Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Monday, 9 March 2026, 7:41 PM
Integrated Management of Newborn and Childhood Illness Module: 15. Synthesis of IMNCI for a Sick Child up to Five Years: Assess and Classify
Study Session 15 Synthesis of IMNCI for a Sick Child up to Five Years: Assess and Classify
Introduction
This Module has introduced you to the integrated strategy for managing and treating the major childhood illnesses. You have learned how to assess, classify, identify and provide appropriate treatment for children under five years old. Each study session has been designed to help you understand each of the main symptoms individually. However, as you read in the introduction to the Module, IMNC is an integrated strategy and therefore you need to understand how all the components work together to ensure you can provide the best possible care and support for a sick child and advise parents how to give effective home care. The purpose of the next two study sessions therefore, is to help you learn how to look at a child holistically. This study session will look at assessing and classifying the sick child.
Learning Outcomes for Study Session 15
When you have studied this session, you should be able to:
15.1 Define and use correctly all of the key words printed in bold. (SAQ 15.1)
15.2 Demonstrate that you know how to determine health problems in children up to five years old. (SAQ 15.1)
15.3 Describe the severity of a child’s condition. (SAQ 15.1)
15.1 Integrated case management process
The IMNCI guidelines are based on the following principles:
- All sick children must be checked for ‘general danger signs’ which indicate the need for immediate referral or admission to a higher health facility level.
- All sick children must be routinely assessed for major symptoms: cough, fever, diarrhoea, ear problems.
- Children should also be assessed for nutritional and immunization status, feeding problems and other problems.
You learned about all of these key principles in the earlier study sessions in this Module. We are now going to describe how to bring your learning together so you can treat the sick child in a holistic way.
Triage is pronounced ‘tree-ahj’.
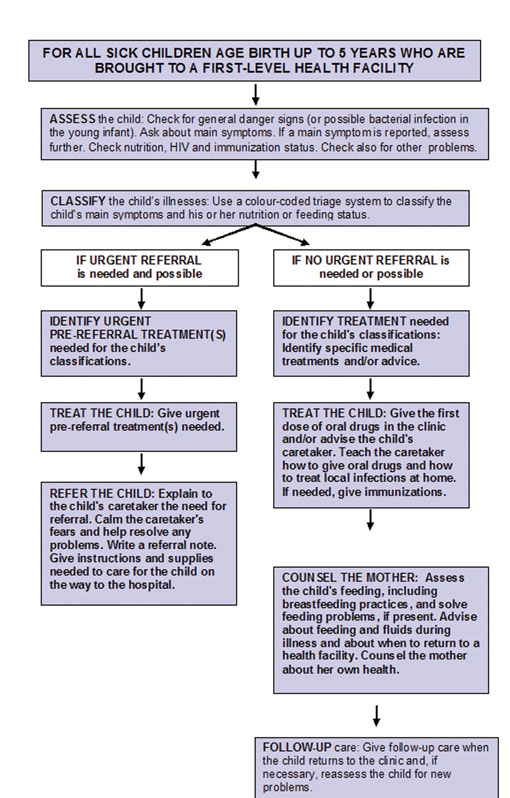
Figure 15.1 summarises the integrated case management process in the form of a flow diagram. Take a few moments to look at this now. After assessing for general danger signs, other symptoms and problems, the next step is to use the colour coded triage system (identifying the appropriate treatment according to the priority or severity of the symptoms). This guides how you classify the child’s main symptoms, feeding status and nutrition. You can see from Figure 15.1 that the classification will be either ‘urgent referral is needed and possible’ or ‘no urgent referral needed or possible’.
As well as understanding the case management process, it is important that you know how to select the correct chart for managing the sick child.
