The staff at the referral site should make the decision about immunizing the child when the child is admitted. This will avoid delaying referral.
As you read earlier, children with diarrhoea who are due for OPV should still receive this during their visit to the health post. However, the dose should not be counted and you should tell the mother to return with the child in four weeks for an additional dose of OPV.
You should also advise the mother to be sure the other children in the family are immunized.
12.5 Recording the child’s immunization status
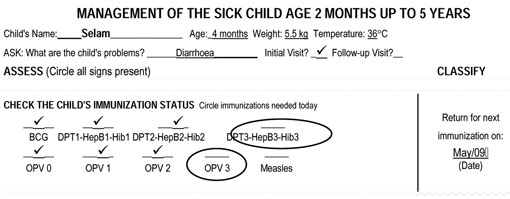
When you have checked the child’s immunization status and given the correct dose of vaccines for the child’s age you should use the case recording form (see Case Study 12.1). Put a check mark (✓) for the immunizations already given and circle the immunizations needed at the current visit. If the child needs to return for an immunization, write the date that the child should return in the classification column.
The case study below illustrates how you should record the immunization status in the correct section of the case recording form.
Case Study 12.1 Selam
Selam is four months old. She has no general danger signs. She is classified as having diarrhoea with no dehydration. Her immunization record (on the case recording form) shows that she has received BCG, OPV0, OPV1, OPV2, DPT1-HepB1-Hib1 and DPT2-HepB2-Hib2. You can see this below.
What advice would you give a mother about her child’s immunization programme?
There are several things you could talk to the mother about, for example the correct age to bring her child for immunization, and that she should bring the child’s immunization record card with her each time she comes to the health post. If you have given an OPV dose at a time the child has diarrhoea, you would also need to tell the mother that she must return for her child to receive another dose in four weeks. You should also tell her that it is important that the whole family is immunized.
Now that you have seen how to enter information about immunization on the child’s record, you are going to learn about routine administration of vitamin A and deworming a child.
12.6 Routine administration of vitamin A and deworming
Vitamin A deficiency and worm infections are common in developing countries and both have serious health effects for a growing child. Preventive therapy should be given routinely for both conditions.
12.6.1 Vitamin A
Vitamin A helps maintain the surface linings of the eyes and the respiratory, intestinal and urinary tracts. It also helps the immune system to resist severe infections.
Vitamin A deficiency (VAD) is a public health problem in many countries, including Ethiopia. It is the leading cause of preventable blindness in children and increases the risk of disease and death from severe infections, particularly measles, diarrhoea and pneumonia. Improving the vitamin A status of children aged 6−59 months can reduce measles and diarrhoea mortality rates by 50% and 33% respectively, and can decrease overall under-five mortality by 23%.
Thus, routine bi-annual (every six months) supplementation of vitamin A is recommended for all children aged 6−59 months of age. You should give one dose if the child has not received a dose within the last six months. The first dose is usually given at nine months of age together with the measles vaccine, and it should then be given every six months up to five years of age. Table 12.2 sets out the correct dose according to the child’s age.
| AGE | VITAMIN A CAPSULES (to be given once every six months) | ||
|---|---|---|---|
| 200,000 IU | 100,000 IU | 50,000 IU | |
| 6 months up to 12 months | ½ capsule | 1 capsule | 2 capsules |
| 12 months up to 5 years | 1 capsule | 2 capsules | 4 capsules |
Footnotes
IU stands for International Units.To administer vitamin A, cut across the nipple of the capsule with a clean instrument (surgical blade, razor blade, scissors or sharp knife). If the vitamin A capsule does not have a nipple, pierce the capsule with a clean needle. Squeeze the capsule gently so drops of vitamin A fall onto the child’s tongue. Record the date each time you give vitamin A to a child. This is important. If you give repeated doses of vitamin A in a short period of time (in less than six months), there is danger of an overdose.
12.6.2 Deworming
Soil-transmitted intestinal worms represent a serious public health problem wherever the climate is tropical and inadequate sanitation and unhygienic conditions prevail. Three types of worms are the most prevalent and have the most damaging effect on the health of preschool children: roundworms, hookworms and whipworms.
Worm infections are associated with a significant loss of micronutrients from the child’s body and contribute to vitamin A deficiency, anaemia, growth failure and malnutrition in children. An infected child’s physical fitness and appetite are negatively affected and their school performance is impaired.
