Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Thursday, 12 February 2026, 6:37 PM
Non-Communicable Diseases, Emergency Care and Mental Health Module: 11. General Management Principles in Mental Health Care
Study Session 11 General Management Principles in Mental Health Care
Introduction
As described in Study Session 9, mental illnesses are common in the community. However, most communities in Ethiopia receive little benefit from either general health services or the scarcely available mental health services. This may be because of lack of knowledge, skill and attitude, both among healthworkers and in society at large. Therefore, your training will help you in identifying and giving care to people with mental health problems. In this study session you will learn about ways to talk to clients, how to identify their problems and needs, recognise and handle emergency psychiatric conditions and help clients to cooperate in accepting medicines and other treatment methods. We will also discuss how to follow up on cases.
Learning Outcomes for Study Session 11
When you have studied this session, you should be able to:
11.1 Define and use correctly all of the key words printed in bold. (SAQs 11.1 and 11.2)
11.2 Outline the key principles of how to approach people with mental illness. (SAQ 11.1)
11.3 Describe how people with a mental illness can be identified. (SAQs 11.2 and 11.3)
11.4 Describe the emergency management of urgent mental health problems. (SAQs 11.2 and 11.3)
11.5 Describe the referral process for people with mental health problems and how these clients should be followed up in the longer term. (SAQs 11.3 and 11.4)
11.1 General approaches to people with mental health problems
To be able to help people with a mental illness it is important to think carefully about how you approach people with mental health problems. In your practice, when you see a person with a mental illness, you may show emotional reactions, which directly or indirectly determine your approach to the client. A common response is to try to keep away or avoid them. Many people may think: ‘Why should I bother, he is mad’. However, with this approach it is difficult for clients to develop trust in you and they may therefore be unlikely to accept your help. Many clients recognise and understand your reactions and respond accordingly. If you trust them and treat them with love and affection, they will also do the same towards you. If you are helpful, they will cooperate. People with mental health problems like to be treated as responsible and respectable individuals. You should treat them as individuals who are in real need of your understanding and help. A good starting point is to ask them about their problems and listen to them patiently (see Figure 11.1).
After the client has given their version of their problems, obtain information from their family members regarding how they see the problems. If you find differences between the two accounts, do not get alarmed or angry. Draw their attention to the discrepancies and kindly request them to clarify the issues for you, so you understand their points of view. When you are interviewing the client or the family members, ask the essential questions without going into unnecessary details. It is important to develop your skills in recognising, identifying and giving care to people with mental illness. Below we outline a few key principles in how to approach people with mental health problems and their relatives.
11.1.1 Listening with interest

For a good understanding of your clients’ problems it is necessary to listen to them with interest and patience. People like to relate their own personal feelings and ideas. It is important to provide adequate privacy and give the clients ample time to tell their story. Active listening involves careful attention not just to what is being said but also to how it is said and to the feelings expressed by your client. Based on what you hear and observe you can then adjust your response to the client. To show your client that you are an active listener it can also be helpful to refer to earlier conversations and discussions. Active listening requires respect for the client’s view even if you do not agree with them.
11.1.2 Acceptance people’s beliefs
Every community has a rich experience and varying views and beliefs on all aspects of life, including mental health problems. These views and beliefs are often embedded in the community’s history and shaped by observations and events that happened in the past.
In your past life or work experience you may have come across people with serious medical conditions, such as epilepsy. Recall one such situation and describe what people in the local community thought was the cause of this illness. You may also want to refer back to Section 9.2.2 in Study Session 9, on explanatory models and cultural context, before answering this question.
We don’t know what exact situation and medical condition you recalled, and the people in your local community may have responded in different ways. One common belief in rural Ethiopia is that epilepsy is caused by being possessed by the devil. The person with epilepsy or their family may therefore think that medical treatment is unnecessary.
A simple technique to understand what people think about mental health is to ask them a specific question and allow them to narrate their views in their own words without too many interruptions. It is important to accept that people may have different ideas about mental health. This respect for the existing values and beliefs allows you to subsequently plan and execute your care. For example, in the situation described above, about the person with epilepsy who thinks they are possessed by the devil, you would make sure to give your client some essential education about epilepsy and encourage them to take appropriate drug treatment. The topic of epilepsy is discussed in more detail in Study Session 15.
