Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Sunday, 15 February 2026, 9:07 PM
Labour and Delivery Care Module: 9. Obstructed Labour
Study Session 9. Obstructed Labour
Introduction
Obstructed labour is a totally preventable labour complication. One of your major roles as a skilled birth attendant is to prevent the occurrence of obstructed labour in women in your community. It is highly prevalent in the rural areas of Ethiopia, particularly among women who are in labour at home for a long time.
Obstructed labour is associated with a high perinatal mortality and morbidity (fetal and newborn deaths, and disease and disability occurring around the time of the birth). It contributes to 22% of the maternal mortality in Ethiopia. This shocking figure is certainly an underestimation of the problem, because deaths due to obstructed labour are often classified under other complications (such as sepsis, postpartum haemorrhage or ruptured uterus).
In this session, you will learn how to identify the clinical signs of prolonged and obstructed labours and determine the best management. Delayed management of obstructed labour often causes fistula in surviving women, which if not treated, may make them outcasts from their community for the rest of their lives.
Learning Outcomes for Study Session 9
When you have studied this session, you should be able to:
9.1 Define and use correctly all of the key words printed in bold. (SAQs 9.2 and 9.3)
9.2 List the main causes of obstructed labour and describe how each factor contributes to the development of this complication. (SAQ 9.1)
9.3 Describe the clinical signs of obstructed labour and the common maternal and fetal complications that result from uterine obstruction. (SAQ 9.3)
9.4 Describe the management of obstructed labour and ways of preventing it through your actions. (SAQ 9.3)
9.5 Explain how social changes at community level could affect the risk of obstructed labour occurring. (SAQ 9.4)
9.1 Defining obstructed labour
Obstructed labour is the failure of the fetus to descend through the birth canal, because there is an impossible barrier (obstruction) preventing its descent despite strong uterine contractions. The obstruction usually occurs at the pelvic brim, but occasionally it may occur in the pelvic cavity or at the outlet of the pelvis. When labour is prolonged because of failure to progress, there is a high risk that the descent of the fetus will become obstructed. There is no single definition of prolonged labour, because what counts as ‘too long’ varies with the stage of labour (see Box 9.1).
Box 9.1 When is labour classed as prolonged in the different stages of labour?
- Prolonged latent phase of labour: when true labour lasts for more than about 8 hours without entering into the active first stage.
- Prolonged active phase of labour: when true labour takes more than about 12 hours without entering into the second stage.
- Prolonged second stage of labour:
- Multigravida mother: when it lasts for more than 1 hour.
- Primigravida mother: when it lasts for more than 2 hours.
Although labour can be classed as ‘prolonged’ at any stage, you should note that obstructed labour most commonly develops after the labour has entered into the second stage.
9.2 Causes of obstructed labour
As indicated above, obstructed labour is generally a second stage phenomenon, in women whose labour is prolonged. Why labour becomes prolonged or obstructed may be due to one of the ‘Ps’ (as midwives and obstetricians call them): ‘powers’, ‘passenger’ and ‘passage’.
- Powers: Inadequate power, due to poor or uncoordinated uterine contractions, is a major cause of prolonged labour. Either the uterine contractions are not strong enough to efface and dilate the cervix in the first stage of labour, or the muscular effort of the uterus is insufficient to push the baby down the birth canal during the second stage.
- Passenger: The fetus is the ‘passenger’ travelling down the birth canal. Prolonged labour may occur if the fetal head is too large to pass through the mother’s pelvis, or the fetal presentation is abnormal.
- Passage: The birth canal is the passage, so labour may be prolonged if the mother’s pelvis is too small for the baby to pass through or the pelvis has an abnormal shape, or if there is a tumour or other physical obstruction in the pelvis.
