Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Tuesday, 3 March 2026, 5:38 AM
Integrated Management of Newborn and Childhood Illness Module: 13. Ear Problems and Other Common Childhood Infections
Study Session 13 Ear Problems and Other Common Childhood Infections
Introduction
In this study session you will learn about ear problems and other common conditions affecting children. These conditions do not directly lead to death, but may cause serious complications that can result in permanent disability or death by involving other vital organs. You will learn how to identify a number of the most common ailments in a simple way and offer appropriate treatment and care. You will begin the study session by looking at ear problems and then go on to look at throat, eye and skin infections.
Learning Outcomes for Study Session 13
When you have studied this session, you should be able to:
13.1 Define and use correctly all of the key words printed in bold. (SAQs 13.1, 13.2, 13.3 and 13.4)
13.2 Assess, classify and treat a child with ear problems. (SAQ 13.1)
13.3 Assess, classify and treat a child with throat problems. (SAQ 13.2)
13.4 Identify and treat a child with eye infections. (SAQ 13.4)
13.5 Identify and treat a child with impetigo or scabies. (SAQ 13.3)
13.6 Give appropriate follow-up care for ear, throat, eye and skin infections. (SAQs 13.1, 13.2 and 13.3)
13.1 Ear problems
Ear infections rarely cause death but are major causes of morbidity. In developing countries, they are the leading cause of deafness and learning problems. Therefore it is important for you as a Health Extension Practitioner to know how to identify when a child has an ear problem, and that you are able to assess, classify and provide the appropriate treatment. You also need to know what follow-up care to give a child with an ear problem and how to advise the mother to give home treatment and care.
A child with an ear problem may have an ear infection which can cause ear pain and fever. If an ear infection is not treated on time, the ear drum may perforate and the child feels less pain. Examples of complications of ear infections are meningitis, brain abscess, mastoiditis and deafness.
Mastoiditis is pronounced ‘mass-toy-dye-tiss’.
13.1.1 Assessing ear problems
The Assess and Classify chart will help you identify ear problems caused by ear infection. You should ask about ear problems for every sick child who is brought to your health post.
When you assess a child you will be looking for the following signs:
- ear pain
- ear discharge, and
- if discharge is present, how long the child has had the discharge, and
- tender swelling behind the ear, a sign of mastoiditis.
Box 13.1 is from the ‘Assess’ column in the Assess and Classify chart that tells you how to assess a child for ear problems.
Box 13.1 Assess for ear problems
ASK: Does the child have an ear problem?
| IF YES, ASK: | LOOK AND FEEL: |
|---|---|
∙ Is there ear pain? ∙ Is there ear discharge? If yes, for how long? | ∙ Look for pus draining from the ear ∙ Feel for tender swelling behind the ear |
ASK: Does the child have an ear problem?
If the mother answers no, you do not need to assess the child for ear problems. Your next question in this case would be whether the child has a throat infection (you will learn about throat infections in Section 13.2 below).
If the mother answers yes, ask the next question:
ASK: Does the child have ear pain?
If the mother is not sure that the child has ear pain, ask if the child has been irritable and rubbing his ear. Whether the answer is yes or no you should ask the next question.
ASK: Is there ear discharge? If yes, for how long?
When asking about ear discharge, use words the mother understands. For example, ‘Is there any fluid that looks like pus coming out from the ears?’ If the child has had ear discharge, ask the mother for how long.
LOOK for pus draining from the ear
Look inside the child’s ear to see if pus is draining from the ear. Pus is usually white, creamy or light green and may have an offensive smell.
- An ear discharge that has been present for two weeks or more is defined as a chronic ear infection.
- An ear discharge that has been present for less than two weeks is defined as an acute ear infection.
FEEL for tender swelling behind the ear
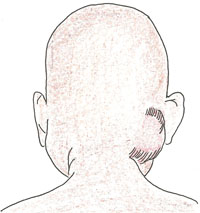
Feel behind both ears. Compare them and decide if there is tender swelling of the mastoid bone. In infants, the swelling may be above the ear.
Both tenderness and swelling must be present to classify mastoiditis, a deep infection in the mastoid bone. You can see an illustration of this in Figure 13.1.
How can you find out whether a sick child brought to your health post has ear problems?
You could ask the mother whether the child has been irritable and rubbing his ear, which suggests it might be painful. You would ask her whether there has been any fluid coming from the child’s ear and for how long this has been happening.
13.1.2 Classify and treat ear problems
There are four classifications for ear problems:
- Mastoiditis
- Acute ear infection
- Chronic ear infection
- No ear infection.