11.1.3 Interest in individuals
Any activity carried out with interest is likely to give better results. You will regularly visit families in your catchment area as part of various healthcare activities. When you do, it would be helpful to know their names, their family situation, and their individual circumstances, and to speak to them about their backgrounds. This helps in building a relationship with your clients and will make them feel more comfortable, so that they are more likely to share their problems with you. Knowing about the history of your client also helps in devising an appropriate treatment plan.
11.1.4 Encouraging emotional expression
Your job may expose you to individuals who have experienced traumatic events, such as illnesses, accidents or the death of someone they love. As a consequence your client can appear to be emotionally very upset. You should encourage the expression of emotions by asking your client about their feelings, their fears and the effect the event has had on their life. Such emotional expression is part of the treatment and may relieve their stress. Sometimes your client’s emotion may be expressed in the form of irritation, anger or crying. When this happens it is important to remain patient and try not to criticise or judge your client.
11.1.5 Recognition of the needs of people with mental health problems
As a consequence of their mental illness, people with mental health problems often have difficulty with functioning in normal daily life. They are likely to want more attention, love and affection. They may also complain a lot and express dissatisfaction with their family and other significant individuals. This does not mean that the individual is finding fault with others and should not be responded to in any judgemental manner. In such situations you can react by saying it is understandable to feel this way when having such an illness.
11.1.6 Reassurance
Mental health problems can be very unexpected and stressful. These problems may make your client and their relatives feel very uncertain about the situation; it is natural for everyone to expect support during this period. Reassurance from someone like you who knows what is happening and whom they can trust can be valuable to help them to get over a crisis situation. You should always provide reassurance where you can, for instance by informing your client and their family about the lack of harmful effects of medicines. However, it is best to avoid unrealistic reassurance in situations beyond your capacity.
11.1.7 Non-judgemental attitude
You may be approached by many people from your local community, because most people feel comfortable with healthworkers. In your role it is important to avoid quick judgements and telling people that they are right or wrong. At no point should you refer to the public as unintelligent, illiterate, dumb, or useless. Instead, your efforts as a healthworker are essential in bringing about changes in people’s attitudes and knowledge about mental health. You are there to assist everyone to achieve a higher level of health by providing care and health education.
11.1.8 Maintain confidentiality
As a healthworker, you are likely to get private and sensitive information from a client during the assessment and management process. It is very important to maintain confidentiality, that is, to keep the information private and not to share it with anyone outside the medical team involved in taking care of the person. Your duty is to assure clients that their information will be kept confidential and to ensure that it remains so. This will help in building trust between you and your client.
11.2 Management of people with mental illness
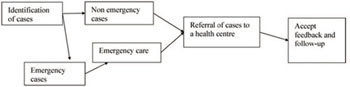
Many people with mental health problems do not get any meaningful treatment. Along with your regular healthcare responsibilities, there are several steps you can undertake to help (see also Figure 11.2):
- Identify all the persons with mental illness and epilepsy in the population covered by you.
- Provide necessary care including emergency care.
- Refer the identified persons to the next level health centre or hospital.
- Conduct regular follow-ups with the patient and their family members to check how they are doing, and to enquire about possible adverse effects of medication and adherence to treatment.
Each of these aspects of mental health management will be discussed in more detail in the remainder of this study session.
11.2.1 Identification of people with mental illness in the community
In order to identify people with mental health problems, you should perform routine enquiries during your practice in the community. You can identify people with mental health problems during your daily work. For instance, when you go to a village for your routine work, talk to important people like the village shimagle, neighbours, kebele or village leaders, teachers, youth leaders, women’s association leaders and shopkeepers. Ask them to tell you about individuals they hear saying they are possessed or bewitched, or who appear to be suffering from a mental health problem. Inform them that these conditions can be helped and that such help is available at the nearest higher-level health facility. Request them to refer such people to you or to the nearest health centre or hospital. Every time you meet them, remind them to do this.
Likewise, when you visit people’s homes, ask tactful questions (without offending any family members) to obtain information about anyone in that family or neighbourhood who may be suffering from mental health problems. When you go to a school to carry out school health activities, ask teachers and students about any children who have fits, or have behavioural or learning problems. Lastly, it is important to be sensitive to possible mental health problems in those who contact you for other health-related problems.
Using this approach, you can identify people who may need help during your routine duties. Make sure that you identify who they are and get their details, so that you can refer them to a doctor who specialises in diagnosing and treating mental health problems (see Section 11.2.3).