Table 9.1 summarises the mechanical causes of ‘passenger’ and ‘passage’ failure.
| Passenger | Passage |
|---|---|
Head: ● Large fetal head (big for that pelvis) ● Hydrocephalus (brain surrounded by fluid, which makes the skull swell) Presentation and position: ● Brow, face, shoulder ● Persistent malposition Twin pregnancy: ● Locked twins (locked at the neck) ● Conjoined twins (fused together with some shared organs) | Bony pelvis: ● Contracted (due to malnutrition) ● Deformed (due to trauma, polio) Soft tissue: ● Tumour in the pelvis ● Viral infection in the uterus or abdomen ● Scars (from female circumcision) |
The mechanical causes of prolonged and obstructed labour shown in Table 9.1 can be grouped into various categories: cephalopelvic disproportion; malpresentations and malpositions; or an abnormality in the fetus or the mother which obstructs the birth canal. We will look at each of these in turn in more detail.
9.2.1 Cephalopelvic disproportion (CPD)
Cephalic (pronounced ‘seff-ah-lik’) is from a Greek word meaning ‘the head’. Disproportion tells you that the size of the fetal head is different from the size of the mother’s pelvic brim.
Cephalopelvic disproportion (CPD) means it is difficult or impossible for the fetus to pass safely through the mother’s pelvis due either to a maternal pelvis that is too narrow for that fetal head, or a large fetal head relative to that mother’s pelvis (see Figure 9.1, and think back to the anatomy of the maternal pelvis and fetal skull which you learned in Study Session 6 of the Antenatal Care Module). The small (or contracted) pelvis in developing countries like Ethiopia is generally due to malnutrition in childhood persisting into adult life. Cephalopelvic disproportion cannot usually be diagnosed before the 37th week of pregnancy because before then the baby’s head has not reached birth size.
9.2.2 Abnormal presentations and multiple pregnancies

Persistent malpresentation or malposition are other major causes of obstructed labour.
Can you distinguish between these two terms and recall some abnormal fetal presentations and malpositions from Study Session 8?
Malpresentation is any presentation other than vertex (the top of the baby’s skull is the presenting part). The most common malpresentations are breech (the baby’s buttocks and/or its feet present first), and shoulder when it engages ‘shoulder first’. Malposition is when the baby is ‘head down’ (cephalic presentation), but the vertex is in the wrong position relative to the mother’s pelvis. Two of the most common malpositions result in face and brow presentations.
You also learned about multiple pregnancies in Study Session 8. Labour can be obstructed by locked twins (the two babies are ‘locked’ together at their necks when the first twin is in breech presentation and the second twin is in cephalic presentation), or conjoined twins (twins fused at the chest, head or any other site).
9.2.3 Fetal abnormalities
Some fetal abnormalities result in a fetus with an abnormally large head diameter, for example, hydrocephalus, which is due to excessive accumulation of fluid around the baby’s brain.
9.2.4 Abnormalities of the reproductive tract
A possible cause of obstructed labour is if the mother has a tumour (growth or swelling of tissue) in her pelvic cavity, or a scarred birth canal due to a severe type of female genital mutilation (‘female circumcision’). Or she may have a tight perineum (the area between the vulva and the anus), which does not stretch in order to allow the baby to pass through.
Female genital mutilation is the subject of Study Session 5 in the Module on Adolescent and Youth Reproductive Health.
9.3 Clinical signs of obstructed labour
A key sign of an obstructed labour is if the widest diameter of the fetal skull remains stationary above the pelvic brim because it is unable to descend. You should be able to detect this by careful palpation of the mother’s abdomen as the uterus relaxes and softens between contractions. However, if the uterus has gone into tonic contraction (it is continuously hard) and sits tightly moulded around the fetus, it will be very difficult to feel whether the fetus is making any progress in the birth canal. Palpation will also be very painful for the woman. In this case you will have to rely more on other signs for your diagnosis, listed below.
9.3.1 Assessment of clinical signs of obstruction
Obstructed labour is more likely to occur if:
- The labour has been prolonged (lasting more than 12 hours)
- The mother appears exhausted, anxious and weak
- Rupture of the fetal membranes and passing of amniotic fluid was premature (several hours before labour began)
- The mother has abnormal vital signs: fast pulse rate, above 100 beats/minute; low blood pressure; respiration rate above 30 breaths/minute; possibly also a raised temperature.
You should assess a woman with this labour history by doing a vaginal examination. Any of the following additional signs would suggest the presence of obstruction:
- Foul-smelling meconium draining from the mother’s vagina.
