Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Thursday, 12 February 2026, 5:04 PM
Non-Communicable Diseases, Emergency Care and Mental Health Module: 8. Gastrointestinal Emergencies, Choking and Basic Life Support Techniques
Study Session 8 Gastrointestinal Emergencies, Choking and Basic Life Support Techniques
Introduction
Non-injury emergencies are life-threatening conditions such as appendicitis and intestinal obstruction, poisoning and choking. They are certain to occur in your community and require your urgent help in supporting the life of affected people before they are transferred to a higher health facility for specialised treatment. In this study session you will learn about the most common non-injury emergencies, and how to detect those which, if unattended, might result in death. You will also learn how to prepare patients with these conditions for referral.
This study session ends with a section on basic life support techniques, which applies to patients with non-injury emergencies and also to conditions such as airway obstruction, bleeding, or multiple injuries as described previously in Study Session 7.
Learning Outcomes for Study Session 8
When you have studied this session, you should be able to:
8.1 Define and use correctly all of the key terms printed in bold. (SAQs 8.1, 8.2, 8.3, 8.4 and 8.5)
8.2 Describe the signs and symptoms of appendicitis and intestinal obstruction, and explain how to give life-supportive care for these emergency conditions. (SAQs 8.1 and 8.2)
8.3 List the routes of entry of poison into the body, describe the signs and symptoms of poisoning, and explain how to give life-supportive care to someone who is poisoned. (SAQs 8.3 and 8.4)
8.4 Describe the signs and symptoms of choking and explain how to give life-supportive care to someone who is choking. (SAQ 8.5)
8.5 Outline how to give emergency life-supportive care, using the ABCDE-T approach. (SAQs 8.2, 8.3, 8.4 and 8.5)
8.1 Gastrointestinal emergencies
Gastrointestinal emergencies are acute abdominal conditions characterised by pain in the abdomen, which began in the last seven days (not longer ago) and which is severe enough to affect the daily life and activities of the individual. A condition is described as acute if it begins suddenly and gets worse over a short period of time. An acute emergency is one that rapidly becomes life-threatening.
If abdominal pain has lasted for more than seven days it is called chronic abdominal pain and the affected person should be referred as soon as possible.
Can you suggest a possible cause of chronic abdominal pain? (Think back to Study Session 3.)
It may be due to a cancer somewhere in the abdomen, e.g. in the stomach, intestines, liver, spleen, pancreas or reproductive organs.
The two most common causes of gastrointestinal emergencies are appendicitis and intestinal obstruction, described below. Note that they have overlapping symptoms and signs, making their distinction difficult. In addition, the symptoms are not always typical in very old or very young people and this uncertainty often causes delay in diagnosis. Delay in starting treatment contributes to the more severe effects of these conditions in older or younger age groups, and their bodies have more limited ability to repair afterwards.
8.1.1 Appendicitis
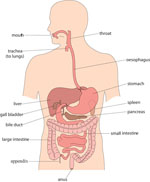
Appendicitis is an acute condition which occurs as a result of inflammation of the appendix. The appendix is a small tube, closed at one end, which is found at the junction between the small and the large intestine (Figure 8.1). It has no known function in digestion. The appendix can become inflamed when pieces of food get trapped in it and infection develops in the rotting food.
Acute appendicitis commonly affects adolescents and young adults, but it can occur at any age. The typical symptoms and signs that make you suspect someone has acute appendicitis include:
- Pain around the navel (belly button) which later shifts to the lower abdomen, particularly on the right side. Notice in Figure 8.1 that the appendix is on the lower right side of the abdomen.
- Fever (body temperature above 37.5ºC)
- Nausea and vomiting
- Tenderness and rigidity of the abdominal muscles guarding the affected internal organs.
If you see a person with the above symptoms which have only recently begun, refer them to a health centre or hospital for assessment. You can give two paracetamol tablets with a small cup of water to help to relieve the pain, but tell the person not to eat or drink anything else until they have been seen by a doctor. If they have acute appendicitis, the appendix will have to be removed surgically by an operation to the abdomen. Reassure the patient that this type of surgery is straightforward and they will soon recover afterwards.
Can you remember why eating or drinking is not advised for a patient who is being referred for possible surgery?
You learned in Study Session 7 that the reason the stomach should be empty before surgery is to avoid the patient vomiting food or drink and obstructing their lungs when they are unconscious due to the anaesthetic.