Suppose that on one of your village visits the village leader informs you that Mr Abdissa appeared to be drunk frequently in the last few weeks. You decide to pay Mr Abdissa a visit to see how he is doing. Based on what you have so far learned in Study Sessions 10 and 11, what kinds of questions would you ask Mr Abdissa?
As you may recall from what you have learned so far, it is important to show an interest in the people in your village and to be an active listener. Before asking Mr Abdissa sensitive questions about his problems, you would start making friendly conversation, for instance about village events, or how Mr Abdissa’s crops are growing. After having created a friendly atmosphere you would try to get to know more about Mr Abdissa’s possible alcohol problems by asking questions such as: ‘Have you been worried about drinking too much alcohol recently?’ and ‘How much money and time have you been spending on alcohol recently?’
In your work you may encounter individuals who need emergency care. In the next section we will discuss how you can manage these situations.
11.2.2 Care of people with emergency mental health conditions
You may be in situations where people will be in need of urgent help but the doctor is too far away or not available. Under these circumstances, you must offer immediate help. In this section we will describe four different situations in which urgent help is needed, and what you should do in these circumstances.
Agitated and violent person
People with agitated and violent behaviour are individuals who are restless, unable to sit still, angry looking and who threaten to attack. Because of the threat of violence this is an emergency situation and you will need to use special techniques to approach them. Box 11.1 explains how you could manage a situation like this.
Box 11.1 How to deal with a violent or agitated person
- Get help from someone in whom the person has confidence.
- Advise others not to talk or behave in a way that might irritate or provoke the person.
- Tell individuals whom the person does not like to keep away.
- Keep some distance from the person while you try to find out what the reasons are for their anger and what is troubling them.
- Try to gain the person’s confidence by asking them: ‘What are your problems? Why are you so angry? What is troubling you? I am here to help you.’
- Do not argue with the person or provoke them.
- When the person calms down, see that he or she takes some fluids and food.
- Try to convince them that they need medication and that it is better if they see the doctor.
- If the person is not in a position to listen to you, organise people to throw a blanket, gabi or netela on the person and hold them with the help of others. Take them to the hospital immediately.
- Do not use thread, rope or chain to restrain the person. If necessary, use only a towel or long cloth to tie their hands.
Withdrawn person
A withdrawn person is someone who avoids any form of social contact. This may be caused by the presence of suicidal thoughts or plans. Whenever someone threatens to kill themselves, take their words seriously (see Section 10.5 in the previous Study Session). Make sure that there is always someone else present with the person until they are taken to a doctor. Box 11.2 helps you to know what to do when you see a withdrawn person.
Box 11.2 What to do when you see a withdrawn person
- Take time to talk to the person as they may have a delayed response.
- Persuade them to eat something.
- Ask family members for possible reasons for withdrawal.
- Find out whether they feel like ending their life, and if so, try to find out what the reasons are for the suicidal thoughts.
- Listen with sympathy, encourage the person to talk about their problems in detail, and reassure them that you will assist them to solve the problems.
- Take the person to the doctor yourself or refer them immediately, along with a supportive relative or friend.
Paranoid person
You may come across people who have disturbed thoughts. They may be suspicious of other people’s motives, and may think all other people are against them. They may have delusions (as part of psychosis) or the suspiciousness may be due to alcohol abuse or depression. It may not be easy to approach a person in a paranoid state, because they might think you are one of the people who are against them. You must be careful how you go about it; the methods outlined in Box 11.3 may serve as your guidelines.
Box 11.3 What to do when you meet a paranoid person
- Be fair and honest. Do not tell lies or hide information.
- Do not question the person’s beliefs or suspicions. Do not tell them that their beliefs are wrong, baseless or false.
- Allow the person to talk about their suspicions. Collect more information. Do not pass judgement on them.
- Draw their attention towards their possible other problems, like sleeplessness, decreased appetite, etc. Try to convince the person to see the doctor and to take necessary medication.
Confused person
Persons with extreme confusion may not recognise the time of the day, where they are or where they live, or may not recognise people they have known before. Confusion may be caused by head injury, infectious disease, alcohol withdrawal, or diabetes mellitus, but could also be due to other causes. It is important that you recognise people who are in a confused state, as they need a quick evaluation and urgent referral to a health centre or hospital (see Box 11.4).