- Concentrated urine, which may contain meconium or blood.
- Oedema (swelling due to collection of fluid in the tissues) of the vulva (female external genitalia, including the labias), especially if the woman has been pushing for a long time. Vagina feels hot and dry to your gloved examining finger because of dehydration.
- Oedema of the cervix.
- A large swelling over the fetal skull can be felt (caput, Study Session 4).
- Malpresentation or malposition of the fetus.
- Poor cervical effacement (look back at Figure 1.1 in the first study session); as the result the cervix feels like an ‘empty sleeve’.
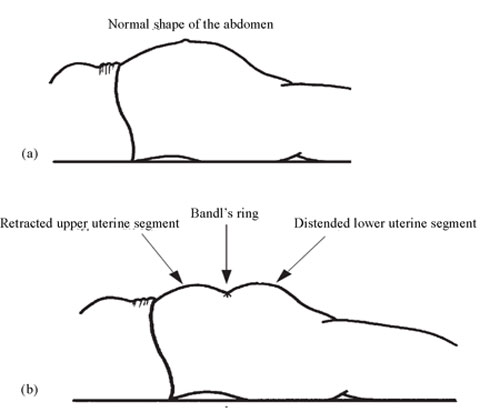
- Bandl’s ring may be seen (Figure 9.2).
9.3.2 Bandl’s ring
Bandl’s ring is the name given to the depression between the upper and lower halves of the uterus, at about the level of the umbilicus. It should not be seen or felt on abdominal examination during a normal labour (Figure 9.2a), but when it becomes visible and/or palpable (Figure 9.2b) Bandl’s ring is a late sign of obstructed labour. Above this ring is the grossly thickened, upper uterine segment which is pulled upwards (retracted) towards the mother’s ribs. Below the Bandl’s ring is the distended (swollen), dangerously thinned, lower uterine segment. The lower abdomen can be further distended by a full bladder and gas in the intestines.
9.3.3 Evidence from the partograph
You will remember from Study Session 4 that the partograph is a key tool in detecting an abnormal or prolonged labour. Obstructed labour is revealed by recordings on the partograph of the rate of cervical dilatation (which, as you know, should progress at a rate of at least 1 cm per hour) and the rate of fetal head descent. Figure 9.3(a) shows a partograph record of a normal labour with progressive cervical dilatation and fetal head descent. However in Figure 9.3(b) you can quickly see that there is evidence of a prolonged first or second stage of labour because:
- the cervical dilatation measurement has crossed the ‘Alert line’ and if no action is taken it will cross the Action line, despite strong uterine contractions; the fetal head is not descending.

![]() The cervical dilation record on the partograph should not cross the Alert and/or Action line. If this occurs you should consider this to be a prolonged and possibly obstructed labour and make an urgent referral.
The cervical dilation record on the partograph should not cross the Alert and/or Action line. If this occurs you should consider this to be a prolonged and possibly obstructed labour and make an urgent referral.
In Figure 9.3(b), how many hours after recordings began on the partograph did cervical dilation stop progressing?
The cervix stopped dilating 4 hours after the partograph record began.
In the partograph shown in Figure 9.3(b), how much time has passed since there was any sign of cervical dilatation?
The partograph shows that there was no increase in cervical diameter for the previous two and a half hours.
9.4 Management of obstructed labour
There are several things that you can do to try to relieve the obstruction if the record of cervical dilatation reaches the Alert line on the partograph, and before it approaches the Action line. The details of these procedures were taught in the Antenatal Care Module (Study Session 22) and your practical skills training, so we will only refer briefly to them here.
- If the woman has signs of shock (fast pulse and low blood pressure), prepare to give her an intravenous infusion of Normal Saline or Ringer’s Lactate to rehydrate her. Use a large (No. 18 or 20) cannula. Infuse her with 1 litre of fluids, with the flow rate running as quickly as possible, then repeat 1 litre every 20 minutes until her pulse slows to less than 90 beats per minute, and her diastolic blood pressure (when the heart relaxes after a beat) is 90 mmHg or higher.
