Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Sunday, 22 February 2026, 2:21 PM
Labour and Delivery Care Module: 5. Conducting a Normal Delivery
Study Session 5 Conducting a Normal Delivery
Introduction
In the previous study sessions of this Module, you were introduced to the definition, signs, symptoms and stages of labour and the use of the partograph. You also learned about care of the woman in labour. In this session, you will learn how to assist the woman in the second stage of a normal labour and how to deliver the baby. The second stage is the part of labour when the mother pushes the baby out of the uterus and down the vagina, and the baby is born. Second stage begins when the cervix is completely dilated and ends when the baby is delivered.
During the second stage, the mother’s passive control during the long hours of the first stage of labour is replaced by intense physical effort and exertion for a comparatively short period. The mother and her support person require stamina, courage and confidence from the birth attendant. A healthy outcome for the mother and her baby depends upon your competence in providing quality care and the successful partnership between you and the mother.
Learning Outcomes for Study Session 5
When you have studied this session you should be able to:
5.1 Define and use correctly all of the key words printed in bold. (SAQs 5.1, 5.2 and 5.3)
5.2 Describe the signs of second stage labour and explain what is happening to the mother and the baby as it moves down the birth canal. (SAQs 5.1 and 5.2)
5.3 Describe how you would assess if the second stage is progressing normally and identify the warning signs that sufficient progress is not being made. (SAQs 5.1 and 5.2)
5.4 Describe how you would conduct the normal delivery of a healthy baby and give it immediate newborn care. (SAQs 5.3 and 5.4)
5.5 Explain how you would support bonding between mother and newborn after the delivery. (SAQ 5.5)
5.1 Recognising the signs of second stage labour
The only positive sign in diagnosing second stage of labour is full dilatation of the cervix. The only way you can be certain the cervix is dilated all the way is to do a vaginal examination. But remember: repeated vaginal exams can cause infection. It is better not to do a vaginal exam frequently (less than 4 hours interval) unless:
- When you count the fetal heart beat it is outside the normal range (outside 120–160 beats per minute).
- There is a sudden gush of amniotic fluid, which may indicate that there is a risk for cord prolapse or placental abruption.
- You detect signs of second stage of labour beginning before the next scheduled vaginal examination. (See Box 5.1 for signs of second stage.)
With experience, you can usually tell when the mother is ready to push without doing a vaginal exam.
Box 5.1 Signs of second stage
If the mother has two or more of these signs, she is probably in second stage of labour:
- She feels an uncontrollable urge to push (she may say she needs to pass stool)
- She may hold her breath or grunt during contractions
- She starts to sweat
- Her mood changes — she may become sleepy or more focused
- Her external genitals or anus begin to bulge out during contractions
- She feels the baby’s head begin to move into the vagina
- A purple line appears between the mother’s buttocks as they spread apart from the pressure of the baby’s head.
5.1.1 What happens during second stage of labour?
During second stage, when the baby is high in the vagina, you can see the mother’s genitals bulge during contractions. Her anus may open a little. Between contractions, her genitals relax (Figure 5.1).

Each contraction (and each push from the mother) moves the baby further down. Between contractions, the mother’s uterus relaxes and pulls the baby back up a little (but not as far as it was before the contraction).
After a while, you can see a little of the baby’s head coming down the vagina during contractions. The baby moves like an ocean tide: in and out, in and out, but each time closer to birth (Figures 5.2a–d).

When the baby’s head stretches the vaginal opening to about the size of the palm of your hand (Figure 5.3), the head will stay at the opening - even between contractions. This is called crowning. Once the head is born, the rest of the body usually slips out easily with one or two pushes.
5.1.2 How does the baby move through the birth canal?
Figure 5.4 shows the movement of the baby through the birth canal. Babies move this way if they are positioned head-first, with their backs toward their mother’s bellies. But many babies do not face this way. A baby who faces the mother’s front, or who is breech, moves in a different way. Watch each birth closely to see how babies in different positions move.
5.2 Help the mother and baby have a safe birth
Continue to check the mother’s vital signs as you have been doing during the first stage of labour.

5.2.1 Check the baby’s heart beat
The baby’s heartbeat is harder to hear in second stage because the heart is usually lower in the mother’s belly. If you are experienced, you may be able to hear the baby’s heart between contractions. You can hear it best very low in the mother’s belly, near the pubic bone (Figure 5.5). It is OK for the heartbeat to be as slow as 100 beats a minute during a pushing contraction. But it should come right back up to the normal rate as soon as the contraction is over.
What is the normal fetal heatbeat?