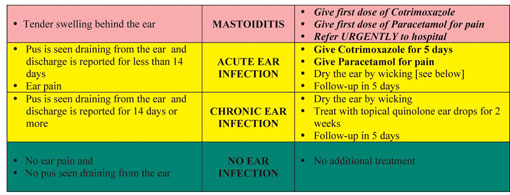
Table 13.2 sets out the classification table for ear problems from the Assess and Classify chart. You can see in the top (pink) row that classification of mastoiditis requires you to give the child one dose each of cotrimoxazole and paracetamol and then refer the child urgently to hospital. The chart also outlines what treatment is required for both acute and chronic ear infection.
Table 13.2 Classification and treatment of ear problems.
You are now going to look in more detail at the different ear problems that a child might have and how you can treat these at the health post or support the mother treating them at home.
Mastoiditis
If a child has tender swelling behind the ear, classify the child as having mastoiditis.
Treatment
You must refer the child urgently to hospital. The child needs treatment with appropriate antibiotics. He may also need surgery. Before the child leaves for hospital, you should give him the first dose of an appropriate antibiotic. You should also treat his pain and high fever with paracetamol.
Acute ear infection
If you see pus draining from the ear and discharge has been present for less than two weeks, or if there is ear pain, classify the child’s illness as acute ear infection.
Treatment
All children with acute or chronic ear infection should be assessed for symptomatic HIV.
Give cotrimoxazole to the child and relieve the ear pain and high fever with paracetamol. Wicking should be done to dry the pus draining from the ear; wicking is described in Study Session 14, which also describes how to counsel a mother about wicking. All Children with acute ear infection and ear discharge should be assessed for symptomatic HIV infection.
Chronic ear infection
If you see pus draining from the ear and discharge has been present for two weeks or more, classify the child’s illness as chronic ear infection.
Treatment
Most bacteria that cause chronic ear infection are different from those which cause acute ear infections. The most important and effective treatment for chronic ear infection is to keep the ear dry by wicking. You should assess all children with chronic ear infection for symptomatic HIV infection.
Topical means ‘applied to the outside of the body, not taken internally.’
Topical quinolone ear drops (such as ciprofloxacin solution, 0.2%) should be instilled into the ear after meticulous ear wicking, three drops three times daily for 14 days. You should show the mother how to wick the ear (see Study Session 14) and instil the ear drops and check whether she has understood the procedure.
No ear infection
If there is no ear pain and no pus is seen draining from the ear, the child’s illness is classified as no ear infection. The child needs no treatment.
13.1.3 Follow-up care for ear problems
If you classified a child with either acute or chronic ear infection you need to tell the mother to return for a follow-up visit five days after her first visit. Box 13.2 below outlines what follow-up care should be given to the child.
Box 13.2 Reassess for ear problems
Measure the child’s temperature.
Treatment
- If there is tender swelling behind the ear or high fever (38.5oC or above), refer the child urgently to hospital.
- Acute ear infection: if ear pain or discharge persists, treat for five more days with the same antibiotic. Tell the mother to continue wicking to dry the ear, and to come for a follow-up visit in five days.
- Chronic ear infection: check that the mother is wicking the ear correctly. Encourage her to continue the ear wicking and giving the child topical quinolone ear drops. Discuss with her the importance of keeping the child’s ear dry.
- If no ear pain or discharge, praise the mother for her careful treatment. If she has not yet finished the five days of antibiotic, tell her not to stop until the end of the fifth day.
You are now going to do an activity which will check your understanding of what you have learned so far.
Activity 13.1
Case Study 13.1 and Case Study 13.2 describe children who have ear problems. In the box after each case study make notes on the following:
- The steps would you take to assess each child’s ear problem.
- How you would classify the ear problem in each case.
- What treatment you would give the child in each case.
If you need to remind yourself of the different classifications, either use the wall chart or your chart booklet at your health post, or refer to the materials that you have already looked at in this study session.
Case Study 13.1 Mebrat
Mebrat is three years old. She weighs 13 kg. Her temperature is 37.5°C. Her mother came to the clinic today because Mebrat has felt hot for the last two days. The health worker checked and found no general danger signs.
Next the health worker asked about Mebrat’s ear problem. The mother said she was sure Mebrat had no ear pain, but that she had seen discharge coming from Mebrat’s ear for about three weeks. The health worker saw pus draining from the child’s ear. She felt behind the child’s ears and found tender swelling behind one ear.