- If you think the obstruction may be due to a very full bladder, prepare to drain it by inserting a catheter. Clean the perineal area and catheterise the mother’s bladder to drain the urine into a closed container. Relieving this obstruction may be enough to allow the baby to be born. Note that catheterisation of the bladder in a woman with obstructed labour is usually very difficult, because the urethra is also obstructed by the deeply engaged baby’s head.
![]() Refer the mother urgently to a health facility where a surgical service is available (Figure 9.4). She may need emergency delivery by caesarean section (cutting open her abdomen and uterus) to get the baby out alive and also to save her life.
Refer the mother urgently to a health facility where a surgical service is available (Figure 9.4). She may need emergency delivery by caesarean section (cutting open her abdomen and uterus) to get the baby out alive and also to save her life.
9.5 Complications resulting from obstructed labour
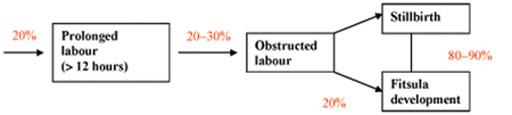
The complications of uterine obstruction for the mother and for the fetus or newborn can be very serious. Remember that uterine obstructions happen mainly because of a prolonged labour at home that was not well managed and which was not referred quickly enough. The commonest complication affecting the mother is the formation of a fistula.
9.5.1 Fistula
Fistula is an abnormal opening (usually as a result of ruptured tissues) between the:
- Vagina and the urinary bladder
- Vagina and rectum
- Vagina and urethra (the tube bringing urine from the bladder to the opening in the vulva)
- Vagina and ureter (the tube bringing urine from each kidney to the bladder).

As a result of the fistula, urine or faeces get into the vagina and exit in an uncontrolled way. A woman with a fistual can leak urine or faeces while walking, or doing any daily activities, and the waste stains her clothes and creates a bad smell (Figure 9.5). Because of these effects, her husband and family may stigmatise her or make her an outcast. You can also imagine what continuously leaking urine or faeces means at a personal level. Other consequences of fistula may include constant depression, and many physical illnesses and infections of the reproductive tract, bladder and kidneys, which may even result in the woman taking her own life.
Obstructed labour is responsible for about 20% of all cases of fistula formation (see the research study reported in Figure 9.6).
Other rare causes of fistula are congenital malformation (abnormal communication, usually between the rectum and vagina, found at birth), infection (specifically tuberculosis), trauma, forceful sexual intercourse (rape), and early age sexual intercourse.
9.5.2 Other common complications of obstructed labour
To summarise briefly, unless it is well managed, obstructed labour can also lead to the following complications in the mother:
- Postpartum haemorrhage (you will learn about this in Study Session 11 in this Module)
- Slow return of the uterus to its pre-pregnancy size
- Shock (low blood pressure and fast pulse rate)
- The small intestine becomes paralyzed and stops movement (paralytic ileus)
- Sepsis (widespread infection throughout the body)
- Death.
Complications of obstructed labour for the newborn can include:
You will learn in detail about complications affecting the newborn in the Modules on Postnatal Care and Integrated Management of Newborn and Childhood Illness
- Neonatal sepsis
- Convulsions (fits)
- Facial injury
- Severe asphyxia (life-threatening lack of oxygen)
- Death.
9.6 Prevention of obstructed labour
There are several things that a skilled birth attendant can do to prevent a prolonged labour from becoming obstructed. Additionally, certain cultural changes would also make a significant difference to the circumstances that increase the risk of obstructed labour. We now look briefly at these factors.
9.6.1 Skilled birth attendance
As we said at the beginning, obstructed labour is a major cause of maternal death worldwide, and especially in developing countries like Ethiopia. The most important intervention that could prevent this toll of death and disability is having the services of a skilled attendant at the birth. So a really important part of your role as a rural health worker is to teach the people in your community (men as well as women) about the importance of getting skilled care at every delivery. Encourage the women to come to you for advice and maintain close links with the health centres or hospital (if there is one) in your area to facilitate quick and efficient referral in cases of emergency.
