Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Sunday, 8 March 2026, 8:56 AM
Integrated Management of newborn and Childhood Illness Module: 16. Synthesis of IMNCI for Children up to Five years: Treatment and Follow-up Care
Study Session 16 Synthesis of IMNCI for Children up to Five years: Treatment and Follow-up Care
Introduction
In Study Session 15 you learned about assessment and classification of the sick young infant and child according to the IMNCI guidelines and principles. In this final study session of the Module, you are going to learn about identifying appropriate treatments, advising about follow-up care and counselling of the mother or caregiver. As in Study Session 14, this study session will briefly review some of the materials you have already covered in the Module in relation to treatment and follow-up care. It will help you to consolidate your learning so you can be confident in providing the best possible treatment and care for the sick young infants and children who are brought to your health post.
Learning Outcomes for Study Session 16
At the end of this study session, you should be able to:
16.1 Define and use correctly all of the key words printed in bold. (SAQ 16.1)
16.2 Identify and prioritise the appropriate treatment for a sick young infant or child. (SAQ 16.1)
16.3 Determine when to refer a sick infant or child urgently to hospital. (SAQ 16.1)
16.4 List the urgent pre-referral treatments for a young infant. (SAQ 16.1)
16.5 Describe the different treatment that can be given to a sick infant or child at home. (SAQ 16.1)
16.1 Identifying treatment priorities
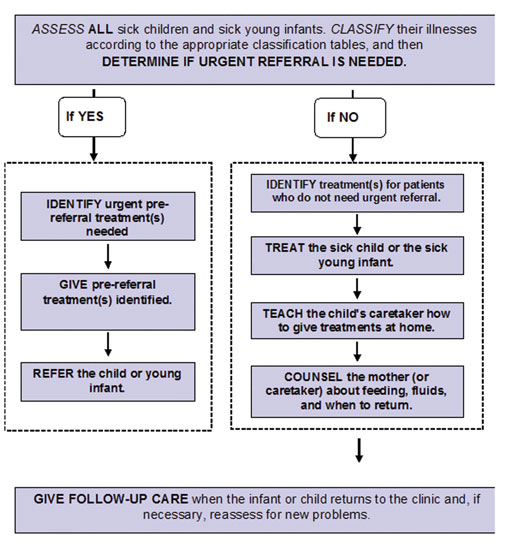
Following assessment and classification of the young infant or child’s illness, the next step is to identify any necessary treatments. In some instances, the very sick infant or child will need urgent referral to hospital for additional care. If so, you will need to start urgent treatments before the child’s departure. Figure 16.1 outlines the steps you need to follow to determine the correct IMNCI approach.
When a child has more than one classification, you must look at more than one classification table in the Assess and Classify charts to see the treatments listed. The coloured rows help you to quickly identify the correct treatment. As you should know by now:
- A classification in a pink row means that the child needs urgent attention and referral or admission for in-patient care. This is a severe classification.
- A classification in a yellow row means that the child needs an appropriate oral drug or other treatment. The treatment includes teaching the child’s caregiver how to give oral drugs or to treat local infections at home. You must also advise her about caring for the child at home and when she should return for a follow-up visit.
- A classification in a green row means the child does not need specific medical treatment such as antibiotics. You would teach the child’s caregiver how to care for the child at home. For example, you might advise her on feeding her sick child or giving fluid for diarrhoea. You would also teach her the signs indicating that the child should return immediately to the health post.
Some of the treatments may be the same for different illnesses. For example, both pneumonia and ear infection require an antibiotic. You need to notice which treatments can be used for more than one problem, and when different treatments are needed.
If an infant or child has to be referred urgently, you must decide which treatments to do before referral. Some treatments (such as wicking an ear) are not necessary before referral. The following sections will help you to identify urgent pre-referral treatments.
If referral is not possible, or if the parents refuse to take the child to the hospital, you should advise and help the family care for the child. The child may stay near the health post to be seen several times a day. Or a health worker may visit the home to help give drugs on schedule and to help give the child fluids and food.
16.2 How to determine if the sick young infant needs urgent referral
All severe classifications on the Assess and Classify chart are in the pink row and include:
- Severe pneumonia or very serious disease
- Severe dehydration
- Severe persistent diarrhoea
- Very severe febrile disease
- Severe complicated measles
- Mastoiditis
- Severe malnutrition
- Severe anaemia.
In the treatment column for these severe classifications there is an instruction ‘Refer URGENTLY to hospital’. This instruction means to refer the child to hospital immediately after giving any necessary pre-referral treatments. Do not give treatments that would unnecessarily delay referral.