15.2 Selecting the appropriate case management charts
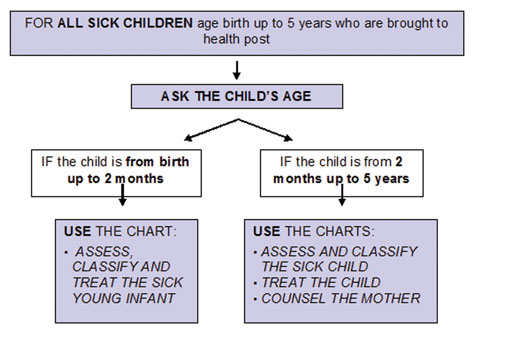
The IMNCI chart booklet contains three charts for managing sick children aged two months up to five years, and a separate chart for managing sick young infants from birth up to two months.
Depending on the procedure for registering patients at the health post, the child’s name, age and other information (such as address) may have been recorded already. If not, you should begin by asking the child’s name and age, before deciding which age group a child is in, which will be either:
- Age birth up to two months, or
- Age two months up to five years.
You should then select the appropriate chart for the child. Figure 15.2 shows this decision-making process.
The IMNCI case management charts guide you through the following steps:
- Assess the sick child or sick young infant
- Classify the illness
- Identify the treatment
- Treat the child or young infant
- Counsel the mother
- Give follow-up care.
The case management steps are the same for all sick children from birth up to five years. However, because signs, classifications, treatments and counselling differ between sick young infants and sick children, it is essential to start the case management process by selecting the appropriate set of IMNCI charts. The charts, tables and registration books for the sick child aged two months up to five years are briefly described below.
15.2.1 Assess and Classify chart
You are now going to look at how to use the Assess and Classify chart. You will need to have a copy of the IMNCI chart booklet with you. It will help you to have a copy to refer to throughout the rest of this study session.
First, complete Activity 15.1.
Activity 15.1 Using the Assess and Classify chart
Open your chart booklet on page 22. You will see that this is the Assess and Classify chart for a sick child aged two months up to five years. Take a few moments to read the information there, and look at how the Assess column on the left-hand side describes how to take a history and do a physical examination. You will see that it describes how to assess for general danger signs (in the upper box) and the main symptom, cough (in the lower box). When you complete the sick child’s recording form you will need to make a note of the main symptoms and signs you found during the examination.
15.2.2 Identify treatment
The Identify Treatment column of the Assess and Classify chart helps you to identify quickly the treatment needed for the classifications written on your case recording form. Appropriate treatments are recommended for each classification. When a child has more than one classification, you must look at more than one table to find the appropriate treatments, for each one, and write these on the reverse side of the case recording form.
15.2.3 Treat the child
The IMNCI chart entitled Treat the Child shows you how to carry out the treatment steps identified on the Assess and Classify chart. ‘TREAT’ can mean giving treatment in the health post, or prescribing drugs or other treatments to be given at home; it can also mean teaching the caregiver how to carry out the treatments. For example, if you look at page 29 in your chart booklet you can see that there are two boxes. The box on the left side of the page describes ‘Teach the mother to give oral drugs at home’ and on the right side you will see ‘Give an appropriate oral antibiotics’.
15.2.4 Give follow-up care
Several treatments in the Assess and Classify chart require the mother to return to the health post with her child for a follow-up visit. At a follow-up visit you can see whether the drug or other treatment that was prescribed for the child has been effective, and that the child’s health is improving. The Give Follow-up Care section (page 38 in the chart booklet) of the Treat the Child chart describes the steps for conducting each type of follow-up visit.
15.2.5 Counsel the mother
Recommendations on feeding, fluids for the sick child, and when the mother should return with her child to the health post are given on the chart titled Counsel the Mother. If you look at page 42 of your chart booklet you will see that it describes assessing the child’s feeding. For many sick children, you will have to assess feeding and counsel the mother about any feeding problems that you have identified. For all sick children who are going home, you should advise the child’s mother about feeding, fluids she must give the child, and when to return for further care. You should always write the results of any feeding assessment on the bottom of the case recording form. An important aspect of your role as a Health Extension Practitioner is to provide advice to the mother about her own health.