Write your notes in the space below on how to assess, classify and treat Mebrat’s ear problems
Case Study 13.2 Danso
Danso is 18 months old. She weighs 9 kg. Her temperature is 37°C. Her mother says that Danso had discharge coming from one of her ears for the last three days.
Danso does not have any general danger signs. She does not have cough or difficult breathing. She does not have diarrhoea and she does not have fever.
The health worker asked about Danso’s ear problem. The mother said that Danso does not have ear pain, but discharge has been coming from one ear for three or four days. The health worker saw pus draining from the child’s right ear. She did not feel any tender swelling behind either ear.
Write your notes in the space below on how to classify and treat Danso’s ear problem
Comment
Clearly, the children in both cases have ear problems. You should have noted that Mebrat has chronic ear infection because the duration of the discharge from the ear is over two weeks. In addition there is a tender swelling behind one of her ears which indicates that she has mastoiditis which, as you learned, is a serious complication of ear infection. Mebrat therefore needs to be referred urgently after the first dose of an antibiotic has been administered. There is no need to waste time by showing her mother how to clean the ear.
In the case of Danso the duration of ear discharge is only three days. There is no swelling behind the ear. You should therefore have classified Danso as having acute ear infection. She should be treated with cotrimoxazole twice per day for five days. You should advise the mother to come back for a follow-up visit in five days. You should also assess Danso for symptomatic HIV.
13.2 Throat problems
You are now going to look at how to assess, classify and treat children who have throat problems. All children who are brought to your health post should be assessed for throat problems.
13.2.1 Assess for throat problems
When you assess for throat problems you should follow these steps:
ASK:
- Does the child have fever?
- Does the child have sore throat?
FEEL:
- For enlarged tender lymph nodes on the front of the neck.
LOOK:
- For red (congested) throat.
- For exudate (white or yellow patches) on the throat and tonsils.
The pharynx is the space behind the nose and the mouth. In a typical case of pharyngitis (sore throat) the pharynx is distinctly red and inflamed and the tonsils are enlarged and covered with yellow pus. There are complications of pharyngitis, including parapharyngeal abscess (this is when pus accumulates behind the structures of the pharynx) and disease of the heart and kidneys.
The key points above are summarised in Table 13.4, which is reproduced from the section in the Assess and Classify chart booklet that tells you how to assess a child for sore throat.
ASK: | LOOK AND FEEL: |
|---|---|
∙ Does the child have fever? (by history or feels hot or temperature 37.5°C or more) | ∙ Feel for enlarged tender lymph nodes on the front of the neck. |
∙ Does the child have a sore throat ? | ∙ Look for red (congested) throat. |
∙ Look for white or yellow exudates on the throat and tonsils. |
13.2.2 Classify for throat problems
There are three possible classifications of throat problem:
- Streptococcal sore throat (Streptococci are the bacteria most often involved in causing throat infections).
- No streptococcal sore throat
- No throat problem.
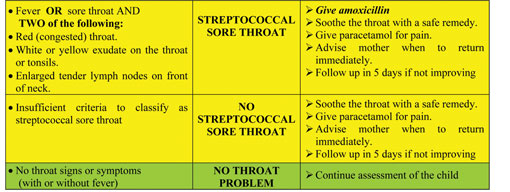
Table 13.5 reproduces the section from the Assess and Classify chart booklet for the classification and treatment of sore throat.
Table 13.5 Classification and treatment of throat problems.
Treatment
As you can see from Table 13.5, there is a range of treatments that you should provide for a child with a throat problem:
- Give an oral antibiotic, amoxicillin for 10 days
- Give paracetamol if the child has a fever with a temperature higher than 38.5°C
- Soothe the child’s throat with warm tea and honey.
13.2.3 Follow-up care for throat problems
If you have assessed the child as having a throat problem, you should tell the mother that she must return with the child for follow-up in five days if there is no improvement. When she returns, you should reassess the throat problem using the guidelines in the Assess and Classify chart booklet and described in this study session. You will need to measure the child’s temperature and if you assess fever you should give the child paracetamol. If there has been no improvement in the sore throat you should refer the child to hospital.
13.3 Eye infection: conjunctivitis
Conjunctivitis is common in young children, especially if they come into contact with other children with conjunctivitis. There are different types of conjunctivitis that infants and children can suffer from, some more serious than others and potentially leading to loss of vision.
Acute conjunctivitis, or red eye, is usually a bacterial or viral infection of the eye characterised by a rapid onset of symptoms that persists for a few days.