If the affected person comes to you several days after the onset of appendicitis, the infection may have spread outside the appendix into the rest of the abdomen. Widespread infection in the abdomen is called abdominal sepsis and it can lead to septic shock, which is manifested by low and falling blood pressure, fast pulse, rapid respiration, fever and extreme abdominal pain. Without urgent surgery to remove the inflamed appendix and antibiotic treatment for the infection, a person with septic shock will soon die. If you have been trained to do so, insert an intravenous (IV) cannula into a blood vessel in the person’s arm and begin fluid therapy with a litre of Normal Saline or Ringer’s Lactate solution. Make sure the fluid infusion continues during the journey to a health centre or hospital.
![]() Refer a person with acute abdominal pain urgently! If they develop septic shock, death will soon follow.
Refer a person with acute abdominal pain urgently! If they develop septic shock, death will soon follow.
8.1.2 Intestinal obstruction
![]() If you suspect an intestinal obstruction, refer the patient immediately.
If you suspect an intestinal obstruction, refer the patient immediately.
Intestinal obstruction means a blockage somewhere in the gastrointestinal system (look back at Figure 8.1) and is another important cause of acute abdominal pain. It can be caused by either mechanical or non-mechanical obstructions. A mechanical obstruction means that something is physically blocking the digestive tract, preventing the flow of food through the intestine.In the case of non-mechanical obstruction, the digestive tract is not directly blocked, but food does not move forwards because of some problem in the muscular action of the intestine itself, which normally pushes the food along. Without special tests, it is difficult to diagnose whether a blockage is mechanical or non-mechanical. In both cases, the patient will require immediate referral to a higher health facility.
The signs and symptoms of intestinal obstruction are:
- Abdominal pain, which may be throughout the abdomen
- Nausea and vomiting
- Constipation (absence of gas and faeces)
- Abdominal distension (swollen abdomen)
- Tenderness and rigidity of the abdominal muscles guarding the internal organs
- Shock (in advanced cases).
The pre-referral actions described above for acute appendicitis also apply to a patient with suspected intestinal obstruction.
8.2 Poisoning
A poison (also called a toxin) is a naturally occurring or manufactured substance which, if taken into the body in sufficient quantity, causes temporary or permanent damage. The common poisons that people may have in their homes include medical drugs, alcohol, household cleaning chemicals, kerosene and pesticides. You may be surprised when we say to you that medical drugs are ‘poisons’, but remember that medicines must be taken in the prescribed dosages and only by the person who has been prescribed that drug. All medical drugs are toxic if the dose is exceeded, or if they are taken by the wrong person – for example, the adult dose of a drug could seriously harm a child. In the Amharic language, this is expressed in the saying that ‘even honey is sour if too much is taken’.
Can you think of some naturally occurring poisons?
You may have thought of poisonous plants, the bite or sting of poisonous animals (e.g. snakes, scorpions), and the toxins released by certain bacteria when they get into the body.
There are four different ways that a poison can get into the body. It can be:
- Ingested by swallowing, e.g. medicines, household chemicals, etc.
- Inhaled in the breath, e.g. when spraying houses or water collections with chemicals to kill insects or other vectors of communicable diseases (Figure 8.2); or inhaled carbon monoxide gas, which is an invisible poison found in the fumes formed by burning charcoal
- Injected, e.g. when bitten by a snake or injected by a needle
- Absorbed when the poison comes into contact with the skin and passes through it into the body, e.g. when a person is splashed with a chemical that kills insects (insecticide) or weed killer.

You should also know that the effects of poisoning are more serious when the person poisoned is very young, very old, or in poor health. This makes early diagnosis especially important in these groups.
8.2.1 Signs and symptoms of poisoning
The symptoms of poisoning partly depend on the route of entry into the body. Common symptoms include nausea, vomiting, abdominal pain, difficulty in breathing, headaches, changes in heart rate pattern (fast, slow or irregular), watering of the eyes, confusion, and impaired consciousness. If the exposure has been to the skin, the person may also complain of swelling, rashes, redness and itching of the skin.
You should suspect poisoning if there are empty containers for medicines or chemicals near the poisoned person, or there is a strange smell present (for example, of bleach or kerosene). So, in considering poisoning, you should look around where the person became ill and ask questions to gather possible clues. Take the containers with you to show the doctor when you transport the patient to the nearest health facility. Knowing what has been swallowed will help the medical staff to know what action to take to neutralise the poison.
