Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Thursday, 12 February 2026, 5:01 PM
Non-Communicable Diseases, Emergency Care and Mental Health Module: 7. Injury-Related Emergencies and Supportive Care
Study Session 7 Injury-Related Emergencies and Supportive Care
Introduction
Emergency conditions are those that threaten a person’s life, limbs or eyesight. These are common conditions in every community all over the world. They can result in disability and death if they are not properly and urgently treated. Learning about these emergencies enables you to improve the outcome of life-supportive care, i.e. care that prevents death and reduces the risk of long-term disability in an individual who has suffered a life-threatening emergency. Note also that effective life-supportive care also protects the person’s family and his or her community from the socio-economic consequences of loss of life, limb or eyesight. These adverse outcomes reduce or destroy the productivity of the individual and affect their ability to care for their family and contribute to the community at large.
In this study session you will learn about common injury-related emergencies, how they occur, how to detect these conditions, and how to give basic life-supportive care to an injured person. You will also learn how to transfer a patient with these emergencies to a higher-level health facility for more complete specialist care. The emergencies to be covered in this session are acute injury and bleeding caused by violence, fractures, head and spinal injury, burns and multiple injuries.
Learning Outcomes for Study Session 7
When you have studied this session, you should be able to:
7.1 Define and use correctly all of the key words printed in bold. (SAQs 7.1, 7.2 and 7.4)
7.2 Describe how to stop external bleeding following an injury and how to assess a person for internal bleeding. (SAQs 7.1 and 7.4)
7.3 Identify different types of fractures and explain how to immobilise a fractured limb for transport to a health facility. (SAQs 7.1, 7.2 and 7.4)
7.4 Describe the signs and symptoms of head and spinal injuries and how to immobilise a person with such an injury for transport to a health facility. (SAQs 7.1, 7.2 and 7.4)
7.5 List the common causes and degrees of burns injuries and describe the first aid you should give for a burn. (SAQs 7.1 and 7.3)
7.1 Acute injury and violence
Acute injury refers to any physical damage to the body that occurs suddenly as a result of force. There are many ways in which a person can be injured, either unintentionally (for example, in an accidental fall or being hit by a vehicle), or intentionally through violence, war or attempted suicide. Figure 7.1 (on the next page) shows the distribution of deaths as a result of different types of injury worldwide.
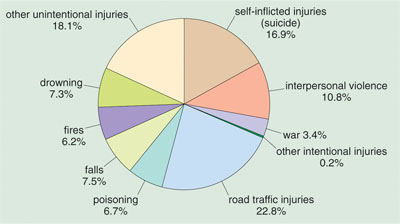
What are the top four causes of injury-related deaths shown in Figure 7.1?
They are: road traffic injuries (22.8%), other unintentional injuries (18.1%, i.e. not due to drowning, fires, falls or poisoning), suicide (16.9%), and interpersonal violence (10.8%).
Violence includes rape and is the intentional and unlawful use of force between two individuals, or a group of people, leading to physical or mental harm. It is a major public health problem worldwide – each year more than two million people die as a result of injuries caused by violence. Many millions survive their injuries, but remain permanently disabled. Many other health problems result from violent assaults, including mental disorders (see Part 2 of this Module), sexually transmitted infections (STIs), unwanted pregnancies and behavioural problems.
7.2 Bleeding
Violence caused by blows, sharp objects, bullets or sticks, and other causes of acute injury like falling or road traffic accidents, usually results in bleeding – the loss of blood from the arteries, veins and capillaries in the cardiovascular system. (Look back at Figure 1.4 in Study Session 1 of this Module to remind yourself about these blood vessels.) Based on the source of bleeding, it can be classified into:
- arterial blood (bright red, foamy and spurting in pulses)
- venous blood (darker in colour and flowing swiftly from the wound)
- capillary bleeding (red, oozing slowly from the wound at a steady rate).
Life-threatening bleeding is called haemorrhage, but you should be aware that it could be due to external or internal bleeding. External bleeding is visible and obvious, whereas internal bleeding is hidden inside the body (abdomen, chest or a limb) and is more difficult to detect. We will describe the signs of each of them in turn, and how to give life-supportive care to a person who is bleeding.