Between 120 and 160 beats per minute.
If the baby’s heartbeat does not come back up within 1 minute, or stays slower than 100 beats a minute for more than a few minutes, the baby may be in trouble. Ask the mother to change position (to lie on her side), and check the baby’s heartbeat again. If it is still slow, ask the mother to stop pushing for a few contractions. Make sure she takes deep, long breaths so that the baby will get adequate oxygen.
5.2.2 Support the mother’s pushing

When the cervix is fully dilated, the mother’s body will push the baby out. Some healthcare providers get very excited during the pushing stage. They yell at mothers, ‘Push! Push!’ but mothers do not usually need much help to push. Their bodies push naturally, and when they are encouraged and supported, women will usually find the way to push that feels right and gets the baby out.
If a mother has difficulty pushing, do not scold or threaten her. And never insult or hit a woman to make her push. Upsetting or frightening her can slow the birth. Instead, explain how to push well (Figure 5.6). Each contraction is a new chance. Praise her for trying.
Tell the mother when you see her outer genitals bulge. Explain that this means the baby is coming down. When you see the head, let the mother touch it. This may also help her to push better.
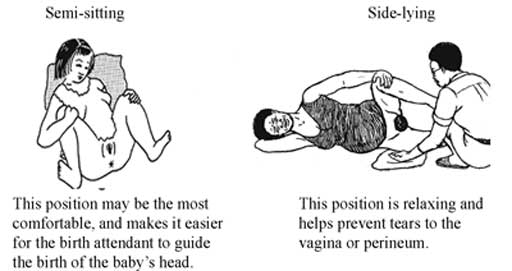
Let the mother choose the position that feels good to her. You already learned about different positions in first stage in Study Session 3. But note that it is not good for the mother to lie flat on her back during a normal birth. Lying flat can squeeze the blood vessels that bring blood to the baby and the mother, and can make the birth slower.
5.2.3 Watch for warning signs
![]() Do not apply fundal pressure to help push the baby out. Fundal pressure can cause the placenta to detach or the uterus to rupture.
Do not apply fundal pressure to help push the baby out. Fundal pressure can cause the placenta to detach or the uterus to rupture.
Watch the speed of each birth. If the birth is taking too long, take the woman to a hospital. This is one of the most important things you can do to prevent serious problems or even death of women in labour.
First babies may take a full 2 hours of strong contractions and good pushing to be born. Second and later babies usually take less than 1 hour of pushing. Watch how fast the baby’s head is moving down through the birth canal. As long as the baby continues to move down (even very slowly), and the baby’s heartbeat is normal, and the mother has strength, then the birth is normal and healthy. The mother should continue to push until the head crowns.
But pushing for a long time with no progress can cause serious problems, including fistula, uterine rupture (you will learn about this in Study Session 10 of this Module), or even death of the baby or mother. If you do not see the mother’s genitals bulging after 30 minutes of strong pushing, or if the mild bulging does not increase, the head may not be coming down. If the baby is not moving down at all after 1 hour of pushing, the mother needs help.
Therefore, refer immediately if the woman stayed (couldn’t deliver) in the second stage for more than:
- 1 hour with no good progress (multigravida woman)
- 2 hours with no good progress (primigravida).
![]() Good progress in the second stage is characterised by a marked change in level of station of the baby’s head. If you have a woman in the second stage with little or no fetal descent, or you see any signs that the baby is developing caput or excessive moulding of its skull, refer the woman to hospital or a health centre immediately.
Good progress in the second stage is characterised by a marked change in level of station of the baby’s head. If you have a woman in the second stage with little or no fetal descent, or you see any signs that the baby is developing caput or excessive moulding of its skull, refer the woman to hospital or a health centre immediately.
5.3 Conducting delivery of the baby
Your skill and judgment are crucial factors in minimising trauma for the mother and ensuring a safe delivery for the baby. These qualities are acquired through experience but certain basic principles must be applied whatever the expertise you have. These are:
- Observation of progress of the labour
- Prevention of infection
- Emotional and physical comfort of the mother
- Anticipation of normal events
- Recognition of abnormal labour or fetal distress.
5.3.1 Prevent tears in the vaginal opening
The birth of the baby’s head may tear the mother’s vaginal opening. But you can prevent tears by supporting the vagina during the birth. In some communities, circumcision of girls (also called female genital cutting) is common. This harmful traditional practice causes scars that may not stretch enough to let the baby out or the scar may tear as the baby is born.
5.3.2 Delivery of the head

Wash your hands well and put on sterile gloves and other protective materials.