8.2.2 Suicide by poisoning
Drinking berekina (bleach, Figure 8.3) or kerosene is a common method of trying to commit suicide, i.e. the person intended to purposefully kill themselves. If you suspect suicide by poisoning, deal with the immediate emergency as you would for any other poisoning event. If the person survives, they will need additional support when they return to the community to resolve the cause of the mental distress that pushed them to attempt suicide. Refer to Study Session 10 of this Module for a detailed discussion of the signs that may give you early warning that someone is thinking of trying to kill themselves. Part 2 of this Module describes a wide range of mental health problems and how to deal with them at community level.

8.2.3 First aid for a person with poisoning
![]() Go with a person who has been poisoned – they could stop breathing on the way to the health facility and you may be able to save their life on the journey.
Go with a person who has been poisoned – they could stop breathing on the way to the health facility and you may be able to save their life on the journey.
If you find a person who has been poisoned accidentally or intentionally, apply basic life-supportive care using the ABCDE-T approach (described in Section 8.4.1 of this study session). If the poison has been absorbed through the skin, remove any contaminated clothing and wash the body with water and soap. If a chemical has been swallowed which has caused burning of the lips and throat, you can give the person frequent sips of cold water or milk, which may neutralise the poison a little bit. Then refer the person to the hospital or health centre urgently.
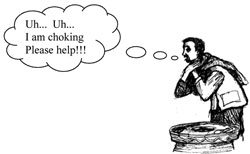
8.3 Choking
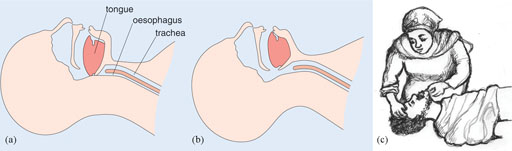
Choking is defined as an obstruction of the upper part of the windpipe (trachea) resulting in an acute life-threatening emergency (Figure 8.4). A person whose airway is obstructed will quickly become unconscious and die due to suffocation (lack of oxygen), unless the obstruction is quickly removed. Look back at Figure 4.1 in Study Session 4 of this Module to remind yourself of the location of the trachea in the respiratory system.
An obstruction of the airway may be partial or complete, and choking may occur in the conscious or unconscious person. The common causes of choking that you may be faced with are:
- Blockage of the airway by the tongue falling back into the throat of an unconscious person who is lying on their back (see Figure 8.4(a) later in this study session)
- Inhalation (breathing in) of a piece of food, such as a lump of meat, a chicken or fish bone, a bean or a nut; children may also inhale small objects during play
- Injury to the airway, for example after a blow to the front of the neck.
8.3.1 Signs of choking
You can distinguish between complete or partial obstruction of the airway by noting the following features:
In partial obstruction, the person may:
- have difficulty breathing, but may be able to call for help
- have a persistent cough (the body’s attempt at removing the obstruction)
- produce snoring and/or wheezing sounds.
In complete obstruction, the person may:
- be unable to speak, breathe or cry out
- be gripping his/her throat
- be agitated and distressed
- have a blue/dark tinge on the lips due to low oxygen levels
- rapidly lose consciousness.
8.3.2 How to help someone who is choking
In your village you may have seen someone choking before – perhaps a child or an adult. Were you able to help them? This is what you should do:
- If the person is breathing, encourage him/her to continue breathing and coughing.
- Slap the person vigorously on the upper back with your palms, while bending the person forwards. Do this several times (see Figure 8.5a).
- If back slapping does not remove the obstruction, try giving abdominal thrusts (see Figure 8.5b and Box 8.1).
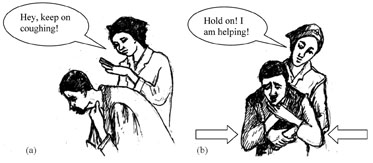
Box 8.1 Abdominal thrust technique to remove an airway obstruction
- Position yourself behind the person and put both of your arms around the upper part of the abdomen. Make sure that he/she is bending forwards.
- Make a fist with one hand over the person’s upper abdomen (between the bellybutton and the breastbone), then grasp the wrist of the fisted hand with the other hand (Figure 8.5b).
- Pull both your hands sharply inwards and upwards. Do this up to five times. This helps you to increase the pressure in the blocked airway in order to dislodge the obstruction.
- Usually, this will have removed the obstruction: however, if not, repeat the back slapping and abdominal thrust procedures two to three times more.
- If the person becomes unconscious, lay them on their back, open their mouth and try to remove any obstruction with your fingers or forceps if you have them. Begin ‘rescue breathing’ as described in Section 8.4.1.
