Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Thursday, 12 February 2026, 6:26 PM
Non-Communicable Diseases, Emergency Care and Mental Health Module: 4. Chronic Obstructive Pulmonary Disease (COPD) and Bronchial Asthma
Study Session 4 Chronic Obstructive Pulmonary Disease (COPD) and Bronchial Asthma
Introduction
Chronic obstructive pulmonary disease (COPD) and bronchial asthma are very common respiratory diseases (i.e. affecting the respiratory system) all over the world, including in Ethiopia. Patients with COPD are usually in the older age groups and have a combination of two clinical conditions – emphysema and chronic bronchitis, which will be explained in this study session. Bronchial asthma is an allergic reaction to particles getting into the lungs from the environment. Although it can affect all ages, it is the most common chronic disease among children.
According to estimates by the WHO, about 235 million people have asthma worldwide, and 210 million people have COPD. Millions more have these or other undiagnosed chronic respiratory diseases. Asthma is not often fatal, but about three million people die of COPD every year and experts predict that COPD will become the third leading cause of death worldwide by the year 2030.
In this study session, you will learn about the respiratory system, what COPD and bronchial asthma mean, and how they affect patients’ lives. We will teach you how to recognise the symptoms and signs in people in your community, and how to use screening questions for COPD to find out if a person has risk factors for developing this respiratory condition, or early signs of disease that they are not yet aware of. We will also discuss how COPD and bronchial asthma affects patient’s lives and how to prevent these diseases, so you can make an important contribution to improving the health of your community.
Learning Outcomes for Study Session 4
When you have studied this session, you should be able to:
4.1 Define and use correctly all of the key words printed in bold. (SAQs 4.1 and 4.2)
4.2 Describe the main structures in the respiratory system and how they are affected by COPD and bronchial asthma. (SAQ 4.1)
4.3 Describe the major risk factors for COPD and bronchial asthma, and the screening questions you can use to detect early signs of COPD. (SAQs 4.1, 4.2, 4.3 and 4.4)
4.4 Describe the major symptoms and signs of COPD and bronchial asthma, and how they affect patients’ lives. (SAQs 4.3 and 4.4)
4.5 Explain how you can educate people in your community to prevent or reduce the impact of COPD and bronchial asthma. (SAQs 4.2, 4.3 and 4.4)
4.1 The human respiratory system
Before we can teach you about respiratory diseases, you need to know more about the respiratory system and how it works. Look carefully at Figure 4.1. The air that you breathe in (inhale) passes down your windpipe (its medical name is trachea) into tubes in your lungs called bronchi, which branch into fine bronchioles that carry air into all parts of the lungs.
Trachea is pronounced ‘trak-ee-yah’; bronchi is pronounced ‘bronk-ee’ and bronchioles are ‘bronk-ee-oles’.
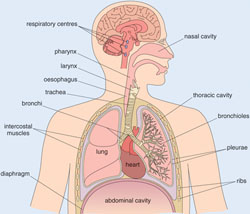
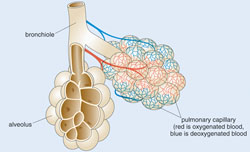
The bronchioles end in bunches of tiny round air sacs called alveoli (‘al-vee-ole-eye’, the singular is alveolus). The airways and alveoli are elastic (stretchy). When you breathe in, each air sac fills up with air like a small balloon, and when you breathe out, it gets smaller again as the air leaves.
Small blood vessels called pulmonary capillaries cover the walls of the alveoli (Figure 4.2). When air enters the air sacs, the oxygen in the air passes through the very thin walls of the alveoli into the blood in the capillaries. At the same time, carbon dioxide (a waste gas) moves from the capillaries into the alveoli and is breathed out (exhaled). This process is called gas exchange.
With this information in your mind, we can move on to describe how the respiratory system is affected in COPD first and then in bronchial asthma.
4.2 Chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease (COPD) is a progressive respiratory disease that makes it hard to breathe. The long name of this condition tells you a lot about the problem if you know what each of the words means.
What does chronic mean when applied to a disease? You should know it already from earlier study sessions in this Module.
A chronic disease is one that begins slowly, gradually gets worse over time and lasts for a long time, usually for the rest of the person’s life.
‘Obstructive’ means that the disease involves blockages (obstructions) somewhere in the body, and ‘pulmonary’ tells you that the disease affects the respiratory (or pulmonary) system.
4.2.1 The lungs in COPD
People with COPD have inflammation in their lungs that causes the production of large amounts of mucus – a clear slimy fluid secreted by cells lining the inside of the lungs. The mucus is a very good place for bacteria to grow, so lung infections are common in people with COPD. The mucus blocks the fine bronchioles and causes wheezing – squeaky breathing; you can often hear a quiet whistling or squeaking sound coming from the lungs when the person breathes in.
