Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Thursday, 12 February 2026, 5:07 PM
Non-Communicable Diseases, Emergency Care and Mental Health Module: 3. Cancers
Study Session 3 Cancers
Introduction
This study session is about cancers – a complex group of more than 100 non-communicable diseases. Cancers are characterised by the rapid creation of abnormal cells which grow beyond their usual boundaries, invading adjoining parts of the body and spreading to other organs. Cancers can develop in any part of the body. Over 11 million new cases of cancer are diagnosed every year around the world and at least 25 million people are currently living with the disease. In 2008, cancers were responsible for about 7.6 million deaths worldwide, accounting for 13% of all deaths in that year – more than the total dying from HIV/AIDS, tuberculosis and malaria combined.
The World Health Organization (WHO) estimates that over 70% of all cancer deaths are in low- and middle-income countries. This is mainly because specialist equipment for cancer diagnosis and treatment, and anti-cancer drugs, are very expensive and many poorer countries cannot afford enough for their populations. In Ethiopia there are no official data on cancer rates, but hospital reports suggest that cancer of the female cervix may be the leading type, followed by breast cancer.
In this study session you will learn how cancers develop from normal cells, the effects of cancers on the human body and the risk factors for cancer. Then we will focus on screening for breast and cervical cancer, and conclude with palliative care for a person who is dying with advanced cancer.
Learning Outcomes for Study Session 3
When you have studied this session, you should be able to:
3.1 Define and use correctly all of the key words printed in bold. (SAQs 3.1, 3.2, 3.4, 3.5 and 3.6)
3.2 Explain what cancer is, describe how normal cells become cancer cells and summarise their effects on the human body. (SAQs 3.1, 3.2 and 3.3)
3.3 Describe the main risk factors for cancers and the main strategies for preventing them. (SAQ 3.4)
3.4 Describe the signs and symptoms of breast cancer and cervical cancer, and explain how to educate women in your community on early detection of these cancers and what actions they should take. (SAQ 3.5)
3.5 Describe the main features of palliative care for the person who is terminally ill with advanced cancer. (SAQ 3.6)
3.1 Cells and cancer
As the definition of cancers in the Introduction stated, cancers are characterised by the rapid creation of abnormal cells. So we have to begin this study session by reminding you about what cells are and how new cells are created. All living organisms, including bacteria, protozoa, fungi, plants and animals, are organised into distinct functional and structural units termed cells. The outer surface of every cell is a cell membrane that separates the inside of the cell from the external environment. Inside the cell membrane is a jelly-like fluid (the cytoplasm, or cytosol in modern biology textbooks), and tiny structures with specific functions arranged in a particular way.
A diagram of a typical cell found in the human body is shown in Figure 3.1.

The largest structure in any cell is usually the nucleus, which contains most of the DNA in the cell. DNA (deoxyribonucleic acid) is a complex large chemical, which contains the genes of the individual. Genes are structures that determine what type of cells will develop, how they function, and how the cells in an organism are arranged, nourished, stimulated and protected in the body. Most human cells have one nucleus, but muscle cells have more than one and red blood cells have none at all. Other important structures in the cell create new molecules (e.g. proteins needed for cell growth) and others break down fuel molecules (e.g. glucose) absorbed from the surrounding environment. Cells would not be able to survive without generating energy from nutrients brought to them in the blood to fuel all the processes that go on inside the cell.
What is the difference between a normal cell and a cancer cell, in terms of cellular structures? The short answer is not much is different. Almost always the only important difference is that the nucleus is larger and may be somewhat irregular in cancer cells. The difference is not so much in their appearance, but in how cancer cells behave.
3.2 What is a cancer?
Cancers can develop in any part of the body, but they are more common in some organs than in others. For example, the top five organs in which fatal cancers developed worldwide in 2008 were:
- lungs (1.4 million deaths)
- stomach (740,000 deaths)
- liver (700,000 deaths)
- colon and rectum (610,000 deaths)
- breast (460,000 deaths).
Each of these cancers began when a single normal cell in the organ (e.g. a breast) began to divide uncontrollably, forming a solid mass of new cells (Figure 3.2). A lump of new cells growing in an inappropriate location is known as a tumour (the general public often calls it a ‘growth’). The original mass of cells is called the primary tumour to distinguish it from any ‘break-away’ tumours that may form later, if cells from the primary tumour escape and spread to other parts of the body.