A child is choking and comes to you coughing and screaming. Which technique would you use first and why?
You should first try backslaps and encourage coughing (Figure 8.6). This is the first step for someone who is choking but who can breath, speak and cough. In this case, the child’s coughing and screaming indicates that the blockage is partial because they can still breathe.
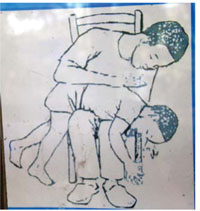 Figure 8.6 This poster is displayed in many Health Posts in Ethiopia to teach parents how to help a child who is choking. (Photo: Basiro Davey)
Figure 8.6 This poster is displayed in many Health Posts in Ethiopia to teach parents how to help a child who is choking. (Photo: Basiro Davey)
8.4 Basic life support techniques
In Study Session 7 you considered the effects of a single injury and how you might respond to each injury type. In this study session, you have learned how to deal with some common non-injury emergencies. In this final section, you will learn about basic life support techniques, which you must apply to a person who is unconscious or has stopped breathing for whatever reason – whether due to an injury, internal bleeding, septic shock, airway obstruction or some other cause. These techniques are also important in someone who is suffering from the combined effects of multiple injuries, e.g. after being hit by a car or falling off a horse, a person may have internal bleeding, a head injury and fractured bones.
Before giving care for each of the emergency conditions you suspect may be occurring, you must know how to prioritise your actions when giving basic life-supportive care. What should you do first, second and third? It is vital that you first address whatever condition is most threatening to their life. This section shows you how to do this.
8.4.1 The ABCDE-T approach
The simple way of remembering what to do first, second and third to save the life of a person with an emergency condition is to use a system known by the letters ABCDE-T (Box 8.2).
Box 8.2 The ABCDE-T of basic life support
You should perform these actions in the following sequence:
- A is airway care
- B is breathing
- C is circulation of the blood
- D is disability and brain and spinal cord damage
- E is exposure and examination of the person’s body
- T is transfer to the nearest health facility.
‘A’ stands for airway care
Your first action is to keep the airway open. As you already know, the commonest cause of blockage of the airway is food or another foreign body lodged in the windpipe. Airway obstruction can also occur when a person is unconsciousness after a blow to the head or neck, or because they have lost a lot of blood from an injury.
The obstruction after a head injury may also be due to a broken tooth, blood clots or the person’s tongue falling back into the throat and blocking the airway. This is particularly likely to happen if they are lying flat on their back.
Figure 8.7(a) illustrates how the airway gets blocked easily by the tongue falling back into the throat. In Figure 8.7(b) and (c), note how the action of lifting the chin also lifts the tongue and opens the airways, allowing the person to breathe. Remember that when you lift the chin, you must not move the neck! You may aggravate a possible neck or spinal injury in the process.
‘B’ stands for breathing
Once you are sure that the airway is open, the next step is to check whether the person is breathing or not. Listen for sounds of breathing and feel for breath on your cheek when you bend close to the person’s mouth. Also look for chest movements (rising and falling) as breath moves in and out. If the person is breathing steadily, you can put him or her in the recovery position (see Figure 8.8). Notice the position of the injured person’s legs and arms, which stabilise him on his side with his airway open. Lying the person on their side is to prevent choking if they vomit and to keep the tongue from falling back into the throat and blocking it.

If the person is not breathing at all, begin rescue breathing, i.e. breathing for the person, also known as ‘mouth-to-mouth resuscitation’. The steps of rescue breathing are shown in Box 8.3.
Box 8.3 Steps in rescue breathing for an adult patient
- Make sure that the airway is open
- Pinch the nose shut to prevent air from escaping and tilt the person’s chin upwards to open their mouth
- Fill your own lungs with air and steadily blow into the person’s mouth until the chest rises. This should take about two seconds
- Feel for the person’s pulse to make sure their heart is beating, but don’t waste time measuring the pulse rate
- Repeat the rescue breaths about every five seconds. Do this for about one minute, giving about 12 rescue breaths in that time
- Feel for a pulse between every rescue breath. Continue rescue breathing as long as a pulse is present but the person is not spontaneously breathing on their own
If the patient is a child:
- Follow the steps above, but you need to give smaller, faster rescue breaths. Give one rescue breath about every three seconds. Do this for about one minute, giving about 20 rescue breaths in that time. Then continue with step 6.