You are now going to look at how to assess and classify for children up to two months old, beginning with essential newborn care.
15.3 The sick young infant from birth up to 2 months
You have already come across some of the information earlier in your studies. However, as the immediate care of a newborn can make a significant difference to the life chances of that child, it is critical that you feel confident in being able to provide the most effective integrated care possible. You should therefore see this section as an opportunity to really understand your role and task as a Health Extension Practitioner when looking after a newborn baby.
Care of the normal newborn, and the special care needed for preterm and low birth weight babies, is described in the Postnatal Care Module.
The care you give immediately after birth is simple but important. Most babies breathe and cry at birth with no help. Remember that the baby has just come from the mother’s uterus. It was warm and quiet in the uterus and the amniotic fluid and walls of the uterus gently touched the baby. You too should be gentle with the baby, and keep the baby warm. Skin-to-skin contact with the mother keeps the baby at the perfect temperature.
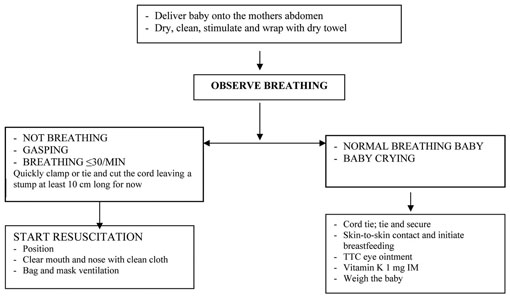
15.3.1 Steps of immediate newborn care
You have learned the steps of immediate care which should be given to all babies at birth. In case you need to remind yourself what these are, take a look at Figure 15.3 below.
![]() If any danger sign is present refer the baby urgently.
If any danger sign is present refer the baby urgently.
Study Session 1 of this Module described the newborn danger signs (so look back at this if you need to remind yourself what they are).
What are the newborn danger signs?
You should have recalled that the newborn danger signs are that the child:
- is not able to drink or breastfeed
- vomits everything
- has convulsions, in the past or during the visit
- is lethargic or unconscious.
15.3.2 Assess and classify the sick young infant
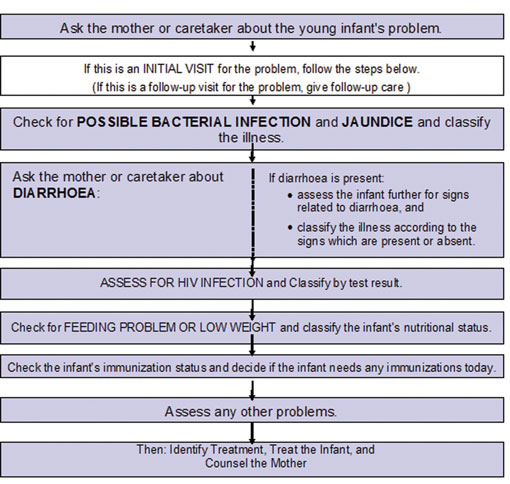
This section describes the steps you should take to assess and classify a sick young infant at the initial visit.
When a sick child is brought to your health post for an initial visit you should always do the following:
- Check for signs of possible bacterial infection. Then classify the young infant based on the clinical signs found
- Ask about diarrhoea. If the infant has diarrhoea, assess for related signs. Classify the young infant for dehydration. Also classify for persistent diarrhoea and dysentery, if present
- Check for feeding problems or low weight. This may include assessing breastfeeding. Then classify feeding
- Check the young infant’s immunization status
- Assess any other problems.
If you find a reason that a young infant needs urgent referral, you should continue the assessment. However, you should not carry out the breastfeeding assessment because this can take some time. Figure 15.4 below summarises these steps.
How to classify possible bacterial infection
Assessing for bacterial infection is critically important and must be done for every sick young infant. In this step you are particularly looking for signs of a serious infection. A young infant can become sick and die very quickly from serious bacterial infections such as pneumonia, sepsis and meningitis.