Neonatal conjunctivitis, or ophthalmia neonatorum, is purulent conjunctivitis during the first ten days of life, usually acquired during birth. If the mother has gonorrhoea this can cause conjunctivitis in the newborn by infection during the birth.
Purulent is pronounced ‘purr-you-lent’, and means ‘with pus’.
Purulent conjunctivitis is eye infection with pus discharge from the eyes; it is caused by bacteria. In newborns, if the mother has gonorrhoea it can cause severe conjunctivitis with profuse purulent discharge.
Treatment
There are a number of ways to treat acute conjunctivitis. You should show the mother how she can treat her child at home, following the steps outlined below.
13.3.1 Treat eye infection with tetracycline eye ointment
- Clean both eyes three times daily, using a clean cloth for each eye.
- Wash hands before and after treating the eye
- Ask the child to close the eyes
- Use the clean cloth and water to gently wipe away pus.
- Apply tetracycline eye ointment in both eyes three times per day.
- Ask the child to look up
- Squirt a small amount of ointment on the inside of the lower lid
- Wash hands again.
- Treat until redness is gone
- Do not use other eye ointment or drops, or put anything else in the eye.
If you assess that the newborn has neonatal conjunctivitis you should refer the infant immediately because this is a serious problem that may lead to loss of vision. It needs treatment with injectable antibiotics.
13.3.2 Follow-up care for eye infection
You should advise the mother to return to the health post two days after the initial assessment. Box 13.3 sets out the steps to take at the follow-up visit.
Box 13.3 Follow-up for eye infection
Treatment for eye infection
After two days: Look for red eyes and pus draining from the eyes.
∙ If pus is still draining from the eye, ask the mother to describe how she has treated the eye infection. If treatment has been correct, refer the child to hospital. If treatment has not been correct, teach the mother the correct treatment.
∙ If the pus is gone but redness remains, tell the mother to continue with the treatment. After finishing the treatment, if there is no change she should return for further evaluation.
∙ If no pus or redness, stop the treatment.
13.4 Bacterial skin infections
In Ethiopia, skin diseases are common. In most situations caregivers do not seek medical help. However, your role in providing effective healthcare for a child means that you should look for and treat skin diseases. Some skin diseases can lead to serious complications unless treated appropriately. In this section you will learn how to assess, classify and treat some common childhood skin infections.
13.4.1 Assess skin infections
If the mother brings in her child because he has a skin infection, you should start by asking her some simple questions such as ‘Does the child have skin itchiness?’ Or, ‘Does the child have pain from the skin problem?’ If the mother answers yes to your questions you should then get more detailed information from her and look for the signs set out in Box 13.4.
Box 13.4 Signs of skin infection
Ask the mother:
- ‘Does the child have skin itchiness?’
- ‘Does the child have pain from the skin problem?’
Then, look and feel more closely for:
- extensive warm, redness and swelling
- localised warm, tender swelling or redness
- swelling or redness around the eyes
- obvious lesions with pus or crusts
- small swellings on the skin of the hands, knees, elbows, feet, trunk
- round or oval scaly patches.
13.4.2 Classify and treat skin infections
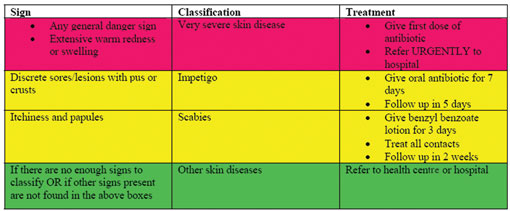
After assessing the child for skin infections, the next step is to use all your findings so that you can classify the skin condition as shown in Table 13.6 reproduced from the Assess and Classify chart.
Table 13.6 Classify and treat skin infections.
Impetigo
Impetigo is common among preschool children and young adults as well. Impetigo begins as a single reddish tiny swelling containing fluid that progresses to one or many honey-coloured, crusted lesions weeping fluid. Impetigo most frequently occurs on the face, around the nose and mouth, and on the extremities. It is associated with increased risk of kidney disease and it should be treated by giving the child amoxicillin for seven days. Follow-up care should be provided five days after the initial classification.
Scabies
Scabies is characterised by severe itching. It is caused by small mites that burrow under the skin, and is transmitted by close contact the infected person. Itching is intense, particularly during the night.
Vesicles distributed in the web spaces of fingers, wrist, elbows, umbilical area, genital area and feet are often seen. Usually the face and neck are not affected.