- If the young infant up to two months old has possible serious bacterial infection, he or she needs urgent referral
- If the young infant has severe dehydration (and does not have possible serious bacterial infection), the infant needs rehydration with IV fluids according to Plan C and you should urgently refer the infant for IV therapy. The mother should be advised to give the young infant frequent sips of oral rehydration solution (ORS) on the way and she should continue breastfeeding.
There is one exception: for severe persistent diarrhoea, the instruction is simply to ‘Refer to hospital’. This means that referral is needed, but not as urgently. Therefore, there is time to identify treatments and give all of the treatments the child requires before referral to hospital.
Most children who have a general danger sign also have a severe classification. They will be referred for their severe classification (or possibly treated, if they have severe dehydration only). In rare instances, children may have a general danger sign or signs without a severe classification. These children should also be referred urgently.
The Assess and Classify chart does not include all of the problems that children may have. You have to decide whether a child has any other severe problem that cannot be treated at this health post. For example, a child may have a severe problem that is not covered on the chart, such as severe abdominal pain. If you cannot treat a severe problem, you should always refer the child to hospital.
16.3 Identify urgent pre-referral treatment
When a young infant or a child needs urgent referral to hospital, you must quickly identify and begin the most urgent treatments for that child before he leaves for the hospital. Urgent treatments are in bold print on the classification tables. You will give just the first dose of the relevant drugs before referral.
The following urgent pre-referral treatments are for young infants aged from birth up to two months:
- Give the first dose of intramuscular or oral antibiotics
- Advise the mother how to keep the infant warm on the way to the hospital. If the mother is familiar with wrapping her infant next to her body, this is a good way to keep him or her warm on the way to the hospital. Keeping a sick young infant warm is very important
- Treat to prevent low blood sugar
- Refer urgently to hospital with the mother giving the child frequent sips of ORS on the way. Advise the mother to continue breastfeeding.
The following urgent pre-referral treatments are for sick children aged two months up to five years:
- Give an appropriate antibiotic
- Give an appropriate antimalarial drug for severe malaria
- Give vitamin A
- Treat the child to prevent low blood sugar
- Give paracetamol for high fever (38.5°C or above) or pain from mastoiditis
- Apply tetracycline eye ointment (if clouding of the cornea or pus draining from the eye)
- Provide ORS solution so that the mother can give the child frequent sips on the way to the hospital.
The first four treatments above are critical because they can prevent serious consequences such as progression of bacterial meningitis or cerebral malaria, corneal rupture due to lack of vitamin A, or brain damage from low blood sugar. The other treatments listed are also important in order to prevent worsening of the child’s illness.
Do not delay referral to give non-urgent treatments.
Non-urgent treatments, for example wicking the ear, giving oral iron treatment, or teaching a mother how to treat a local infection, should not be done before referral. If immunizations are needed, do not give them before referral. Let hospital personnel determine when to give immunizations to avoid delaying referral.
You should write the urgent pre-referral treatments identified for each classification on the reverse side of the case recording form.
Box 16.1 below summarises the main steps to take when you refer an infant or child to hospital.
Box 16.1 Refer the infant or child
There are four steps you need to follow when referring an infant or child to hospital:
- Explain to the mother the need for referral, and get her agreement to take the child. If you suspect that she does not want to take the child, find out why.
- Calm the mother’s fears and help her resolve any problems. This might include reassuring her about the treatment her child will receive and helping her to find someone to look after any other children she has at home.
- Write a referral note for the mother to take with her to the hospital. Tell her to give it to the health worker there.
- Give the mother any supplies and instructions needed to care for her child on the way to the hospital, such as ORS and keeping her child warm.
16.4 When to return immediately
Notice that the case recording form states: ‘Advise mother when to return immediately’. You will need to teach each mother the signs that mean she should return immediately for more care for her child. You have covered each of these signs in previous study sessions.
Can you think of examples of signs that should alert a mother to return to the health post immediately with her child?
One example is if the mother notices that her child has fast or difficult breathing. Another is if the child becomes lethargic or unconscious.
16.5 Counsel the mother
As you read in the introduction to the Module, the IMNCI strategy includes working with families to help them understand how to prevent disease and illness. The strategy also involves helping the mother and family to provide effective home care and treatment for a sick young infant or child. You’ve read about the importance of good communication skills and how to teach the mother to give oral drugs and to treat infections at home. You have also learned about how to advise the mother on feeding her sick young infant or child, such as increasing fluid and food for the child during illness. Advising the mother or caregiver when to return to the health post is also important, so you are able to monitor a child’s progress.