You should assess and classify all sick young infants for bacterial infection and jaundice. Compare the infant’s signs with the signs listed on the appropriate chart and choose the appropriate classification.
- If the infant has any sign in the top (pink) row, select possible serious bacterial infection or very severe disease.
- If the infant has any sign in the middle (yellow) row, select local bacterial infection.
- An infant who has none of the signs gets the classification of bacterial infection unlikely (green row).
How to assess and classify a young infant for diarrhoea
Remember that you should always ask the mother whether the young infant has diarrhoea. If she says yes, or you see that the young infant has diarrhoea, you should classify for diarrhoea. You learned about this in Study Session 5 of this Module, and should be able to recall that a young infant with diarrhoea is assessed for:
- how long the child has had diarrhoea
- blood in the stool to determine if the young infant has dysentery, and
- signs of dehydration.
Classify diarrhoea
Diarrhoea in a young infant is classified in the same way as it is in an older infant or young child.
Assess for HIV infection
Look at the chart on assessing and classifying the sick young infant for HIV infection. You should ask the mother whether she or her child has had a positive HIV test. Remember this can be a very sensitive issue for the mother so you should ask her in a respectful way and reassure her that the information is confidential.
If the child has had an HIV test, determine whether the test was a rapid test for HIV antibodies, or a DNA PCR test for the virus, and then classify the sick young infant for HIV infection base on the test result.
How to check a young infant for feeding problems or low weight
Assessing feeding and/or low weight problems has two steps. If you look at page 8 in your chart booklet you will see there are two sections in the box separated by a dashed line. In the first (upper) part are the questions you should ask the mother. You need to determine if she is having difficulty feeding the infant, what the young infant is fed and how often. You also need to determine weight for age.
If the infant has any problems with breastfeeding or is low weight for age, you assess how the infant breastfeeds. You will see this is the second (lower) part of the box on page 8 in your chart booklet.
How to classify feeding problems or low weight
There are three possible classifications for feeding problems or low weight:
- Not able to feed — possible serious bacterial infection
- Feeding problem or low weight
- No feeding problem.
How to check the young infant’s immunization status
You should check the immunization status by checking the immunization card, and if this is not available you should ask the mother what vaccinations her child has received
How to assess other problems
Assess any other problems mentioned by the mother or observed by you.
You are now going to look at how to assess and classify children aged between two months and five years.
15.4 Assess and classify the sick child aged two months to five years
When you see the mother, or the child’s caregiver, with the sick child you should:
- Greet the mother appropriately and ask about the child
- Look to see if the child’s weight and temperature have been recorded
- Ask the mother what the child’s problems are
- Determine if this is an initial (first) or follow-up visit for this episode of an illness or problem.
If the child was seen a few days before for the same illness, this is a follow-up visit. A follow-up visit has a different purpose from an initial visit. During a follow-up visit, you find out if the treatment given during the initial visit has helped the child. If the child is not improving or is getting worse after a few days, you need to make a decision whether to refer the child to a hospital or change the child’s treatment.
15.4.1 Assess and classify general danger signs
You are now going to look again at how you assess and classify a sick child ages two months to five years. First you need to assess for the general danger signs, then you need to assess the child for cough and difficult breathing.
15.4.2 Assess and classify cough or difficult breathing
Once you have assessed a child for general danger signs, you should ask the mother, ‘Does the child have cough or difficult breathing’? If the answer is ‘yes’, continue with the assessment.
How to classify cough or difficult breathing
There are three possible classifications for a child with cough or difficult breathing:
- Severe pneumonia or very severe disease
- Pneumonia
- No pneumonia, cough or cold.
15.4.3 Assess and classify diarrhoea
After you assessed for cough or difficult breathing, the next step is to assess the child for diarrhoea.