Tumours can be either ‘benign’ or ‘malignant’ and this has a crucial impact on the person’s chances of survival. Most benign tumours are rarely life-threatening, though some may grow very large over a long time and eventually interfere with the functioning of a vital organ, such as the liver, heart or brain. A malignant tumour is the medical name for a cancer. Some cells in a malignant tumour break away from the original primary mass of cells and spread around the body, carried in the blood stream or lymphatic vessels. The malignant cells become lodged in distant locations (e.g. in fine capillaries in organs like the lungs or breast) and begin to generate new secondary tumours. The habit of spreading to other parts of the body is the defining characteristic of cancers, and this is what makes them life-threatening and difficult to treat.
At this point, you may be asking yourself why cancer cells grow in an uncontrolled fashion, if they contain the same types of molecules and cellular structures as normal cells? Although cancer cells are very similar to their ‘normal’ counterparts, they differ in the activity of a few genes. These genes allow cancer cells to divide and produce new cancer cells much more often than normal cells are able to divide. The cancer genes also change the behaviour of cancer cells and give them other characteristics that promote their survival and their ability to spread beyond the original primary tumour.
Table 3.1 summarises some of the important differences between normal and cancer cells.
| Normal cells | Cancer cells |
|---|---|
| Require energy to fuel chemical reactions inside the cells | Require more energy to fuel chemical reactions inside the cells |
| Divide and reproduce new cells only when appropriate signals are received | Divide and reproduce new cells continuously without needing the appropriate signals |
| Have specialised functions appropriate for their location (e.g. lung cells have special functions for their role in the lungs; breast cells have special functions for their role in the breast, etc.) | Lose part or all of their specialised functions (i.e. a cancer cell originating in the lungs no longer looks or behaves like a lung cell) |
| Age and die after a limited number of cell divisions (usually no more than eight cycles of cell division) | Survive an unlimited number of cell divisions (possibly hundreds of cycles of cell division) |
| Self-destruct and die when the appropriate signals are received (e.g. because the cell is ageing or developing abnormal characteristics) | May not self-destruct even when the appropriate signals are received, so abnormal cells survive and continue to divide |
| With some exceptions (e.g. blood cells) remain fixed in a location within tissues and organs | May escape from their original location and spread to other tissues and organs, where they can divide and reproduce new cancer cells |
3.3 The human body and cancer
Cancer cells grow aggressively and invade other neighbouring tissues. A few cancer cells rapidly become many cells (Figure 3.2b) and some cells break away from the primary tumour and settle in distant places, where they form new secondary tumours (or metastases, pronounced ‘mett-ass-tah-seez’). As a primary or secondary cancer gets larger, it releases chemical signals that cause new blood capillaries to grow into it.
Why do you think a cancer needs new blood vessels as it grows larger?
The cancer cells in the middle of the tumour need a supply of oxygen and nutrients to fuel their growth. The new blood vessels bring it to them and remove waste products such as carbon dioxide.
3.3.1 Problems in diagnosing cancers from their symptoms
The symptoms and signs of cancer are extremely diverse, depending on where in the body the tumours are growing. There are no characteristic signs and symptoms that are only due to cancers, because their effects resemble many other diseases. Some symptoms are local, affecting only the tissue or organ containing the original tumour; for example, a persistent cough may be a symptom of cancer in the lungs. Some cancers may have widespread effects all over the body; for example, cancer in the pancreas can alter the production of insulin and glucagon (Study Session 2), causing disruption to the patient’s energy supply from glucose in the diet, affecting all body functions.
In the two examples given above (cancer in the lungs and cancer in the pancreas), what other diseases have the same symptoms?
A persistent cough could be due to tuberculosis; disruption to the body’s energy supply from glucose in the diet could be due to diabetes mellitus.
There are many other examples of the difficulty in distinguishing between a cancer and another disease. For instance, cancer of the ovaries frequently leads to a lot of fluid collecting in the abdomen, causing swelling and pain which can be confused with intestinal obstruction (described in Study Session 8 later in this Module). Fluid and swelling in the abdomen presses up against the diaphragm (the muscular wall separating the lung cavity from the abdomen), restricting the ability of the person to breathe deeply. This causes the symptom of breathlessness, which can easily be confused with chronic obstructive pulmonary disease or bronchial asthma (described in Study Session 4).