7.2.1 External bleeding
External bleeding usually occurs following a deep cut, piercing with a sharp object or a superficial bullet wound. The most serious bleeding comes rapidly spurting from an artery. This can be life-threatening if the wound is too deep and the spurt is under too much pressure to control. Minor bleeding usually stops by itself within ten minutes when a blood clot develops which blocks the bleeding vessel or wound. You should suspect life-threatening external bleeding if:
- You see blood spurting from a wound
- Bleeding fails to stop after all measures to stop bleeding have been attempted (see Box 7.1)
- The person shows signs of excessive blood loss resulting in low circulating blood volume (shock).
![]() You learned how to set up a pre-referral IV fluid infusion in Study Session 22 of the Antenatal Care Module and in your practical skills training sessions.
You learned how to set up a pre-referral IV fluid infusion in Study Session 22 of the Antenatal Care Module and in your practical skills training sessions.
Box 7.1 First aid supportive care for external bleeding
- Apply direct PRESSURE to the wound, after removing any clothing or foreign body from the wound.
- Help the person to lie down and ELEVATE the injured part above the level of the heart.
- Apply a BANDAGE to the wound; it should be just tight enough to stop the bleeding, but not so tight that it obstructs the circulation.
- Start intravenous (IV) fluid therapy with Normal Saline solution or Ringer Lactate solution if the person shows signs of shock. Transfer the patient to the nearest hospital or health centre immediately after you have begun the infusion.
What are the signs of shock following severe blood loss? (You learned about shock in the Antenatal Care and Labour and Delivery Care Modules in relation to pre- and post-partum haemorrhage.)
A person who is in shock displays weakness, confusion or an altered state of consciousness, and has a fast pulse rate (over 100 beats per minute), and low blood pressure: the diastolic pressure (the bottom number) is below 60 mmHg.
7.2.2 Internal bleeding
This type of bleeding occurs when there is a rupture of arteries or veins inside the body, for example in the abdomen. It may be caused by a kick or violent blow, a fall or another type of accident. You should remember that even though the affected person does not show any sign of bleeding externally, there may be significant damage to the internal organs, usually to the liver, spleen or thigh bone (see Section 7.3.1 below), resulting in a large amount of hidden internal bleeding. The signs that should make you suspect internal bleeding are given in Box 7.2.
Box 7.2 Signs indicating internal bleeding
Be alert for the following signs:
- Pain at the site of impact, reported by the patient
- Tenderness (feeling of pain by the affected person upon palpation)
- Rigid abdominal muscles (guarding an internal injury)
- Bleeding from other sites, e.g. from the nose or ears
- Signs of shock.
Measure the injured person’s blood pressure and pulse rate. If you suspect they have internal bleeding, lie the person down on their back. Raise their legs in an attempt to improve their blood pressure by allowing some blood from the legs to drain back towards the heart. Get someone to hold the person’s legs up for you, or use pillows to support them (Figure 7.2). Then secure an intravenous (IV) cannula in a vein in the person’s hand or arm and begin fluid infusion with a litre of Normal Saline or Ringer’s Lactate solution. Then transfer them urgently to the nearest health facility.
![]() Do not allow an injured person to eat or drink anything before their emergency transfer to a health centre or hospital!
Do not allow an injured person to eat or drink anything before their emergency transfer to a health centre or hospital!

Do not allow the person to eat or drink anything before or during the journey to a health centre or hospital. Their condition may require surgical treatment to stop the internal bleeding, and food or fluids inside the stomach can be vomited into the lungs during surgery.
7.3 Fractures
Another common consequence of accidents or violence is fracture of a bone. A fracture is where there is a break in a bone caused by a force applied to the body. The degree of damage depends on the magnitude of force applied and the strength of the bone. Fractures can happen as a result of minimal force if the bone is weak due to underlying disease (e.g. osteoporosis, or bone cancer). If you have not come across osteoporosis before, it means softening of the bones due to reduction in the concentration of calcium in the bone. This condition is more common in older persons and people who are not moving around because of other illnesses or disability.
Can you give an example from your daily life experience in a rural area of some causes of a bone fracture? Which group in a population is most likely to suffer such an injury and why?
You may have thought of a fall from a horse, tree or motorbike, a heavy blow from a stick or a bullet passing through a bone. Children and young men are the most likely members of a population to take the type of risks that lead to fractures (Figure 7.3).