Can you think what effect it will have on a person whose lungs are obstructed with sticky mucus?
They won’t be able to get as much air into their lungs when they breathe, so they feel short of breath; their lungs can’t expand so easily, so they have a feeling of tightness in the chest. You might also have guessed correctly that people with COPD are always coughing, because of the irritation in their lungs and wanting to cough up the mucus.
4.2.2 Emphysema and chronic bronchitis
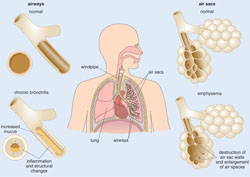
The symptoms we have just described are known as chronic bronchitis (‘bronk-eye-tuss’). Because the airways are constantly irritated and inflamed, the lining of the bronchioles becomes thicker and the space in the middle of the tube becomes smaller (see the bottom left diagram in Figure 4.3). This further restricts the amount of air that can get into and out of the lungs.
People with COPD also develop a condition called emphysema (‘em-fee-see-mah’). Persistent coughing stretches these delicate structures so much that over time they lose their elastic quality and become stiff. This means that they don’t expand as easily to let air enter. Also, the walls between many of the alveoli are destroyed by the high pressure inside the air sacs when a cough fails to dislodge a mucus obstruction. This damage leads to fewer larger air sacs instead of many tiny ones (see the bottom right diagram in Figure 4.3). If this happens, the amount of gas exchange in the lungs is reduced.
4.2.3 Risk factors for COPD
Age is a risk factor for COPD: most people who have COPD were at least 40 years old when their symptoms began. However, the main risk factor is smoking tobacco. Most people who have COPD smoke or used to smoke cigarettes. People who have a family history of COPD (older relatives who developed it) are also more likely to develop the disease if they smoke. Long-term exposure to other lung irritants is another risk factor for COPD. These include:
- Second hand-smoke from someone who is smoking tobacco in the same house every day
- Industrial air pollution (smoke, chemical fumes and dust)
- Most important of all in low-income countries – indoor smoke from cooking fires (Figure 4.4).

4.2.4 Effects of COPD on the patient’s life
As you already know, the symptoms of COPD include a persistent cough that produces large amounts of mucus (often called a ‘smoker’s cough’), shortness of breath, especially with physical activity, wheezing, chest tightness and frequent infections in the lungs (colds, pneumonia). As the disease gets worse over time, the flow of air into and out of the lungs becomes so poor that the person becomes seriously disabled by breathlessness. They may have swelling (oedema) in their ankles, feet or legs, a bluish colour on their lips due to a low blood oxygen level, and extreme shortness of breath even when sitting still. It becomes impossible to walk even a few metres.
COPD also affects the quality of life in other ways. Breathlessness stops people from doing normal physical and social activities, which further reduces their independence and contact with family, friends and neighbours. They become poor because they cannot work, and have to live with family members who may not be sympathetic to their condition. COPD can lead to a diminished role within society and the family, and the loss of intimacy in personal relationships. Many COPD sufferers eventually become housebound (unable to go out at all) and heavily dependent on family care.
![]() Immediately refer a person with COPD causing severe breathlessness; they urgently need oxygen supplied through a mask.
Immediately refer a person with COPD causing severe breathlessness; they urgently need oxygen supplied through a mask.
A person with COPD may die from heart failure, because the heart becomes exhausted by the effort of trying to pump enough oxygen around the body. Urgent medical attention is required if they are having difficulty getting enough breath for talking, their lips and fingernails turn blue due to the low oxygen level in their blood, and their heart is beating very fast.
4.2.5 COPD screening at community level
Table 4.1 is a questionnaire to help you to assess whether a person you suspect may have COPD is at risk of developing the condition. You ask the questions and fill in whether the person gives a ‘Yes’ or ‘No’ answer.
| Questions | Yes | No | |
|---|---|---|---|
| 1 | Have you been coughing a lot and producing thick mucus (sputum) coughed up from your lungs? | □ | □ |
| 2 | Have you had shortness of breath? | □ | □ |
| 3 | Have you heard wheezing from your lungs when you breathe? | □ | □ |
| 4 | Do you smoke cigarettes, or did you smoke cigarettes in the past? If not, do you live with someone who smokes cigarettes? | □ | □ |
| 5 | Does anyone in your family have asthma and/or allergies? | □ | □ |
| 6 | In your work, have you been exposed to dust or chemicals that you often breathed in? | □ | □ |
| 7 | Have you often been exposed to smoke from cooking fires inside your house? | □ | □ |
Interpretation of the results of the COPD screening questionnaire is as follows:
- If the person answers ‘yes’ to at least two out of Questions 1, 2 and 3, refer him or her to the health centre for further evaluation. It is likely that they have COPD.