3.4 Risk factors for cancers
This section will introduce you to the idea of cancer risk factors that can increase our chance of developing a cancer. Knowing what they are is helpful in educating the members of your community in how they can decrease their cancer risks by changing their behaviour. The factors that are linked with increases in cancer risk are listed in Box 3.1.
Box 3.1 Risk factors for cancer
- Age
- Cigarette smoking and chewing tobacco or khat
- Genetic factors
- Environmental risk factors, such as radiation and certain viruses
- Exposure to some industrial chemicals (e.g. insecticides)
- Lack of exercise
- Fatty diet leading to obesity
- Excessive alcohol consumption.
Which of the cancer risk factors in the above list are capable of being reduced by actions that an individual can take for themselves?
Individuals can reduce their cancer risks from all the potential causes in the above list except age, genetic factors and some environmental risk factors.
Old age is a cancer risk because as we get older our cells accumulate more damage from avoidable risks (e.g. smoking, alcohol) and unavoidable exposures in the environment, e.g. radiation from rocks, viruses that cause cancers, etc. Older cells have less ability to control their own growth, so they are more likely to become malignant and start to form a cancer. Genetic factors can also increase a person’s cancer risk; some families seem to have more than the average number of cancers arising in family members, and this is thought to be due to the existence of certain cancer-promoting genes in their cells.
The good news is that the WHO estimates that over 30% of all cancers can be prevented, and in the next section we will explain how.
3.4.1 Cancer prevention through risk reduction strategies
You can teach your community members how to reduce their risk of developing cancer by avoiding certain behaviours and habits.
Look again at the list of cancer risk factors in the previous section. What advice can you give to help people in your community to reduce their cancer risks? (In the answers below, we have added in brackets which cancers can be reduced by each strategy.)
You could advise them to:
- Avoid cigarette smoking or chewing tobacco or khat (they increase the risk of cancers of the mouth, throat, lungs, stomach, colon and bladder)
- Avoid excessive alcohol usage (which is a risk factor for cancers of the mouth, oesophagus, stomach, breast and liver)
- Eat a healthy diet containing plenty of fruits, vegetables and other high-fibre foods from plant sources like whole grains, peas and beans (this helps in reducing cancer risks in the whole of the gastrointestinal system)
- Maintain a healthy weight (this reduces the risk of many cancers, including cancers of the ovaries and breast)
- Avoid exposure to industrial chemicals by wearing personal protective clothing (this reduces the risk of lung and skin cancers, among others)
- Avoid exposure to cancer-promoting viruses (described below).
3.4.2 Prevention of cancers caused by viruses
Infection with two viruses are strongly associated with the development of specific cancers: hepatitis B virus (HBV) causes liver cancer, and human papilloma virus (HPV) causes cancer of the cervix. Both these viruses can be transmitted by unprotected sexual intercourse. HBV infection can follow from exposure to the blood of an infected person, e.g. during healthcare. Immunization against HBV is a routine part of the Expanded Programme on Immunization (the EPI) in Ethiopia; three doses are given to all infants as part of the pentavalent vaccine (pentavalent means that five different vaccines are combined in one injection). Some high-income countries also offer immunization with a vaccine against HPV, but this is not currently available in Ethiopia.
The EPI in Ethiopia is described in detail in the Immunization Module in this curriculum.
What advice would you give to women about protecting themselves from cancer of the cervix caused by HPV infection acquired during sexual intercourse?
The best way to prevent cervical cancer due to HPV is to follow the ABC rules for prevention of sexually transmitted infections (STIs):
You learned about the ABC rules in the Communicable Diseases Module, Part 3, Study Session 25.
- Abstinence (refraining from sexual intercourse)
- Be faithful (to one long-term partner)
- Condoms (correct and consistent use of condoms for all acts of sexual intercourse).
You should also teach your community that cancers that are detected early by regular self-examination are more easily treated, with a much better chance of success, than cancers where treatment begins only after a long delay. Waiting before showing a health professional a lump found anywhere in the body could mean that it is too late to save the person’s life! You should also encourage people to come for cancer screening and early detection. All types of cancer affecting men and women are found in Ethiopia, but from hospital data the most common cancers seem to be breast cancer and cancer of the cervix (cervical cancer) in women – which we describe next.