7.3.1 Types of fractures
Fractures can be classified according to the following criteria:
- Closed or open fractures, depending on the presence or absence of skin perforation. In an open fracture, part of the broken bone pushes out through the person’s muscles and skin at the site of the fracture; in a closed fracture, the broken end of the bone is not exposed to view.
- Simple or complicated fractures, depending on presence (complicated) or absence (simple) of damage to soft tissues (nerves, arteries, muscles) around the site of the fracture.
Are the fractures in Figure 7.4 simple or complicated, open or closed?
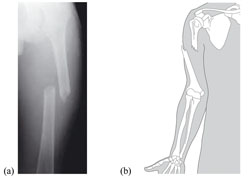 Figure 7.4 (a) X-ray picture showing a fracture of the thigh bone (femur); (b) Diagram of a fracture of the upper arm bone (humerus). (Photo (a) Courtesy of Philip Parkinson, Leeds Teaching Hospital, NHS Trust, UK; (b) The Open University, Trauma, Recovery and Repair, SDK125, Case Study 6, Figure 4.11)
Figure 7.4 (a) X-ray picture showing a fracture of the thigh bone (femur); (b) Diagram of a fracture of the upper arm bone (humerus). (Photo (a) Courtesy of Philip Parkinson, Leeds Teaching Hospital, NHS Trust, UK; (b) The Open University, Trauma, Recovery and Repair, SDK125, Case Study 6, Figure 4.11)Both fractures are complicated by the displacement of the bone into the soft tissue in the thigh or upper arm. In (a) the broken ends of the bone remain inside the soft tissue, so it is a closed fracture. In (b) the broken end of the bone has penetrated right through the soft tissue and is visible outside the surface of the arm – this is an open fracture.
7.3.2 Symptoms and signs of fractures
A person who has fractured a bone will have great pain, tenderness and abnormal movement at the site of the fracture, loss of function of the affected limb, deformity (bending), swelling and bruising. They can also have external or internal bleeding, resulting in low blood pressure and fast pulse rate. If you encounter a person who has been involved in an accident or injury with any of the above symptoms and signs, you should consider the possibility of fracture.
7.3.3 Supportive care for a bone fracture
IV fluids to replace lost blood
You have learnt that it is very important to give IV fluid to someone who has shock and low blood volume due to blood loss from an injury or other causes. The amount of blood lost in fractures depends on the type of bone affected and the severity of the fracture. The larger the size of bone fractured, you should expect more blood to be lost. The amount of internal bleeding following a fracture is estimated as:
- About 1.5 l (litres) of blood is lost following fracture of a single thigh bone
- About 1.0 l is lost following fracture of bones of the lower leg (calf).
You should also be aware that fracture of a relatively small bone may result in a much larger amount of bleeding if there is associated injury to a major blood vessel. Therefore, you should always check for signs of shock after a fracture and begin IV fluid infusion if the person’s blood pressure falls and the pulse rises. Also give the person two paracetamol tablets with a small cup of water to relieve the pain of the fracture.
Immobilising a fractured limb
The other important component of basic supportive care for a person with a fracture in a large bone (e.g. in the arm or leg) is to immobilise the injured limb before transporting the person to a health centre or hospital.
Why do you think immobilising the limb is important?
It prevents further damage to the limb, which can happen if it moves and the sharp ends of the fractured bone push out through the skin.
A fractured limb is immobilised by keeping it straight, using a rigid material called a splint, which you can make from anything like very strong cardboard, a plank of wood, or similar material. The splint should be as long as the whole arm or leg (not just the broken part) to stop movement in the joint above and below the fractured site. It is usually fixed behind the affected limb by wrapping soft cloths around the limb and the splint to bind them together (see Figure 7.5). This process is called splinting. Splinting prevents further damage, which may result in loss of the limb or disability at a later period.

Once you have applied the splint and fixed it securely, the next step is to make sure that the person reaches a hospital or health centre in a splinted state in order not to aggravate the injury further. By doing this you ensure that the patient is treated in a more specialised and complete way, which helps reduce the risk of death or disability from fracture.
7.4 Head and spinal injury
Head, neck and spinal injuries account for about 50% of the deaths immediately following injury globally. Injury to the brain or the spinal cord (the part of the nervous system that extends from the brain down inside the vertebral column or backbone) can affect the person’s ability to breathe and lead to permanent paralysis.