Clean the perineal area using antispetic and (if you have them) put clean drapes (cloths) over the mother’s thighs.
Press one hand firmly on the perineum (the skin between the opening of the vagina and the anus). This hand will keep the baby’s chin close to its chest — making it easier for the head to come out (Figure 5.8). Use a piece of cloth or gauze to cover the mother’s anus; some faeces (stool) may be pushed out with the baby’s head.
Use your other hand to apply gentle downward pressure on the top of the baby’s head to keep the baby’s head flexed (bent downwards).
Once the head has crowned, the head is born by the extension of the face, which appears at the perineum.
Clear the baby’s nose and mouth. When the head is born, and before the rest of the body comes out, you may need to help the baby breathe by clearing its mouth and nose. If the baby has some mucus or water in its nose or mouth, wipe it gently with a clean cloth wrapped around your finger.
5.3.3 Check if the cord is around the baby’s neck
If there is a rest between the birth of the head and the birth of the shoulders, feel for the cord around the baby’s neck.
- If the cord is wrapped loosely around the neck, loosen it so it can slip over the baby’s head or shoulders.
- If the cord is very tight, or if it is wrapped around the neck more than once, try to loosen it and slip it over the head.
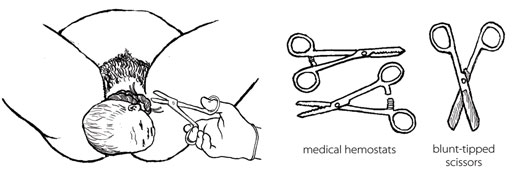
- If you cannot loosen the cord, and if the cord is preventing the baby from coming out, you may have to clamp and cut it.
If you can, use medical hemostats (clamps) and blunt-tipped scissors for clamping and cutting the cord in this situation. If you do not have them, use clean string and a new razor. Clamp or tie in two places and cut in between (Figure 5.9). Be very careful not to cut the mother or the baby’s neck.
![]() If you cut the cord before the birth of the baby, the mother must push hard and get the baby out fast. Without the cord, the baby cannot get any oxygen until he or she begins to breathe.
If you cut the cord before the birth of the baby, the mother must push hard and get the baby out fast. Without the cord, the baby cannot get any oxygen until he or she begins to breathe.
5.3.4 Delivery of the shoulders
After the baby’s head is born and he or she turns to face the mother’s leg, wait for the next contraction. Ask the mother to give a gentle push as soon as she feels the contraction. Usually, the baby’s shoulders will slip right out. To prevent tearing, try to bring out one shoulder at a time (Figure 5.10).
![]() Do not bend the baby’s head far. Guide the head — do not pull it.!
Do not bend the baby’s head far. Guide the head — do not pull it.!
5.3.5 Delivery of the baby’s body
After the shoulders are born, the rest of the body usually slides out without any trouble. Remember that new babies are wet and slippery. Be careful not to drop the baby!
Put the baby on the mother’s abdomen, dry the baby with a clean cloth and then put a new, clean blanket over him or her to keep the baby warm. Be sure the top of the baby’s head is covered with a hat or blanket. If everything seems OK, give the baby the chance to breastfeed right away. You do not have to wait until the placenta comes out or the cord is cut.
5.3.6 Cutting the cord
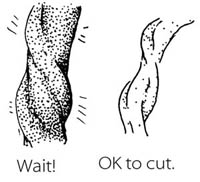
Most of the time, there is no need to hurry to cut the cord right away. Leaving the cord attached will help the baby to have enough iron in his or her blood, because some of the blood in the placenta drains along the cord and into the baby. It will also keep the baby on the mother’s belly which is the best place to be right now. Wait until the cord stops pulsing and looks like it is mostly empty of blood.
BUT if the mother is known to be HIV-infected or her HIV status is not known, it is better to cut the cord soon after you have dried the baby and made sure that he or she is warm.

Use a sterile string or sterile clamp to tightly tie or clamp the cord about two finger widths from the baby’s belly. (The baby’s risk of getting tetanus is greater when the cord is cut far from the body.) Tie a square knot (Figure 5.11).
Put another sterile string or clamp one finger from the first knot. And, if you do not have a clamp on the cord on the mother’s side, add a third knot two fingers from the second knot. Putting a double knot on the cord reduces the risk of bleeding.
Cut after the second tie (e.g. the first tie is approximately 3 cm from the baby’s abdomen and the second is approximately 5 cm). Cut after the 5 cm tie with a sterile razor blade or sterile scissors.