3.5 Breast cancer
The cause of most breast cancers is unknown. Genetic factors are involved in about 2% of cases, and women who are obese and/or eat a high fat diet, or drink a lot of alcohol are more at risk, but there is no clear cause in most cases. However, benign (harmless) lumps in the breast are very common, so you need to reassure women in your community that every change and every lump found in the breasts does not mean they have breast cancer. Only about one in every five women with a breast lump turns out to have cancer. The breasts are changing every month with the phases of the menstrual cycle, due to changes in the levels of the female reproductive hormones (oestrogen and progesterone), and sometimes these changes result in temporary lumps in the breast. Some women develop small painless lumps just before their menstrual period, which disappear after a few days. Sometimes a small tender cyst develops (a collection of fluid in the breast), which also disappears after a few days. If a lump is felt in the breast that remains for two weeks, it is wise to get it checked by a health professional.
3.5.1 Screening for breast cancer
![]() Advise women who find a breast lump to seek medical help – they should not to go to the traditional healers.
Advise women who find a breast lump to seek medical help – they should not to go to the traditional healers.
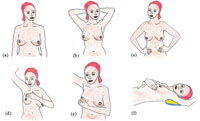
Screening refers to any method of examining an apparently healthy person to see if they have the early signs of a particular disease, which would benefit from having early treatment. Screening for breast cancer is easily carried out by women themselves. You should advise women in your community to examine their breasts once every week, using the method of breast self-examination illustrated in Figure 3.3 and described in Box 3.2.
Box 3.2 Steps in breast self-examination
The following steps relate to the diagrams in Figure 3.3 and should be carried out in this order.
- a.View the breasts with arms down at your sides. One breast is normally a little larger than the other, but do they appear about the same size and shape? Is the outline of each breast rounded and smooth, or are there any creases or dimples?
- b.Look at your breasts for the same signs as in (a), but this time with your arms raised and your hands holding each other behind your head.
- c.Repeat the visual inspection with your hands on your hips.
- d.Raise your right hand above your head; with all four fingertips of your left hand, gently press the whole of your right breast, moving your fingers to the next area and using small circular movements. Feel for any lumps or thickened tissue. Repeat with the left breast and right hand.
- e.Hold your right nipple between the thumb and first finger of your left hand; gently roll the nipple, feeling for any lumps or tenderness. Repeat with the left breast.
- f.Lie down and stretch your left arm upwards and behind your head. Use small circular pressures with the finger tips of your right hand to examine the whole breast. Repeat with the right breast and left hand.
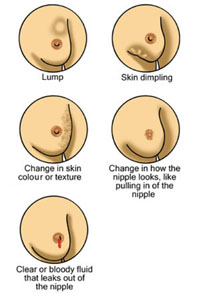
If a woman feels an unusual lump or any palpable mass in the breast, or sees a change in the appearance of the breast, she should go to the nearest health centre for further assessment and specialist treatment. The types of changes in the appearance or ‘feel’ of the breast that should alert a woman to seek medical help are shown in Figure 3.4.
There are also image screening methods for early detection of breast cancer in higher health institutions, using either low-dose X-rays (the technique is called mammography) or ultrasound imaging of the breast. In many high-income countries, all women over the age of 45 or 50 years are screened using these methods every two or three years. However, the technology is not available (or not accessible) in most low-income countries in Africa.
3.5.2 Breast cancer treatment
Breast cancer is usually treated surgically, either by removing just the cancerous tumour from the breast, or by removing the whole breast. The skin covering the breast is stitched back in place after the breast (or lump) has been removed, leaving a neat scar. Follow-up treatment may be recommended with either radiotherapy (a high-dose radiation beam is shone on the breast area), or chemotherapy with special anti-cancer drugs. This is to try to kill any cancer cells that have spread away from the original tumour in the breast, to stop them from developing into new secondary tumours elsewhere.
3.6 Cervical cancer
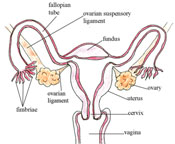
Cervical cancer refers to cancer cells growing in the tissues of the cervix – the muscular organ connecting the uterus and the vagina (Figure 3.5). Most cases of cervical cancer are caused by sexually transmitted infection with the human papilloma virus (HPV).
In low- and middle-income countries, cervical cancer is the most common female cancer and one of the leading causes of death amongst women. In Ethiopia, it is believed from hospital reports that cervical cancer is the most common of all cancers. It is usually a slow-growing cancer that may not produce symptoms in its early stages. If the cancer is advanced, it may produce symptoms including an offensive discharge and bleeding from the vagina, and pain during sexual intercourse. You should encourage any woman with these symptoms to seek urgent medical attention.