Vesicles: small swellings on the skin containing clear fluid. Scabies is described in more detail in Study Session 39 of Communicable Diseases, Part 4.
Children with scabies should be treated with an application of 25% benzyl benzoate lotion daily to the whole body below the neck. The solution should be left on for 13 hours and should then be washed off. The treatment should continue for three days. All family members and close contacts of the child should be treated simultaneously, as scabies is very contagious. Follow-up care should be provided within two weeks of the initial classification.
In this study session you have learned about common problems in children, most of which may not appear to cause risk of immediate death. However, as you have seen, diseases of the ears, throat, eyes and skin can give rise to serious medical problems that may lead to death or to disability. Therefore your role in early identification of problems and providing the appropriate treatment and follow-up care is very important.
Summary of Study Session 13
In Study Session 13, you have learned that:
- All children brought to the health post should be assessed for ear, throat, eye and skin infections.
- Disease of the ears, throat or eyes and skin infections in children under five can give rise to serious medical problems and may lead to disability or even death.
- A child who has mastoiditis must be referred urgently to hospital.
- Wicking a child’s ear can be an effective treatment for less serious ear problems.
- Conjunctivitis in newborns is a serious problem that may lead to loss of vision if not treated with antibiotics.
- Some skin diseases can lead to serious complications, such as kidney disease, if they are not treated properly.
Self-Assessment Questions (SAQs) for Study Session 13
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
Read Case Study 13.3 and then answer the questions below.
Case Study 13.3 for SAQ 13.1
A mother brings her ten-month-old infant to your health post, saying that her child has had an ear discharge for about four or five days and he is crying more than usual. He has no swelling behind either ear.
SAQ 13.1 (tests Learning Outcomes 13.1, 13.2 and 13.6)
- a.How would you classify this infant’s illness? Give reasons for your answer.
- b.What complications might develop from the illness?
- c.How would you treat the infant?
Answer
- a.You should have classified this child as having acute ear infection. This is because the infant has not had pus draining from the ear for two weeks or longer (which would be a sign of chronic ear infection). As there is no swelling, the infant is not showing signs of mastoiditis.
- b.If the infection is not treated, however, it could develop into mastoidistis, which you will recall is a serious condition that requires the child to be referred urgently. Untreated, the infection could also lead to deafness.
- c.The child should be given cotrimoxazole for five days and you should show the mother how to wick the child’s ear each day. She could also give the child paracetamol to ease the pain.
Read Case Study 13.4 and then answer the questions below.
Case Study 13.4 for SAQ 13.2
A four-year-old child is brought to your health post. Her mother says that the child is finding it painful to swallow and she has been feeling very hot to the touch for the last two days. When you examine the child’s throat, you see it is red and there is some yellowish pus.
SAQ 13.2 (tests Learning Outcomes 13.1, 13.3 and 13.6)
- a.How would you classify this child’s illness? Give reasons for your answer.
- b.How would you treat the child?
- c.How would you advise the mother?
Answer
- a.The classification in this case is streptococcal sore throat. You might remember that enlarged and tender lymph nodes on the neck are also signs of this illness.
- b.The treatment includes giving the child the antibiotic amoxycillin and soothing the throat with a safe home remedy such as warm tea or honey. Paracetamol can be given to ease the pain.
- c.You would advise the mother to return immediately if her child’s syptoms became much worse. Otherwise, she should treat the child at home and only return if the child is not showing signs of improvement five days after the visit to your health post.
Read Case Study 13.5 and then answer the questions below.
Case Study 13.5 for SAQ 13.3
A three-year-old boy is brought to your health post because he has some small skin lesions on his neck. The lesions are crusted and have a yellow discharge.
SAQ 13.3 (tests Learning Outcomes 13.1, 13.5 and 13.6)
- a.How would you classify this problem? Give reasons for your answer.
- b.What possible complications are linked with this problem?
- c.How would you treat the child?
Answer
- a.In this case, the child has impetigo, identified by the crusted lesions weeping yellow fluid.
- b.If impetigo is not treated effectively, if can lead to kidney disease.
- c.To treat this condition, the child should be given an oral antibiotic for seven days, with a follow-up visit in five days.
SAQ 13.4 (tests Learning Outcomes 13.1 and 13.4)
Describe how you would treat conjunctivitis, and give reasons for your answer.
Answer
You should have included the following steps in your answer: both eyes should be cleaned three times daily, using a clean cloth for each eye; tetracycline ointment should then be applied in both eyes three times per day until the redness has gone. Other eye ointments or drops should not be put into the child’s eyes.