How to classify diarrhoea
The three classifications for diarrhoea are dehydration, persistent diarrhoea and dysentery. Dehydration and persistent diarrhoea are classified as follows:
Dehydration
- Severe dehydration
- Some dehydration
- No dehydration.
Persistent diarrhoea
- Severe persistent diarrhoea
- Persistent diarrhoea.
Dysentery does not have any other classification.
Fever
The next main symptom you need to assess is fever. A child with fever may have malaria, measles or another severe disease. Or, a child with fever may only have a simple cough or cold or other viral infection.
How to assess fever
Ask about fever in ALL sick children.
If you open your chart booklet at p.24 you will find the assessment box for fever. You can see that the assessment of fever has two parts. The upper part of the box (above the broken line) describes how to assess the child for signs of malaria, measles, meningitis and other causes of fever. The lower part of the box describes how to assess the child for signs of measles complications, if the child has measles now or has had measles within the last three months.
Because fever can be caused by serious illnesses, such as malaria, measles and meningitis, as well as more simple illnesses (such as a common cold), it is important that you are able to recognise and assess fever and classify the illness that is causing it.
If the child has a fever, what are the three levels of malaria risk?
You will need to decide whether a child with fever has a high risk, a low risk or no risk for malaria. You should ask about the duration of the fever and, if the child has recently travelled, whether it was to a high or low risk area. If you are not certain, you should assume a high risk of malaria.
What signs should you look for in the child with fever?
You should examine the child for stiff neck, runny nose and signs suggestive of measles, such as a generalised rash, cough or red eyes.
How to classify fever
If the child has fever and no signs of measles, classify the child for fever only. If the child has signs of both fever and measles, classify the child for fever and for measles.
There are three possible classifications for fever in an area with low malaria risk:
- Very severe febrile disease
- Malaria
- Fever – malaria unlikely.
There are two possible classifications for fever in an area with no malaria risk:
- Very severe febrile disease
- Fever – malaria unlikely.
There are three possible classifications for measles:
- Severe complicated measles
- Measles with eye or mouth complications
- Measles.
You are now going to look at the management of children with ear problems.
15.5 Ear problems
15.5.1 How to assess an ear problem
You learned about ear problems in Study Session 13. As you read, although ear problems do not directly lead to death, they can cause serious complications that may result in permanent disability or death by involving other vital organs.
Ask about ear problems in all sick children. Ask the mother or caregiver whether the child has any ear pain or ear discharge and for how long they have had fever. Look for pus draining from the ear or feel for tender swellings behind the ear.
15.5.2 How to classify an ear problem
There are four classifications for ear problems:
- Mastoiditis
- Acute ear infection
- Chronic ear infection
- No ear infection.
Study Session 13 looked at each of these problems in detail, so you should return to this study session if you need to remind yourself what is the appropriate treatment for each classification.
15.6 Malnutrition and anaemia
Check ALL sick children for signs suggesting malnutrition and anaemia.
A mother may bring her child to the health post because the child has an acute illness. A sick child can also be malnourished, but the child’s family may not notice the problem, because the child may not have specific complaints that point to malnutrition and anaemia. A child with malnutrition has a higher risk of disease and death. There it is important that you check all sick children for signs suggesting malnutrition and anaemia.
15.6.1 How to assess for malnutrition and anaemia
- Look for:
- visible severe wasting
- palmar pallor
- oedema of both feet
- weight for age.
What are the signs or palmar pallor?
If the skin of the child’s palm is pale, but has some pink areas, the child has some palmar pallor. If the skin is very pale or so pale that it looks white, the child has severe palmar pallor.
How do you determine whether there is oedema?
If you press gently with your thumbs on the topside of each of the child’s feet for at least three seconds and a dent remains following the pressuring, oedema is present.
15.6.2 How to classify nutritional status and anaemia
As you read in Study Session 7, adequate feeding is essential for a child’s growth and development. Poor feeding during infancy can have a lifelong effect, so recognising problems and improving feeding if necessary is an important task for you as a Health Extension Practitioner.