3.6.1 Cervical cancer screening
Early detection of cervical cancer can be done with a test called a Pap smear test, in which cells are gently scraped from the cervix with a blunt instrument, smeared onto a glass slide and looked at under a microscope. A special stain is applied to the cells (called the Pap stain after the doctor who invented it), which shows up the cancer cells if they are present (Figure 3.6).
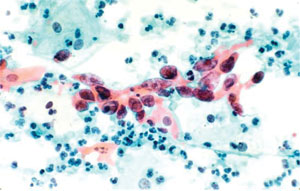
Women who are sexually active should ideally have a Pap smear test once every two or three years, but this is only available in higher-level health facilities in Ethiopia. Cervical cancer screening detects the cancer early. If effective treatment, such as surgical removal of the uterus, chemotherapy or radiation follows, it dramatically stops the progression of cervical cancer and can cure the disease completely. Advise your female clients to go to a specialised well-woman clinic if possible and have the screening test for cervical cancer.
3.7 Care for a person with advanced cancer
As you have seen in previous sections, cancer may be treatable if it is diagnosed early and depending on its type. However, some cancers are untreatable and others are diagnosed too late for treatment to be effective. If the original cancer spreads to other part of the body, the secondary tumours can damage the function of many different organs and make the patient very sick. As the cancers grow, they can interfere with processes that maintain life and the patient becomes terminally ill (i.e. expected to die within weeks).
The care given to a person who has advanced cancer (or any other chronic life-threatening condition) is referred to as palliative care. The aim of palliative care is to improve the quality of life of the sick individual and their family in the period before the death, and to help the family cope with the bereavement after the death. It involves prevention and relief of suffering, pain and other physical problems, and attention to psychosocial and spiritual issues. It focuses on supporting the patient to enjoy what remains of their life as fully as possible, and helps them and their family to manage symptoms such as pain and nausea. It also helps the relatives to cope with the overwhelming feelings they may be experiencing about losing their loved one.
The aim in palliative care is always to support the patient in their own home for as long as possible, and to involve others in the community who can give comfort to the patient and family members. In Ethiopia, an important contribution can be made by religious and spiritual leaders in the community. Don’t forget that families who are caring for a dying person also need practical help and support, for example to lift a bedridden patient to change the bedding or make the person more comfortable (Figure 3.7).

Please refer to the Communicable Diseases Module, Part 3, Study Session 30 for a detailed description of palliative care in relation to people dying from HIV/AIDS. However, all the aspects described are equally relevant to someone who is dying from cancer, heart disease or any other chronic condition – for example, chronic obstructive pulmonary disease or bronchial asthma, the subjects of the next study session.
Summary of Study Session 3
In Study Session 3, you have learned that:
- Cancers are characterised by the rapid creation of abnormal cells which grow beyond their usual boundaries, and which can invade adjoining parts of the body and spread to other organs.
- A tumour is a solid mass of new cells growing in an inappropriate location; they can be benign (harmless) or malignant (life-threatening cancers).
- The human body is made of fluids and cells of many different types with specific functions; cancers can start in cells in any organ or tissue and spread to other parts of the body.
- The symptoms and signs of cancers are easily confused with other chronic conditions, and depend on where in the body the cancer is growing; there is no characteristic defining symptom or sign of cancer.
- Age, genetic factors, cigarette smoking, chewing khat, drinking excessive alcohol, high fat diets, obesity, exposure to chemicals or viruses, and lack of exercise are some of the risk factors for cancer.
- About 30% of all cancers can be prevented by having a healthy lifestyle and avoiding tobacco, alcohol, fatty food, exposure to chemicals and unprotected sexual intercourse.
- Cervical cancer and breast cancer are the most common cancers in Ethiopia, based on hospital reports.
- There is no clear cause of breast cancer, but it can usually be treated if it is detected early enough. Teaching women about breast self-examination can save many lives through early detection and treatment.
- Cervical cancer is mainly caused by infection with the human papilloma virus (HPV); it can be prevented by following the ABC rules (Abstinence, Be faithful, Condom use). Early detection by regular Pap smear tests followed by treatment can save many lives.
- The palliative care given to someone who is terminally ill with advanced cancer includes management of symptoms such as pain and nausea, and physical, practical and spiritual support for the dying patient and their family members.
Self-Assessment Questions (SAQs) for Study Session 4
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 3.1 (tests Learning Outcomes 3.1 and 3.2)
Which of the following statements is false? In each case, explain what is incorrect.