Therefore, all children 24 months of age or older need to be given Mebendazole or Albendazole every 6 months to treat intestinal parasites, especially hookworm and whipworm infections. Table 12.3 sets out the correct doses according to the child’s age, for children who have not been tested in the previous 6 months.
| Mebendazole or Albendazole | ||
|---|---|---|
| Drug | Give as a single dose every 6 months for all children in these age groups | |
| 0–2 years | 2–5 years | |
| Albendazole 400 mg tablet | None | 1 tablet |
| Mebendazole 500 mg tablet or 5 tablets of 100 mg | None | 1 tablet (500 mg) |
When you see a child aged 24 months or older, you should check whether they have been given a dose of Mebendazole or Albendazole in the previous six months. If not, you should give them Mebendazole or Albendazole as indicated in Table 12.3 above.
Only chewable deworming tablets which taste good should be given to children under five years of age. For children under three years of age, tablets should be broken and crushed between two spoons, then water added to help administer the tablets.
Bear in mind that vitamin A supplements are given from the age of six months and deworming tablets are given from the age of two years.
Summary of Study Session 12
In Study Session 12, you have learned that:
- The EPI delivers eight vaccine antigens to protect children against tuberculosis, poliomyelitis, diphtheria, pertussis, tetanus, Haemophilus influenzae type B (Hib) infections, hepatitis B and measles.
- Most vaccines (except BCG and measles) require administration of repeated doses.
- Ideally, every child must complete his or her full vaccination programme before celebrating their first birthday.
- You must check the immunization status of all the children who visit your health post or when you visit them at home. If you have any doubt whether the child has received all the relevant vaccinations you should immunize the child.
- Common illnesses are not contraindications for immunization, and if the sick child is well enough to go home he or she should be vaccinated.
- Vitamin A deficiency and worm infections are common. Both have serious health effects for a growing child and therefore preventive therapy should be given routinely for both conditions. Routine bi-annual supplementation of vitamin A is recommended for all children aged 6−59 months and deworming for all children 2–5 years of age.
Self-Assessment Questions (SAQs) for Study Session 12
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 12.1 (tests Learning Outcomes 12.1, 12.2, 12.3 and 12.4)
How do you decide whether a child who comes to the health post should be immunized?
Answer
First of all you need to check the child’s age, and then consult the immunization schedule which tells you which vaccinations are due and when.
Then you need to check the immunization of the child against this schedule, either using the immunization card if the mother has brought it, or by asking the mother.
Once you know what vaccinations have been missed or are due now, you need to be sure that the child does not have AIDS, has not reacted badly to the previous dose of a vaccine, or have active neurological disease.
If a child is being referred, you should leave the vaccination to staff at the referral unit.
Read Case Study 12.2 and then answer the questions below.
Case Study 12.2 for SAQ 12.2
Kelkay is three months old. She has no general danger signs. She is classified as having diarrhoea with no dehydration and she has anaemia.
Immunization history: BCG, OPV0, OPV1, and DPT1-HepB1-Hib1. OPV1 and DPT1-HepB1-Hib1 given five weeks ago.
SAQ 12.2 (tests Learning Outcomes 12.2, 12.3 and 12.4)
- a.What immunizations, if any, would you give Kelkay today?
- b.What advice would you give to Kelkay’s mother and why?
Answer
- a.This question was asking you to decide whether Kelkay needed any immediate immunizations or not, and to give reasons for your answers. You should have identified that her immunizations are not up-to-date. This means that she needs OPV2 and DPT2-HepB2-Hib2 today. However, do not record OPV2 since she has diarrhoea currently and it needs to be repeated during the next immunization visit.
- b.You should advise the mother that it is important that she ensures Kelkay is brought for her future vaccinations at the right age. You should tell her that she needs to return to the health post after four weeks (at four months of age) to receive DPT3-HepB3-Hib3 and repeat OPV2 immunizations.
Read Case Study 12.3 and then answer the questions below.
Case Study 12.3 for SAQ 12.3
Tahir is 15 months old. He has no general danger signs. He is classified as having no pneumonia: cough or cold and no anaemia and not very low weight for his age. He has completed his full immunization programme, including measles vaccine at nine months of age, when he also took a dose of vitamin A.
SAQ 12.3 (tests Learning Outcomes 12.1, 12.3 and 12.5)
- a.What do you do for Tahir during this visit?
- b.What advice do you need to give to Tahir’s mother?
Answer
- a.Tahir has completed his immunization schedule and does not need additional vaccines. However, he had the last dose of vitamin A six months ago (at nine months of age). You should give the appropriate dose of vitamin A today.
- b.You should advise the mother that it is important that she ensures Tahir is brought for his next dose of vitamin A after six months, and a dose of Mebendazole to treat worm infections when he is 2 years old. Tell her that he needs to return to the health post every six months to get both these treatments until he is five years old.