‘C’ stands for circulation
Once you are sure that the person is breathing, then check for any site that is bleeding. Count the person’s pulse and measure the blood pressure. If there is any bleeding give first aid to stop the bleeding (look back at Box 7.1 in the previous study session). If the person has got any signs of shock, start pre-referral intravenous (IV) fluid therapy, if you have been trained to do so.
If a person has a haemorrhage or septic shock, what do you expect to find when you take the pulse and blood pressure?
The pulse will be rapid (possibly over 100 beats per minute), but weak and fluttering. The blood pressure will be low and falling; the diastolic pressure may be below 60 mmHg.
‘D’ stands for disability and brain and spinal cord damage
Next you assess the person for any possible head or spinal injuries, as described in the previous study session (Section 7.4).
Do you remember the signs of head or spinal injuries?
The person may have difficulty breathing, pain in the neck, head or back, blood or fluid coming from the nose, ears or cuts on the scalp, tingling or loss of sensation in the hands, fingers, feet or toes, confusion, loss of control of urination and defaecation, difficulty with balance and walking, or partial or complete paralysis.
‘E’ stands for exposure
Expose the person to your full attention; this means open their clothes and if possible remove their clothing. You must do this very carefully, avoiding moving the limbs, head or neck if you suspect a limb fracture, head or spinal injury. Look at the whole person to be certain that you have not missed any injury. Examine the abdomen for swelling, tenderness or ‘guarding’ the internal organs with rigid muscles, which may indicate internal injury, acute appendicitis or intestinal obstruction.
‘T’ stands for transfer
When you have stabilised the patient by treating any immediately life-threatening conditions, transfer your patient to the nearest health facility as quickly as possible. Remember to take all the precautions to reduce trauma and support life during the journey, as described in this and the previous study session.
What else should you remember to do?
Write a clear referral note giving the patient’s name, address, age, the circumstances that led up to the emergency, your assessment of their condition, and any actions you have taken. Sign and date the referral note and print your name and contact details so the higher level health facility can communicate with you about the patient.
This concludes Part 1 of this Module. In Part 2, we turn to the important subject of mental health problems in rural communities.
Summary of Study Session 8
In Study Session 8, you have learned that:
- Non-injury emergencies, such as appendicitis, intestinal obstruction, poisoning or choking, are potentially life-threatening conditions that require urgent attention and life-supportive care.
- The effects of non-injury emergencies are more severe in young children and old people. This is due to delayed recognition of their condition because their symptoms may not be typical, and the body's more limited ability to reduce the effects of these conditions in extreme age groups.
- Appendicitis means inflammation and infection of the appendix. The signs and symptoms are similar to intestinal obstruction: i.e. abdominal pain, tenderness and guarding of the internal organs by rigid abdominal muscles, fever, nausea, and vomiting. In advanced cases, septic shock may occur.
- Poison can enter the body through the mouth, lungs or skin, or it may be injected; poisoning may be accidental or intentionally self-inflicted (suicide) and the poison (toxin) may be naturally occurring, a manufactured chemical or an overdose of medicine.
- Common symptoms of poisoning include nausea, vomiting, abdominal pain, difficulty in breathing, headaches, fast, slow or irregular heart rate, watering of the eyes, confusion, and impaired consciousness. If poison was absorbed through the skin, there may be swelling, rashes, redness and itching.
- First aid for a person who is choking is to encourage coughing, back slapping and applying repeated abdominal thrusts. If the person becomes unconscious, attempt to remove the obstruction if you can see it in their throat and begin rescue breathing.
- Basic life support techniques can be used for both injury and non-injury emergency life-threatening conditions.
- A simple way to remember the priorities of basic life-supportive care is to use the ABCDE-T approach, addressing in this order: their Airways, Breathing, Circulation, Disability, Exposure (to check for anything you may have missed), and Transfer to a higher health facility.
Self-Assessment Questions (SAQs) for Study Session 8
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 8.1 (tests Learning Outcomes 8.1, 8.3 and 8.5)
- a.In which group of patients is it most difficult to recognise the signs and symptoms of appendicitis and intestinal obstruction?
- b.Which signs and symptoms are common to both conditions?
- c.Are there any signs that may make you more likely to suspect appendicitis or more likely to suspect intestinal obstruction?
Answer
- a.Gastrointestinal emergencies are more difficult to recognise in very old and very young people.
- b.The signs and symptoms that are common to both appendicitis and intestinal obstruction are abdominal pain, guarding the internal organs with rigid abdominal muscles, nausea and vomiting, and fever.