7.4.1 Causes, signs and symptoms of head and spinal injuries
Head injuries usually occur from blows to the brain. Injuries to the head may include fracture of the bones of the face or the skull, swelling of the brain due to inflammation and fluid collecting inside the skull after a blow to the head, or cuts to the scalp and other soft tissues around the skull. Spinal injury is when the backbone and the nerve tissue inside the spine are injured.
Certain causes of injury should alert you to possible head and spinal damage. These include a fall from any height (e.g. from a horse, motorbike, bicycle, or building), a penetrating injury to the head from a gun or knife, a heavy blow to the head, or a traffic accident (Figure 7.6). When you are called to see a person after any of these events, you should suspect the possibility of head or spinal injuries. These accidents are also common to fracture injuries. The symptoms and signs of head injury or spinal injury are given in Box 7.3.

Box 7.3 Signs of head or spinal injury
You may find these signs either separately or in combination:
- Unconsciousness or reduced level of consciousness
- Confusion in the patient’s speech or behaviour
- Visible cuts or bruises to the scalp
- Blood or fluid coming out through the nose or ears
- Unexplained headache or disturbance to sight
- Difficulty breathing
- Extreme pain or pressure in the neck, head or back
- Tingling or loss of sensation in the hands, fingers, feet or toes
- Partial or complete loss of control over any part of the body, including urination and defaecation (passing stool)
- Difficulty with balance and walking.
7.4.2 Emergency care for someone with a head or spinal injury
When you suspect an individual has a head or spinal injury, the first thing to make sure is whether the person’s airway is clear, so he or she is able to breathe. Then check for signs of blood loss and shock as described earlier. It is very important to keep the person at rest, not moving, and in the position you found him or her. When you approach the injured person, approach from the foot end, to reduce the risk of moving their head or neck and causing further damage.
After giving basic life-supportive care (described in the final section of Study Session 8), the next step is to prepare the injured person for transportation to a health facility. This primarily involves protecting and stabilising the spinal cord in the neck, so that it cannot move and cause more serious damage, which may lead to death or permanent disability. Apply sandbags or pillows on each side and at the back of the neck to immobilise the person’s head and neck (Figure 7.7).

7.5 Burns injuries
Burns are such a common accident that you are sure to have seen someone suffering from a burn in your village. A burn is a severe form of injury which causes significant soft tissue damage, as well as changes affecting blood volume (fluid balance). By fluid balance it is meant that people with a major burn will develop shock as a result of evaporation of body fluids from the burn surface; this reduces their blood volume even though they are not bleeding. While most burns are minor and do not require hospitalisation, extensive burns are a life-threatening emergency. You should also know that the very young and the very old do not tolerate burns well or respond so well to treatment (Figure 7.8).

7.5.1 Common causes of burns
What are the common causes of burns in your village? Do they include the situations listed in Box 7.4, which are common all over the world?
Box 7.4 Common causes of burns
- Fire and flame
- Boiling fluid (scald injury)
- Acid (chemical burn)
- Electrical burn from faulty electrical equipment.
All these causes of burns result in destruction of the skin and varying layers of the soft tissue underneath. In burns injuries, the depth of the burn depends upon the temperature of the heat source and how long the body was in contact with it. The most common sites of a burn are the hands, arms, legs and feet.
Other important burns-related conditions that you should know about are burns involving the chest, face and inhalation (breathing in) of a large amount of smoke and heat. These conditions require urgent special attention at a health facility due to the risk that they will interfere with breathing. You should suspect a respiratory tract burn when the person inhales a large amount of smoke and heat as a result of being trapped in a closed space during a fire.
7.5.2 Classification of burns
Most burns injuries are minor and do not require hospitalisation. Factors that affect the severity of a burn include the age of the person, the presence of burns to the face or respiratory tract (lungs), and of course, the depth of the burn. Burns can be classified into first degree (superficial), second degree (intermediate), or third degree (full-thickness) depending on the depth of injury to the skin and underlying structures.
First degree burns
In a first degree burn the injury is restricted to the most superficial layer of the skin. Nerve endings in this layer become exposed and the burn surface is painful. Blister formation is common. This kind of burn heals spontaneously within ten days if protected from infection by gentle washing regularly and sometimes covering with a clean sheet of gauze or cloth.