9.6.2 Using the partograph
The best diagnostic tool for identifying prolonged labour is to plot the stages of labour on the partograph, at the same time as regularly assessing fetal and maternal condition (see also Study Session 4). The partograph record will give you an early warning if labour may be prolonged to the point where an obstructed uterus seems likely and referral is essential. So always remember to use it when attending any delivery.
What are the two things you must do to minimise the chances of a woman who is in labour developing a fistula?
The two things you should do are:
- Closely monitor the progress of labour using the partograph to check that the record of cervical dilatation stays on or to the left of the Alert line.
- Urgently refer the mother to a health facility if she has an obstruction (the record of cervical dilatation is approaching the Action line on the partograph), with pre-referral IV fluid infusion or bladder catheterisation if appropriate.
9.6.3 Birth preparedeness and complication readiness
As you learned in the Antenatal Care Module (Study Session 13), birth preparedness and complication readiness are the pillars of safer labour and delivery. So assist your community to organise themselves into birth preparedness teams, which have the leadership, knowledge, funding and transport to transfer mothers to the nearest health facility if there is an emergency such as obstructed labour.
9.6.4 Nutritional education
It is also important to intervene in the underlying factors that increase the risk of obstructed labour. As we said earlier, a major cause of obstructed labour is a small pelvis, which is mostly the result of poor nutrition during childhood persisting into adult life. Thus it is important to improve childhood nutrition through health education, especially for girls, to reduce the risk of prolonged and obstructed labour in later life.
9.6.5 Delaying early marriage
Early marriage is the subject of a study session in the Module on Adolescent and Youth Reproductive Health.
Another issue is early marriage. Researches in Ethiopia have shown that 50% of women, especially rural women, get married on average at around 16 years, and most of them rapidly become pregnant. This group of very young mothers is at especially high risk of obstructed labour because the pelvis has not grown sufficiently to accommodate the baby’s head. In your discussions with women, their partners and community leaders you can point out these risks of early marriage, and try to persuade them of the importance of delaying the first birth until after the woman is 18. As part of this, you will need to promote contraception (family planning methods) as a way of delaying the first pregnancy among these very young women. If unwanted pregnancy occurs, it is also important to counsel about safe abortion services (as described in the Antenatal Care Module, Part 2, Study Session 20).
Summary of Study Session 9
In Study Session 9 you have learned that:
- Obstructed labour is failure of descent of the fetus through the birth canal (pelvis) because there is an impossible barrier (obstruction) preventing its descent in spite of strong uterine contractions.
- Causes of obstructed labour are cephalopelvic disproportion (CPD), abnormal presentations, fetal abnormalities and abnormalities of the maternal reproductive tract.
- Causes of prolonged labour are abnormality in one or more of the three ‘Ps’: power, passenger and passage.
- The best diagnostic tool for you to identify prolonged labour is the partograph.
- The clinical features of obstructed labour include mother stay in labour for more than 12 hours, exhausted and unable to support herself, deranged vital signs, dehydrated, Bandl’s ring formation in the abdomen, bladder full above the symphysis pubis, big caput and big moulding, may be edematous vaginal opening.
- Common maternal complications of obstructed labour include sepsis, paralytic ileus, postpartum haemorrhage, fistula formation.
- Common fetal complications of obstructed labour are severe asphyxia, neonatal sepsis and death.
- Early referral can save the life of the woman and the baby in case of obstructed labour.
Self-Assessment Questions (SAQs) for Study Session 9
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the following questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 9.1 (tests Learning Outcome 9.2)
Write down what you understand by the three ‘Ps’ and how they cause obstructed labour.
Answer
The three ‘Ps’ (powers, passenger and passage) are a shorthand way of describing the main causes of obstructed labour. After you have checked your answers with ours (below), re-read Section 9.2 for more detail about the causes.
- Powers refers to the strength of the uterine contractions – too weak or uncoordinated and the baby is not pushed down the birth canal.
- Passenger refers to the baby – if the head is too big or deformed, or if the position or presentation is wrong, the baby will not be able to pass down the birth canal.
- Passage refers to the birth canal – if it is too small or deformed, or has blockages from tumours or scars, the baby will not be able to pass smoothly.