- c.A person suffering with acute appendicitis is more likely to experience lower abdominal pain, particularly on their right side. An intestinal obstruction usually produces widespread abdominal pain, the abdomen may be swollen and the person may have difficulty in passing faeces or gas.
SAQ 8.2 (tests Learning Outcomes 8.1, 8.2 and 8.5)
What life-supportive care do you give to a person with a gastrointestinal emergency?
Answer
Life-supportive care for patients with gastrointestinal emergencies depends on the severity of the symptoms. If the symptoms began very recently, give two paracetamol tablets with a small cup of water to relieve the pain. If the symptoms are advanced and there are signs of shock, begin IV fluid administration. In both cases, refer the patient to the nearest hospital or health centre, instructing them to take nothing by mouth before they have been seen by a doctor, because surgical intervention is likely to be required.
SAQ 8.3 (tests Learning Outcomes 8.1, 8.3, 8.4 and 8.5)
Which of the following statements is false? In each case, explain what is incorrect.
A If you suspect that a person has swallowed poison, apply abdominal thrusts to help them to cough out the poison.
B If you suspect that a person has absorbed poison through their skin, remove any contaminated clothing and wash the body with soap and water before referring them.
C Swallowing bleach or kerosene is a common method of trying to commit suicide in rural communities in Ethiopia.
D Tying a cloth over the nose and mouth is good protection from inhaling droplets of insecticide while spraying houses to kill mosquitoes.
E Burning charcoal in an enclosed room is dangerous because the fumes are poisonous and inhaling them can cause loss of consciousness.
Answer
A is false. Abdominal thrusts are applied to help someone who is choking to cough the obstruction out of their airway. This technique is useless to help someone who has swallowed poison, which will be absorbed into their body through the digestive tract.
B is true. If you suspect that a person has absorbed poison through their skin, remove any contaminated clothing and wash the body with soap and water before referring them.
C is true. Swallowing bleach or kerosene is a common method of trying to commit suicide in rural communities in Ethiopia.
D is false. Tying a cloth over the nose and mouth is not adequate protection for someone who is spraying houses to kill mosquitoes. Insecticide sprayers should wear proper protective clothing, including a special mask.
E is true. Burning charcoal in an enclosed room is dangerous because the fumes are poisonous and inhaling them can cause loss of consciousness.
SAQ 8.4 (tests Learning Outcomes 8.1, 8.3 and 8.5)
Mrs Chaltu is found unconscious after complaining to her neighbours that she is feeling miserable.
- a.What do you suspect has happened? What would you look for in her surroundings and why?
- b.Outline how you would perform basic life-supportive care for her.
Answer
- a.You suspect that Mrs Chaltu has tried to kill herself by drinking a poisonous chemical. Look for any empty containers in her surroundings to see if you can identify what she has swallowed. Take the containers with you to show the doctor when you transport Mrs Chaltu to the nearest health facility.
- b.She is unconscious so you should apply the basic life support techniques outlined in the ABCDE-T approach, first making sure that her airway is open by placing her in the recovery position (Figure 8.2), and checking her breathing, pulse and blood pressure. If she is not breathing, begin rescue breathing for her. Once she is breathing, if there are signs of burning on her lips, mouth and throat (e.g. from swallowing bleach or kerosene), give her sips of cold water or milk. Check for any signs of disability and examine her body in case there is anything you have missed. Go with her on the transfer to the health centre or hospital.
Read Case Study 8.1 and then answer the question that follows it.
Case Study 8.1 An emergency at a wedding feast
Mr. Shewangizaw is celebrating his daughter’s wedding. He was in good health and happily moving around the wedding tent, talking and encouraging guests to enjoy the food and drink prepared for the wedding feast. However, shortly after sitting down to eat himself, he began coughing and appeared to be having difficulty breathing, holding his neck with both hands and coughing forcefully and persistently.
SAQ 8.5 (tests Learning Outcomes 8.1, 8.4 and 8.5)
What is the correct sequence of actions that you should perform to help this man?
Answer
Mr Shewangizaw is choking, probably caused by a blockage of food in his airway. He should be encouraged to cough to remove the obstruction. If this does not work, you should support the effort by slapping his upper back. If the back slapping does not work, use the abdominal thrust technique. If he becomes unconscious, lay him down and see if you can remove the obstruction from his throat with your fingers or forceps. Begin rescue breathing to keep him alive while he is taken to a hospital or health centre.