Second degree burns
In a second degree burn the skin is injured to a deeper layer than the first degree burn. Because of the extent of the damage, the burnt surface appears to you whitish (bloodless) and is painless as compared to the first degree burn. This is because the nerve endings that transmit the feeling of pain to the brain have been destroyed. Healing takes longer (three to four weeks) and occurs by scar formation.
Third degree burns
In a full-thickness or third degree burn, the whole layer of the skin and subcutaneous tissue is destroyed and the muscles, tendons or the bone underneath the skin may be visible. Healing occurs very slowly. Severe scarring is unavoidable. If third degree burns cover a large area of the body, death usually results from dehydration as fluids evaporate through the burnt skin, and infection enters through the burn.
7.5.3 Emergency care for people with serious burns
If first aid has not already been given, flush the burn thoroughly with clean cold water. This helps to prevent further damage. You should also remove all burned clothing from the body of the person. If the burn area is limited, immerse the site in cold water for about 30 minutes. This again helps reduce pain, swelling (oedema) caused by tissue fluid flooding into the damaged area, and inflammation.
The other important aspect of immediate care in a major burn is prevention of heat loss from the body, especially in children, if a large area of the body has been burnt, or there are third degree burns. Hypothermia is defined as excessive cooling of a person or reduction of body temperature which, if not prevented, may result in the body systems stopping their normal function. To prevent hypothermia from happening you should apply clean wraps around the burnt area or the whole patient.
Why should you immerse or flush a burnt part of the body with cold water?
This is because of three main reasons:
- It reduces further tissue damage
- It reduces swelling/oedema and inflammation
- It also helps to reduce pain.
 After giving immediate first aid, urgently refer a person with a severe burn to a higher health facility for specialist care and treatment.
After giving immediate first aid, urgently refer a person with a severe burn to a higher health facility for specialist care and treatment.
What you have studied so far is only the first aid treatment for a severe burn. Once you have done this, refer individuals with severe burns to a hospital or health centre for specialist care. This must be done as soon as possible. The first six hours following a burns injury are critical for recovery.
7.6 Multiple injuries, emergency transport and referral
In the previous sections of this study session, we have described how to treat bleeding, fractures, head and spinal injuries and burns when they occur separately. However, in many accidents or after a violent attack, the patient is often suffering the combined effects of multiple injuries – several injuries at the same time. Knowing that multiple injuries are likely to happen in the same individual helps you to remember that you must not concentrate only on one type of injury – you must focus on all the multiple effects and your first priority is to address whatever is most threatening to their life. Delivery of basic life-supportive care is taught at the end of Study Session 8, after you have learned about emergency conditions that are not due to injuries.
Remember that most health emergencies will require rapid referral to a health centre or hospital. As a Health Extension Practitioner, you have an important responsibility in your community to prepare an emergency transport plan, which identifies individuals with vehicles (car, truck, gharry, etc.) who can get injured people to a health facility as quickly as possible. As in all referrals for whatever cause, you must write a clear referral note, describing the patient’s name, address, age, etc., the circumstances in which the injury or other emergency occurred, your assessment of their condition and any actions you have taken.
Summary of Study Session 7
In Study Session 7, you have learned that:
- Injury due to accidents and violence is a common cause of emergency conditions which threaten life, limb and eyesight; it is a common problem globally and at national level.
- The effect of an injury is not limited to immediate life-threatening emergency conditions; it can persist way beyond the immediate injury period in the form of profound economic, mental health and behavioural problems.
- Violent assaults such as rape can lead to sexually transmitted infections (STIs) and unwanted pregnancies
- Injury often results in life-threatening internal or external bleeding. Try to stop external bleeding with pressure and bandages. Start pre-referral IV fluid therapy in cases of shock.
- Fractures (open or closed), head and spinal injuries must be attended to urgently in order to prevent loss of limbs, paralysis and permanent disability. Immobilisation of the injured part during transport to a health facility is essential life-supportive care.
- Flame, hot fluid, chemicals and electricity are the common causes of first, second or third degree burns, depending on the depth of skin and soft tissue affected. Flushing a burn with cold water is an important element of first aid care in order to minimise the extent of damage and reduce pain.