SAQ 9.2 (tests Learning Outcome 9.1)
Write down what you understand by the following terms:
- a.Perinatal mortality and morbidity
- b.Prolonged latent phase of labour
- c.Prolonged second stage of labour
- d.Malposition
- e.Caput
- f.Fistula
Answer
- a.Perinatal mortality and morbidity - fetal and newborn deaths, and disease and disability occurring around the time of the birth.
- b.Prolonged latent phase of labour - when true labour lasts for more than about 8 hours without entering into the active first stage.
- c.Prolonged second stage of labour - when it lasts for more than 1 hour (for multigravida mothers) and more than 2 hours (primigravida mothers).
- d.Malposition - when the baby is ‘head down’ but the vertex (the top of the baby’s skull) is in the wrong position relative to the mother’s pelvis.
- e.Caput - a large central swelling on the fetal skull.
- f.Fistula — an abnormal opening (usually resulting from a tear) between the vagina and the urinary bladder (or the rectum or urethra or ureter).
Read Case Study 9.3 and then answer the questions that follow it.
Case Study 9.1 Tadelech’s story
Tadelech lives in Mekit Woreda. The journey from village to city can take days, and she lives far from even a health post. Tadelech is 25 years old and has already delivered two children safely in the village. This is her third pregnancy. Contractions started at 40 weeks of gestation. After two days of labour Tadelech is carried on a home-made stretcher to your health post. When you examine Tadelech, finds two swellings (masses) over the abdomen, with a depression between them at about the level of the woman’s umbilicus (belly button). You also find that the baby’s head is not engaged (it is just above the pelvic brim). On vaginal examination, you estimate that Tadelech’s cervix is 8 cm dilated and the station of the fetal head is –3. Tadelech’s vagina is hot and dry and she has oedema of the vulva.
SAQ 9.3 (tests Learning Outcomes 9.1, 9.3 and 9.4)
- a.From the case study what signs do you find that indicate prolonged or obstructed labour?
- b.How do you manage Tadelech’s condition?
Answer
- a.The following signs in Tadelech’s case study suggest both prolonged and obstructed labour:
- It is clear that while Tadelech has been in the active first stage of labour for some time (dilated cervix of 8 cm), but she may actually be in a prolonged active phase of labour (when true labour lasts for more than about 8 hours without finally entering the second stage). Since you have not been monitoring her labour up to this point, you cannot be absolutely sure whether her cervix is dilating slowly, or if dilatation has completely ceased and the labour is not progressing at all.
- The two swellings (masses) above and below the depression in her abdomen known as Bandl’s ring indicate an obstructed labour.
- Furthermore, at -3 the baby’s head is not engaged, and remains above the pelvic brim; this indicates that it is not descending as you would expect it to do after Tadelech has been in labour for two days.
- The hot and dry vagina and oedema (swelling due to collection of fluid in the tissues) of the vulva are further signs of a potential obstruction.
- b.It is clear that Tadelech needs urgent referral to a health facility. Your actions should be to:
- Explain this calmly to her and her family.
- Activate the birth preparedness plan to get her transferred to a health facility as quickly as possible, together with her birth companion.
- Tadelech’s vital signs suggest she is in shock: she has a fast pulse rate and low blood pressure). Her hot and dry vagina indicates dehydration. You begin treating her for shock and dehydration by giving her an intravenous infusion (see Section 9.4) and keeping it working during the trip to the higher health facility.
- If the obstruction appears partly to be caused by an overfull bladder which the woman cannot empty in the normal way, you drain this using a catheter.
SAQ 9.4 (tests Learning Outcome 9.5)
How can you reduce the risks of a prolonged and obstructed labour for women giving birth at home?
Answer
You can reduce the risks of obstructed labour by:
- Teaching the importance of good childhood nutrition to ensure that girls’ pelvic bones have the best chance of developing to the normal size for safe delivery.
- Promoting family planning and discouraging early marriage and especially pregnancy at less than 18 years of age.
- Explaining the importance for the safety of the mother and baby of having a skilled care attendant at all deliveries.
- Assisting your community in organising birth preparedness teams so that in an emergency they can get the mother to the nearest health facility as quickly as possible.
- Always using a partograph to monitor the progress of labour.