A More people die from cancer in the world every year than from HIV/AIDS, tuberculosis and malaria combined.
B Benign tumours are not generally life-threatening.
C Malignant tumours are life-threatening because they spread and cause damage to organs and tissues all over the body.
D Cancer cells are normal cells growing in the wrong place.
E Cancer cells can multiply uncontrollably by repeated cell divisions.
F Cancer cells ‘self-destruct’ when they get too old or develop abnormal features.
Answer
A is true. More people die from cancer worldwide every year than from HIV/AIDS, tuberculosis and malaria combined.
B is true. Benign tumours are not generally life-threatening.
C is true. Malignant tumours are life-threatening because they spread and cause damage to organs and tissues all over the body.
D is false. Cancer cells are growing in the wrong place, but they are not normal cells – there are many differences (e.g. see the answer to E below).
E is true. Cancer cells can multiply uncontrollably by repeated cell divisions.
F is false. Cancer cells survive for many cell divisions because they do not ‘self-destruct’; normal cells do self-destruct when they get too old or develop abnormal features.
SAQ 3.2 (tests Learning Outcomes 3.1 and 3.2)
Suppose you are invited to give a talk about cancers in a school in your village. You want to begin by describing what cancer cells are, using words that children will understand. What will you say?
Answer
We don’t know exactly what words you would use, but you might say that normal cells increase their numbers by dividing into two cells, and then these two cells each divide again, so there are four cells, and so on. Usually normal cells can only do this a few times before they become too old and stop dividing. Cancer cells, on the other hand, can go on increasing in number by dividing into two cells, then four cells, and so on, without any control.
SAQ 3.3 (tests Learning Outcome 3.2)
Which of the following is a symptom of cancer? Explain your answer.
- a.Fever
- b.Cough
- c.Missing menstrual periods
- d.All of the above
- e.None of the above
Answer
d. is the correct answer. Cancers don’t have characteristic symptoms that indicate a cancer diagnosis. The symptoms depend on where the cancer is growing in the body and can easily be confused with the symptoms of other chronic diseases or conditions like misses menstrual periods.
SAQ 3.4 (tests Learning Outcomes 3.1 and 3.3)
Mr Abera is a 65-year-old man, who used to be a farmer, but now he doesn’t go out into the fields very often. He has smoked cigarettes for the last 25 years, he drinks alcohol almost every day, and he likes to eat a lot of fatty meat. His body mass index (BMI) is 33 (look back at Figure 2.7 in Study Session 2).
- a.What risk factors do you observe in Mr Abera's lifestyle that increase his chances of developing cancer?
- b.What advice will you give Mr Abera to decrease his risk factors?
Answer
- a.Mr Abera has a lot of cancer risk factors: very little exercise, smoking cigarettes, fatty diet, high alcohol consumption and he is obese (BMI = 33).
- b.You should advise Mr Abera to stop smoking, reduce his alcohol consumption, stop eating fatty foods and switch to eating more vegetables, fruits, peas, beans and whole grains, take more exercise, and lose weight.
SAQ 3.5 (tests Learning Outcomes 3.1 and 3.4)
What advice would you give to women who ask you about the best ways to reduce their chance of dying from breast cancer?
Answer
There is no clear cause of breast cancer that women can avoid, but it is associated with obesity and excessive drinking of alcohol, so you should advise women to avoid alcohol and becoming overweight. Early detection and treatment of breast cancer reduces the chance that women will die from the disease. The best method of early detection is regular breast self-examination to check for lumps or other abnormalities and seeking treatment if anything suspicious is found. If the facilities exist in your locality, then screening women aged over 45 years by mammography every two or three years can detect breast cancers very early.
SAQ 3.6 (tests Learning Outcomes 3.1 and 3.5)
- a.How could you help to support the spiritual needs of a cancer patient who is terminally ill in your community?
- b.What other features of palliative care could help the patient and his or her family?
Answer
- a.A good example of supporting the spiritual needs of a terminally ill patient would be to organise a meeting with family members and religious leaders or spiritual advisers at the patient’s home. It can be very comforting and uplifting to join in a religious service or blessing according to the beliefs of the family and the ill person.
- b.Other aspects of palliative care involve managing the patient’s symptoms (e.g. pain, nausea), helping to make him or her comfortable, assisting the family with practical matters, listening to their worries, and helping the sick person and family members to come to terms with the inevitable death and the grief that follows.