5.4 Immediate care of the newborn baby
Essential newborn care includes the following actions. But note that you will learn about resuscitation of the newborn who is not breathing adequately in Study Session 6.
5.4.1 Clean childbirth and cord care
Principles of cleanliness are essential in both home and health post childbirth to prevent infection to the mother and baby. These are:
- Clean your hands
- Clean the mother’s perineum
- Nothing unclean introduced vaginally
- Clean delivery surface
- Cleanliness in cord clamping and cutting.
The stump of the umbilical cord must be kept clean and dry to prevent infection. Wash it with soap and clean water only if it is soiled. Remember:
- Do not apply dressings or substances of any kind
- If the cord bleeds, re-tie it.
It usually falls off 4–7 days after birth, but until this happens, place the cord outside the nappy to prevent contamination with urine/faeces.
![]() Do not put dirt or dung on the cord stump! Dirt and dung do not protect the stump — they cause serious infections.
Do not put dirt or dung on the cord stump! Dirt and dung do not protect the stump — they cause serious infections.
5.4.2 Check the newborn
Most babies are alert and strong when they are born. Other babies start slow, but as the first few minutes pass, they breathe and move better, get stronger, and become less blue. Immediately after delivery, clear airways and stimulate the baby while drying. To see how healthy the baby is, watch for:
- Breathing: babies should start to breathe normally within seconds after birth. Babies who cry after birth are usually breathing well. But many babies breathe well and do not cry at all.
- Colour: the baby’s skin should be a normal colour – not pale or bluish.
- Muscle tone: the baby should move his or her arms and legs vigorously.
All of these things should be checked simultaneously within the first minute after birth. You will learn about this in detail in Study Session 6 of this Module.
5.4.3 Warmth and bonding
Newborn babies are at increased risk of getting extremely cold. The mother and the baby should be kept skin-to-skin contact, covered with a clean, dry blanket. This should be done immediately after the birth, even before you cut the cord.
The mother’s body will keep the baby warm, and the smell of the mother’s milk will encourage him or her to suck. Be gentle with a new baby. The first hour is the best time for the mother and baby to be together, and they should not be separated. This time together will also help to start breastfeeding as early as possible.
5.4.4 Early breastfeeding

If everything is normal after the birth, the mother should breastfeed her baby right away (Figure 5.12). She may need some help getting started. The first milk to come from the breast is yellowish and is called colostrum. Some women think that colostrum is bad for the baby and do not breastfeed in the first day after the birth. But colostrum is very important! It is full of protein and helps to protect the baby from infections.
- Breastfeeding makes the uterus contract. This helps the placenta come out, and it may help prevent heavy bleeding.
- Breastfeeding helps the baby to clear fluid from his nose and mouth and breathe more easily.
- Breastfeeding is a good way for the mother and baby to begin to know each other.
- Breastfeeding comforts the baby.
- Breastfeeding can help the mother relax and feel good about her new baby.
If the baby does not seem able to breastfeed, see if it has a lot of mucus in his or her nose. To help the mucus drain, lay the baby across the mother’s chest with its head lower than its body. Stroke the baby’s back from the waist up to the shoulders. After draining the mucus, help the mother to put the baby to the breast again. You will learn a lot more about breastfeeding in the next Module in this curriculum on Postnatal Care.
Summary of Study Session 5
In Study Session 5 you learned that:
- The second stage of labour begins when the cervix is completely dilated and ends when the baby is delivered. Close attention, skilled care and prompt action are needed from you for a safe clean birth.
- The signs of second stage are when the mother feels an uncontrollable urge to push, she holds her breath or grunts during contractions, she starts to sweat, her mood changes, her external genitals or anus begin to bulge out during contractions, she feels the baby’s head begin to move into the vagina, a purple line appears between her buttocks.
- Check the mother’s vital signs, the fetal heart beat and the descent of the baby’s head at intervals to ensure that labour is progressing normally.
- Watch for warning signs that labour is not progressing sufficiently during the second stage and take appropriate action to refer the mother.
- Support the mother’s pushing during the time of actual delivery.
- If the cord is trapped around the baby’s neck, cut it before the body is delivered — but make sure the mother pushes hard to get the baby out fast.
- Maintain cleanliness throughout the entire process of labour and delivery to prevent infection to the mother and baby.
- Keep the newborn baby warm and make sure it is breathing well.
- Initiate early breast feeding.
Self-Assessment Questions (SAQs) for Study Session 5
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the questions below Case Study 3.1. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 5.1 (tests Learning Outcomes 5.1, 5.2 and 5.3)
Which of the following statements is false? In each case, explain what is incorrect.