- If the person answers ‘yes’ to only one of Questions 1, 2 or 3, and also has one or more of the risk factors mentioned in Questions 4 to 7, then advise them about the need for regular screening for COPD and educate them on the prevention of COPD by reducing their exposure to the risk factors.
4.2.6 Prevention of COPD
The good news is that COPD is a preventable disease! Educate people in your community how they can protect themselves from developing it by not smoking (or stopping smoking) tobacco, which is dangerous to health not only in terms of COPD.
Smoking is a risk factor for what other conditions?
Cardiovascular diseases and some cancers (e.g. lung cancers) are caused by smoking.
Fitting cooking stoves with a flue (a pipe that takes smoke and fumes out of the house, Figure 4.5) is another way to protect the lungs from smoke damage. This is also important in preventing other conditions, including respiratory infections in children (the smoke irritates their delicate lungs and creates mucus for infectious agents to grow in), and cataracts in women whose eyes are exposed to cooking smoke for many hours a day (cataracts are described in detail in Study Session 5).

4.3 What is bronchial asthma?
Bronchial asthma is a common lung disease affecting millions of people worldwide. Like COPD, it is characterised by narrowing of the airways (bronchioles) in the lungs, but there are some major differences. First, bronchial asthma is an allergic reaction to certain particles in the air, known by the general term allergens, which usually come from other animals or plants. Examples of allergens include:
- Pollen from trees, crops and flowers
- House dust mites (microscopic crawling animals that live in house dust and feed on the flakes of skin that humans shed every day)
- Animal hairs (especially domestic animals like cats, dogs and horses)
The muscles in the walls of the bronchioles constrict (become narrow) if a person with asthma breathes in an allergen that he or she has become sensitive to. Most people are not sensitive to these common allergens, so people who develop bronchial asthma may have genetic factors that make their lungs react so strongly. The narrowing of the bronchioles can begin very suddenly and is called an asthma attack. The symptoms of an asthma attack are similar to COPD and include wheezing, coughing, chest tightness and shortness of breath. If the person uses an inhaler (a device that sprays special medicine into their lungs), the narrowing of the bronchioles can usually be reversed quite quickly, so they can breathe normally again.
Can you see one big difference between asthma and COPD?
Asthma symptoms can be reversed by breathing in the correct medicine, but COPD symptoms cannot be reversed – the damage to the lungs is permanent.
![]() A person with an asthma attack should go urgently to a health centre or hospital.
A person with an asthma attack should go urgently to a health centre or hospital.
However, you should always advise people who are having an asthma attack to be taken urgently to a hospital or health centre if the symptoms do not quickly improve. Although it is unusual for people in high-income countries to die from an asthma attack, this is because most patients carry inhalers with them everywhere and can treat themselves if an attack begins. In countries like Ethiopia, where very few people with asthma have an inhaler, a severe attack can leave the person so short of breath that they die from lack of oxygen.
The factors that set off and worsen acute asthma symptoms are called ‘inducing factors’. They include smoke, atmospheric pollution, some chemicals, and bacterial and viral infections, etc. It is also believed that emotional stress and worry are inducing factors for an asthma attack. Identifying and avoiding asthma-inducing factors are essential steps in preventing a person with asthma from developing an attack of symptoms.
The effects of asthma on people’s lives has some common features with COPD, such as breathlessness restricting physical and social activities. People with asthma are often anxious about the sudden onset of an attack and they may try to avoid going to places where they may be exposed to an inducing factor or an allergen.
In the next study session, we turn to chronic conditions affecting vision and hearing.
Summary of Study Session 4
In Study Session 4, you have learned that:
- COPD is an increasingly common progressive respiratory disease; it mainly affects people after the age of about 40 years.
- COPD has two main components – chronic bronchitis and emphysema – which, over time, cause permanent irreversible damage to the lungs. The main symptoms are a persistent cough, excessive production of mucus in the lungs, shortness of breath, wheezing and chest tightness. COPD makes respiratory infections more likely.
- Smoking tobacco is the main risk factor for COPD, as well as inhaling second-hand smoke, air pollution, chemical fumes and dust from the environment or workplace, and indoor smoke from cooking fires. Stopping (or not ever) smoking and avoiding air pollution is the primary way to prevent COPD.
- Bronchial asthma is a common lung condition, in which narrowing of the airways can happen suddenly in response to inhaling an allergen, such as house dust mite, pollen or animal hairs; inducing factors that can make an attack worse are industrial pollution, respiratory infections, cigarette smoking and emotional stress.
- The symptoms of asthma are similar to those of COPD, but they are reversible if the correct medicine is inhaled. Another difference is that asthma is much more common than COPD among younger people; it is the commonest chronic condition in children worldwide.