- Remember to develop an emergency transport plan to get an injured person to a health centre or hospital quickly. Write a clear referral note with all the patient’s details, your assessment of the injury and any actions you have taken.
Self-Assessment Questions (SAQs) for Study Session 7
Now that you have completed this session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 7.1 (tests Learning Outcomes 7.1, 7.2, 7.3, 7.4 and 7.5)
Which of the following statements is false? In each case, say what is incorrect.
A If a wound is bleeding externally, you apply pressure to it, elevate the bleeding part and bandage it tightly enough to stop the bleeding.
B A person who has internal bleeding will have a slow pulse and rapidly rising blood pressure.
C Pain in the abdomen and rigid abdominal muscles are signs of a possible internal injury.
D Bleeding from the nose, ears or scalp and confusion in the patient’s speech or behaviour are signs of possible head injury.
E Swelling and internal bleeding are signs of an open fracture.
F A person with a first degree burn is at risk of dying from dehydration and infection.
Answer
A is true. If a wound is bleeding externally, you apply pressure to it, elevate the bleeding part and bandage it tightly enough to stop the bleeding.
B is false. A person who has internal bleeding will have a rapid pulse and falling blood pressure.
C is true. Pain in the abdomen and rigid abdominal muscles are signs of a possible internal injury.
D is true. Bleeding from the nose, ears or scalp and confusion in the patient’s speech or behaviour are signs of possible head injury.
E is false. An open fracture means the broken bone is sticking out through the skin at the fracture site. There is also likely to be swelling and internal bleeding, but this also occurs in closed fractures.
F is false. A person with a third degree burn is at risk of dying from dehydration and infection if the burned area is extensive. First degree burns are superficial and heal within a few days.
SAQ 7.2 (tests Learning Outcomes 7.1, 7.3 and 7.4)
- a.How would you immobilise (i) a fractured limb and (ii) a neck or spinal injury?
- b.What is the purpose of immobilisation and what outcomes could it prevent?
Answer
- a.Fracture immobilisation is done by keeping the injured limb straight using a rigid material called a splint, which is bandaged to the broken limb to keep it still. The splint should be long enough to immobilise the whole of the limb above and below the fracture. Immobilisation of spinal injuries is done by applying sand-bags or pillows on each side and at the back of the neck to stop the head and neck from moving during transportation to a health facility.
- b.The purpose of immobilising a fracture or spinal injury is to prevent further injury or damage to the patient, which could occur if the broken parts are moved during transport to a health facility. In the case of a fracture, further damage to the broken limb could lead to loss of the limb or difficulty in using the limb. In the case of spinal injury, further damage could cause death or permanent disability, e.g. paralysis.
SAQ 7.3 (tests Learning Outcome 7.5)
What are the steps of emergency first aid care for a severe burn?
Answer
The first thing you should do is to cool the burn by flushing it with cold water and if possible immerse the burned part in cold water. Gently remove any clothing that is touching the burned area. Cover the wound with a sterile dressing or (if one is not available) a very clean cloth. If the burn is extensive or deep, transport the person to a health centre or hospital for specialist care.
Read Case Study 7.1 about Mr. Samuel and respond to the question that follows it.
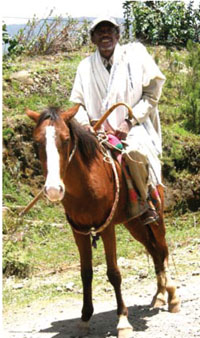
Case Study 7.1 Mr. Samuel has a horse-riding accident
Mr Samuel is a 54-year-old farmer who was heading home from his farm (Figure 7.9). He was riding fast when his horse stumbled and fell into a ditch, throwing Mr Samuel against a rock on the ground. He was found by some villagers, who called you to see him. When you reach the place, you see that he is lying on the ground and he seems unable to get up. You can’t see any blood on his clothes.
SAQ 7.4 (tests Learning Outcomes 7.1, 7.2, 7.3 and 7.4)
What possible injuries could Mr Samuel have suffered?
Answer
Mr Samuel seems unable to get up so he may have fractured a limb, or suffered head and spinal injuries; he may also have internal bleeding. In other words, he could have multiple injuries which happened all at the same time when he fell from the horse and hit the rock.