There are six classifications for a child’s nutritional status and anaemia:
- Severe malnutrition
- Very low weight
- Not very low weight
- Severe anaemia
- Anaemia
- No anaemia.
Take another look at the descriptions in Study Session 7 of this Module, if you need to remind yourself how to assess nutritional status and anaemia, and what recommendations you can give a mother for feeding her infant and young children in ways appropriate to their age and needs.
15.7 HIV infection
15.7.1 Assess for HIV infection
If during assessment up to this point, a child has been found to have at least one or more of the following classifications:
- Pneumonia or severe pneumonia now
- Persistent or severe persistent diarrhoea now
- Acute ear infection with ear discharge or chronic ear infection
- Very low weight for age or severe malnutrition
or, if the mother or child is known to be HIV positive, you should do an assessment for HIV infection.
15.7.2 Classify for HIV infection
There are five classifications in the Assess and Classify chart:
- Confirmed symptomatic HIV infection
- Confirmed HIV infection
- Suspected symptomatic HIV infection
- Possible HIV infection
- HIV infection unlikely.
You learned about these classifications in Study Session 9. As you read, children with HIV are more likely to get infections and get them more often, and pneumonia in particular is a leading cause of hospital admissions and death in HIV-positive children. The correct classification will enable you to identify the most appropriate treatment, if any, for the child.
15.8 Immunization status
Check the immunization status of ALL sick children.
Immunization is the single most cost-effective strategy to decrease childhood morbidity and mortality. Checking the immunization status of every child is therefore very important – ideally, every child will complete their full vaccination programme before their first birthday.
You must use the recommended immunization schedule. Take another look at Table 12.1 in Study Session 12 of this Module if you need to remind yourself what this schedule is from birth to nine months.
15.9 Other problems
In Study Session 13 you learned about some common childhood problems. You should always ask the mother whether the child has any problems as well as observe any during the child’s visit. For example, the child may have throat, eye or skin problems. You need to assess for these and decide what treatment, if any, is needed.
As with ear problems, throat, eye and skin infections can give rise to serious medical problems that can lead to death or to disability. Therefore your role in early identification of these problems and providing appropriate treatment and follow-up care is very important.
15.10 Checking the mother
You should also remember that it is important to check the health of the mother.
- Ask if the mother is sick
- Ask if she has any breast problems
- Check the mother’s immunization status
- Check if the mother has access to family planning, and counselling on sexually transmitted infections (STIs) and HIV/AIDS prevention.
In this study session you have looked at the integrated case management charts and learned what steps you need to follow in order to assess and classify a sick child. You learned that these steps are based on the IMNCI principles which ensure you consider the child as a whole. In the next and final study session we will remind you how to identify the necessary treatments and follow-up care for a sick child.
Summary of Study Session 15
In Study Session 15, you have learned that:
- IMNCI guidelines are based on principles that require you to assess and classify the whole child.
- You need to choose the correct chart for the sick young infant and child.
- There are integrated processes for assessing and classifying the sick young infant and child from birth up to five years old.
- It is important to check the mother’s own health.
Self-Assessment Questions (SAQs) for Study Session 15
Now that you have completed this study session you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answer in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
Read Case Study 15.1 and then answer the questions that follow.
Case Study 15.1 for SAQ 15.1
Rediet is six months old. She weighs 6 kg. Her mother has brought her into the health post because the child has a fever.
The health worker checks for general danger signs. Rediet is able to drink, has not vomited, has not had convulsions and is not lethargic or unconscious. She has not had any convulsions while at the health post.
The health worker assesses Rediet for cough or difficult breathing, and counts 54 breaths per minute. She notes that Rediet has no chest in-drawing or stridor when calm. Although Rediet has had diarrhoea for three days, there is no blood in her stool. She drinks eagerly and the skin pinch goes back slowly.