- The effects of COPD and asthma on people’s lives share some common features, such as breathlessness restricting physical and social activities. People with advanced COPD may be unable to work or live independent lives, or walk even a few steps without becoming dangerously short of oxygen. People with asthma are often anxious about the sudden onset of an attack and they may avoid going to places where they may be exposed to an inducing factor or an allergen.
Self-Assessment Questions (SAQs) for Study Session 4
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Supporting Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module
SAQ 4.1 (tests Learning Outcomes 4.1, 4.2 and 4.3)
Which of the following statements is false? In each case, explain what is incorrect.
A COPD is a progressive disease, which affects the cardiovascular system.
B Wheezing, breathlessness and a cough with production of large amounts of mucus in the lungs are the major symptoms of COPD.
C Air entering the body travels down the oesophagus into the lungs.
D In COPD, the air sacs lose elasticity and their walls can break down.
E Bronchial asthma is mainly a disease of elderly people.
F Exposure to pollen and animal hair can cause COPD.
Answer
A is false. COPD is a disease which affects the respiratory system (not the cardiovascular system).
B is true. Wheezing, breathlessness and a cough with production of large amounts of mucus in the lungs are the major symptoms of COPD.
C is false. Air entering the body travels down the trachea (not the oesophagus) into the lungs. The oesophagus carries food and drinks from the mouth into the stomach. If you got this wrong, look back at Figure 2.2 in Study Session 2.
D is true. In COPD, the air sacs lose elasticity and their walls can break down – this condition is called emphysema.
E is false. Bronchial asthma can affect all ages, but it is much more common than COPD in young adults and it is very common in children. It is COPD that mainly affects older adults and elderly people.
F is false. Asthma (not COPD) can be caused by exposure to pollen and animal hair – but only in people who are sensitive to these allergens.
SAQ 4.2 (tests Learning Outcomes 4.1, 4.3 and 4.5)
- a.What is the most common risk factor for COPD, and what other risk factors may contribute to this condition?
- b.What advice will you give your community members to combat this risk factor, and what other diseases could be prevented by doing so?
Answer
- a.The most common risk factor for COPD is cigarette smoking; other risk factors could include second-hand tobacco smoke, air pollution, chemical fumes and dust from the environment and workplace, and indoor smoke from cooking fires – particularly if dried animal dung is used.
- b.You should always teach people in your community that smoking tobacco is dangerous to health and may cause serious illnesses, including COPD, cardiovascular diseases and lung cancer. It is also an inducing factor for bronchial asthma.
SAQ 4.3 (tests Learning Outcomes 4.3, 4.4 and 4.5)
Table 4.1 presented a questionnaire to help you to evaluate if someone has got COPD or has risk factors for COPD. Imagine that you asked Mr Sileshi all the questions in Table 4.1. He answered ‘Yes’ to Questions 4 and 6, but to all other questions he answered ‘No’.
- What advice will you give Mr Sileshi and why?
Answer
Your advice to Mr Sileshi is that he should stop smoking and make sure he wears a mask to protect his lungs from exposure to dust or chemicals during his work. Tell him that both these factors increase his risk of developing COPD, which is a permanent disabling disease that cannot be reversed. Advise him to go at once for screening for COPD if he develops any of the characteristic symptoms: cough with production of mucus, breathlessness, wheezing and tightness in the chest.
Read Case Study 4.1 and then answer the questions that follow it.
Case Study 4.1 Mihret becomes suddenly breathless
Mihret is a 25-year-old woman who comes to you complaining that when she was cooking in her house this morning, she suddenly felt very tight in her chest and had difficulty breathing. This is the first time this has happened. She went outside into the fresh air and her breathing returned to normal within about 15 minutes. You asked her if she or any family members smoke tobacco and she says ‘No’. You asked if there was smoke in the house from the cooking fire and Mihret said ‘Yes, the house is always smoky when I am cooking’.
SAQ 4.4 (tests Learning Outcomes 4.3, 4.4 and 4.5)
- a.What condition do you suspect that Mihret has experienced? Explain your answer.
- b.What could have caused it?
- c.What advice do you give her?
Answer
- a.You suspect that Mihret has experienced an attack of bronchial asthma. Your reasons are that she is too young to be developing COPD and she does not smoke tobacco or live with anyone who smokes. Also, the attack of tightness in her chest and breathlessness began suddenly and went away after about 15 minutes. COPD symptoms begin gradually over many years and they don’t get better.
- b.You noticed that her breathlessness stopped when she went outside into the fresh air, so the most likely cause of her asthma attack is the smoke from cooking inside the house, which she was breathing in.
- c.The advice you should give her is to try to avoid breathing in smoke; for example she could cook outdoors, or fit a flue to her stove or a chimney over her cooking fire to take the smoke out of the house.