16.6 Follow-up visits
The follow-up visit is very important. It is used to see if the treatment is working, and to give other treatment if needed. You should identify clearly what actions are included under ‘follow-up’, including when the mother should return for any other follow-up visits with her young infant or child to the health post.
16.7 The types of treatment
‘Treat’ means giving treatment in the health post, prescribing drugs or other treatments to be given at home, as well as also teaching the child’s mother or caregiver how to carry out the treatments. The Assess and Classify chart describes how to:
- Give oral drugs
- Treat local infections
- Give intramuscular drugs
- Treat the child to prevent low blood sugar
- Give extra fluid for diarrhoea and continue feeding, and
- Give follow-up care.
Treatment in the health post also involves:
- Teaching the child’s mother or caregiver to give oral drugs and/or treat local infections at home, and
- Counselling the mother or caregiver about feeding, giving fluids and when to return to the health post.
This final study session has reviewed how you provide appropriate treatment for the sick young infant and child, including critical pre-treatments when urgently referring a child to hospital. You have now completed all of the stages of IMNCI: assessment, classification and treatment of the common problems of the young infant from birth to five years.
Summary of Study Session 16
In Study Session 16, you have learned that
- A sick young infant or child needs to be referred urgently to hospital when they have a severe classification (other than severe persistent diarrhoea when there is time to give treatment to the child before referral). Children with a general danger sign usually also need to be referred urgently.
- Pre-referral treatments for a sick young infant or child are critical because they can prevent serious consequences such as progression of bacterial meningitis or brain damage. They can help prevent an illness from worsening.
- When referring an infant or child to hospital you should reassure the mother, provide her with a referral note and supplies for the journey, and help her with arrangements for any other children at home.
- Counselling the mother is an important aspect of your role.
- ‘Treatment’ refers to drugs or other treatment that you provide at the health post or that the caregiver can be taught to provide at home.
Self-Assessment Questions (SAQs) for Study Session 16
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the questions below. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
Read Case Study 16.1 and then answer the questions below.
Case Study 16.1 for SAQ 16.1
Jemel is a six-week-old infant. His weight is 4.5 kg. His axillary temperature is 37°C. His mother has brought Jemel to the health post because he has diarrhoea and a rash. It is Jemel’s first visit for this illness. The health worker checks for signs of possible bacterial infection. Jemel’s mother says that he has not had convulsions. The health worker checks his breathing and counts 55 breaths per minute. There is no chest in-drawing or grunting, the fontanelle is not bulging, and there is no pus coming from either ear. The umbilicus looks normal. Jemel does not have a fever and his movements are normal. The health worker notices some small skin pustules on Jemel. When asked about Jemel’s diarrhoea, his mother says that it began three days ago, but there is no blood in the stool.
Jemel begins crying but when his mother puts him to her breast, he stops and begins feeding normally. When she stops, he begins crying again. Jemel’s eyes look normal (not sunken). When the skin of his abdomen is pinched, it goes back slowly.
Jemel’s mother says she has no difficulty feeding him and that he breastfeeds about five times in 24 hours. She says that she gives him other drinks and food. The weight-for-age measurement shows that Jemel is not underweight for his age. However, since he is feeding fewer than eight times in 24 hours and is taking other foods and drinks, the health worker decides to assess breastfeeding. Jemel’s mother agrees to this and the health worker observes that positioning and attachment of Jemel while he is feeding are both good. When Jemel stops feeding, the health worker looks in his mouth, she does not see any ulcers or white patches.
SAQ 16.1 (tests Learning Outcomes 16.1, 16.2 and 16.3)
- a.Which Assess and Classify chart would you use for Jemel?
- b.What problems do you assess Jemel as having?
- c.How would you classify Jemel’s problems?
- d.What advice will you give to Jemel’s mother?
Answer
- a.You would use the chart for the young infant, because Jemel is less than two months old.
- b.Jemel has three problems:
- Diarrhoea
- Skin rash/pustules
- Feeding problems.
- c.You should have classified these problems as follows:
- Diarrhoea with some sign of dehydration because Jemel is irritable and restless and his skin pinch goes back slowly. Thus the classification is some dehydration
- Local bacterial infection because Jemel only has some skin pustules.
- d.You would advise Jemel’s mother as follows:
- When she should return immediately to the health post
- That she should return for a follow-up visit in two days if the skin pustules are not improving
- Give fluids to treat diarrhoea on treatment Plan B
- Advise her to increase the frequency of feeding
- Tell her to empty one breast completely before switching to the other
- Tell her to increase the frequency of feeding during and after illness
- Counsel the mother on exclusive breastfeeding.
Advise the mother how to treat Jemel’s local infections at home. Ask good checking questions to ensure that she understand the advice that you give her.