Rediet’s family live where there is a high malaria risk. She has had a fever for five days. There is no rash, her eyes are not red, she does not have a stiff neck or a runny nose. There is some discharge from her ear, and her mother says that Rediet has had this fluid coming out of her ear for some weeks.
The health worker checks Rediet for malnutrition and anaemia; Rediet does not appear to have visible severe wasting. There is no palmar pallor and no signs of oedema. Her weight for age is also checked.
Rediet’s mother tested as HIV-positive during her pregnancy. Rediet has oral thrush, and no enlarged lymph nodes or parotid glands.
SAQ 15.1 (tests Learning Outcomes 15.1, 15.2 and 15.3)
- a.How would you assess and classify Rediet? Give reasons for your answer.
- b.What treatment does Rediet need and why? Does Rediet need to be referred urgently for any reason?
- c.What advice would you give to Rediet’s mother?
Answer
- a.Your assessment and classification for Rediet should have included the following information:
Cough or difficult breathing
Rediet has a cough and her breathing rate is 54. For her age she has fast breathing, but no chest in-drawing or stridor. Thus the classification is pneumonia.
Diarrhoea
Rediet has had diarrhoea for three days. She has also the following signs: drinking eagerly and skin pinch goes back slowly. Thus she is classified as ‘some dehydration’.
Fever
Rediet has fever and she is from a high risk malaria area. Thus the classification is malaria.
Ear discharge
Rediet has had an ear discharge for some weeks. The classification is chronic ear infection, because the discharge has been happening for over two weeks.
Rediet has oral thrush, pneumonia and chronic ear discharge. Because her mother tested HIV-positive, Rediet must be classified as suspected symptomatic HIV infection. The reason it is suspected and not confirmed is because Rediet has not yet been tested.
b.You would provide the following treatments for Rediet, and advise the mother how to provide the best care for her baby:
Pneumonia
- Give cotrimoxazole for five days
- Soothe the throat and relieve the cough with a safe remedy
- Advise mother to return immediately if Rediet’s condition gets worse
- Advise a follow-up visit in two days.
Diarrhoea
- Put Rediet on treatment Plan B
- Advise the mother to continue breastfeeding
- Advise mother in what circumstances she should return to the health post immediately
- Tell the mother to return for a follow-up visit in five days if Rediet is not improving.
Fever
- Treat with Coartem
- Give one dose of paracetamol in the clinic for high fever (38.5˚C or above)
- Advise mother in what circumstances she should return to the health post immediately
- Tell the mother to come for a follow-up visit in two days if Rediet’s fever persists
- If fever is present every day for more than seven days, you would have to refer Rediet for assessment.
Ear discharge
- Dry the ear by wicking
- Treat with topical Quinolone eardrops for two weeks
- Return to the health post for a follow-up visit in five days.
Suspected symptomatic HIV infection
- Give cotrimoxazole prophylaxis
- Treat HIV-related conditions if present (e.g. thrush)
- Give multivitamin supplements
- Assess Rediet’s feeding and counsel the mother as necessary
- Advise the mother about the benefits of an HIV test for Rediet and refer both of them for voluntary counselling and testing
- Advise the mother on home care
- Tell the mother to return for a follow-up visit in 14 days.
Oral thrush
- Tell the mother to paint the thrush with gentian violet 0.25% for 7 days
- Avoid feeding for 20 minutes after medication
- Check the mother’s breasts for thrush. If present treat with Nystatin or gentian violet
- Advise the mother to wash her breasts after feeds. If Rediet is bottlefed, you should advise the mother to change to a cup
- If severe, recurrent or pharyngeal thrush is present, you should consider that Rediet has symptomatic HIV
- Give paracetamol if needed for pain.
- c.Rediet’s mother needs referral for HIV counselling and testing.
As you can see from your notes and the information above, you will be providing Rediet’s mother with a lot of information. She may be confused and you need to check carefully that she has understood what she has to do to look after Rediet, and when she should return the health post.