A Full dilatation of the cervix to 10 cm is the most important sign that the second stage of labour is beginning.
B In second stage, the mother’s genitals tend to bulge during contractions and relax between contractions.
C Crowning is the name given to the moment when the baby’s head is completely born.
D In a normal delivery, the baby moves down the birth canal facing the front of the mother’s body, with its back towards her backbone.
E While it is still in the birth canal, the baby’s heartbeat tends to get faster during a contraction.
F Let the mother choose the position that she feels most comfortable in when she gets the urge to push in the second stage of labour.
Answer
A is true. Full dilatation of the cervix to 10 cm is the most important sign that second stage of labour is beginning.
B is true. In second stage, the mother’s genitals tend to bulge during contractions and relax between contractions.
C is false. Crowning is when the top of the baby’s head stretches the vaginal opening to the size of your hand and it stays in the opening even between contractions.
D is false. In a normal delivery, the baby moves down the birth canal facing the back of the mother’s body, with its own back towards her belly.
E is false. While it is still in the birth canal, the baby’s heartbeat tends to get slower (not faster) during a contraction.
F is true. You should let the mother choose the position that she feels most comfortable in when she gets the urge to push in the second stage of labour.
SAQ 5.2 (tests Learning Outcome 5.3)
List four warning signs that second stage labour may not be progressing normally.
Answer
Warning signs that second stage may not be progressing normally include:
- Fetal heartbeat stays above or below the normal range (120-160 beats per minute) even between contractions of the mother’s uterus.
- A sudden gush of amniotic fluid leaves the vagina, which may indicate a cord prolapse or placental abruption.
- A multigravida mother has been pushing for 1 hour without the baby moving down the birth canal, or a primigravida mother has been pushing for 2 hours with no good progress.
- Baby is not descending and there are signs that it is developing caput or excessive moulding of the fetal skull.
SAQ 5.3 (tests Learning Outcome 5.4)
Imagine that the baby’s head has been born and you are waiting for the next contraction to deliver the baby’s shoulders. What should you do if you find that the umbilical cord is wrapped around the baby’s neck?
Answer
First, try to loosen the cord and slip it over the baby’s head. If you cannot loosen it and it is preventing the baby from being delivered, clamp the cord in two places (or tie it with very clean string) and cut it in between the clamps. Be careful not to cut the mother or the baby’s neck.
SAQ 5.4 (tests Learning Outcomes 5.4 and 5.5)
Rearrange the following actions into the correct order during delivery of the baby and immediately afterwards.
A Once the baby’s head is born, help it to breathe by clearing its nose and mouth.
B Wash your hands well and put on sterile gloves and other protective clothing.
C To prevent tearing of the mother’s birth vagina or perineum, deliver the baby’s shoulders one at a time.
D Press one hand firmly over the mother’s perineum.
E When the baby has been completely delivered, put it on the mother’s abdomen and dry it with a clean cloth.
F Clean the mother’s perineal area with antiseptic.
G Clamp or tie the cord in two places and cut it in between the clamps.
H Use your other hand to apply gentle downward pressure on the top of the baby’s head to keep it flexed (bent downwards).
I Cover the baby to keep it warm and give it a chance to breastfeed straight away.
J Use a piece of cloth or gauze to cover the mother’s anus in case any faeces come out with the baby.
K Check that the cord is not around the baby’s neck.
Answer
The correct sequence is as follows:
B Wash your hands well and put on sterile gloves and other protective clothing.
F Clean the mother’s perineal area with antiseptic.
D Press one hand firmly over the mother’s perineum.
J Use a piece of cloth or gauze to cover the mother’s anus in case any faeces come out with the baby.
H Use your other hand to apply gentle downward pressure on the top of the baby’s head to keep it flexed (bent downwards).
A Once the baby’s head is born, help it to breathe by clearing its nose and mouth.
K Check that the cord is not around the baby’s neck.
C To prevent tearing of the mother’s birth vagina or perineum, deliver the baby’s shoulders one at a time.
E When the baby has been completely delivered, put it on the mother’s abdomen and dry it with a clean cloth.
I Cover the baby to keep it warm and give it a chance to breastfeed straight away.
G Clamp or tie the cord in two places and cut it in between the clamps.
SAQ 5.5 (tests Learning Outcome 5.5)
What do you do to help bonding between the mother and her newborn baby?
Answer
To help bonding between the mother and her newborn baby you place the baby on the mother’s abdomen as soon as it is born, and give it an early opportunity to breastfeed. Do not separate the mother and her baby during at least the first hour after the birth.