Box 11.4 What to do when you see person in a confused state
- Find out whether the person had jerky movements of the limbs. The confused state could be the consequence of an epileptic fit.
- Find out whether the person is a known case of diabetes or high blood pressure.
- Enquire whether the person has had a recent head injury or has consumed alcohol.
- Tactfully find out whether the person has consumed drugs (perhaps with the intention to commit suicide).
- Examine the person to see if they have high fever.
- All people with significant levels of confusion should be referred to a health centre as soon as possible.
- Because of the risk for an epileptic fit, avoid giving drink or food.
- Avoid the presence of strangers and unwanted disturbances around the person as it may aggravate the confusion.
11.2.3 Referral
Following identification of the mental health problem and giving first aid if the person is injured or has hurt someone else (recall Study Session 7), you will need to refer the person to a health centre. In the case of an emergency situation the person should be referred to a health centre as quickly as possible. Find out who the leader of the family is and give this person the responsibility to get the patient to the health centre. You should accompany the patient whenever possible. Urgent cases need to be referred based on the referral criteria outlined in Box 11.5.
Box 11.5 General criteria for an emergency mental health referral
- Severe illness, violent and unmanageable at home
- History of recent head injury
- Person has fever, severe headache, vomiting or fits
- Person has attempted suicide and is still threatening to commit suicide
- Person has frequent epileptic fits (more than 3 times a day or continuously).
- A mother shows disturbed behaviour following childbirth (see Study Session 13 in this Module and Study Session 3 in the Module on Postnatal Care).

When the situation is not urgent you can refer the person using the regular referral route. In this case you should send a referral note to the doctor giving all the relevant details you have noted. During your next visit to that family, find out whether they consulted the doctor. If they have not done so, find out the reasons why and encourage them to still do so.
11.2.4 Follow-up
Following your referral, the doctor at the higher health facility will examine the person with mental health problems, diagnose the nature of the illness and prescribe the appropriate treatment if necessary. After the treatment is initiated (Figure 11.3) it is essential to have follow-up visits to your clients and their family members to discuss how they are doing. Follow-up is important to achieve adherence to treatment and improve the overall outcome. If for any reason the patient discontinues the prescribed treatment, all your efforts and the efforts of the doctor and the family members will have been fruitless. Box 11.6 outlines some of the questions you should go through during the follow-up visits to a client who has been on prescribed medication.
Box 11.6 Questions to ask during follow-up
- Is the client taking their medicines regularly as prescribed?
- How much improvement has the client made?
- Has the client developed any side effects following the drug use?
- Has the client started working again?
- Has the client seen the doctor for follow-up and review?
Based on the information you collect during the follow-up visits, you may identify some continuing issues that need to be addressed. In the remainder of this section we will discuss how you can deal with some of the problems that are likely to arise during follow-up of clients who are taking medication.
Adverse effects of medication
Some of the people who take medication to treat their mental illnesses may experience unwanted effects (also known as adverse effects). Different types of medical drugs are used to treat different mental health problems, and some drugs may produce side effects that are unpleasant to the client. Some of these effects are mild, in which case you can reassure the patient; for example, when a client complains about dryness of the mouth, light-headedness or constipation, reassure them that it is temporary. Dryness of the mouth can be helped by taking more water. However, severe unwanted effects, such as unclear speech, walking unsteadily like a drunken person, stiffness of the limbs, or twitching of the tongue, mouth, neck, hands or legs can also occur in some people. A patient may also experience drooling of saliva or drowsiness. If any of these side effects occur you should refer the patient to the doctor immediately. Any necessary changes in the drug dosage will be carried out by the doctor.
When a person is very agitated they are often put on a high dose of medication. As they get better over time a lower dose is needed to adjust to the new situation. Because of the risk of relapse (return of the previous symptoms of mental illness), the drugs should not be stopped suddenly. Similarly, people who are very sad and depressed and receive drugs to treat their problems should not suddenly stop their treatment when they start to feel better. Instead the drugs should be reduced gradually and then stopped, always in consultation with the doctor, to avoid relapse.
Making sure your client takes their medication
For a very ill or unmanageable person, one member of the household should be made responsible to make sure that the patient takes their medication. A neighbour or any other individual in the village who is close to the patient could also be given this responsibility. If the family is taking less interest in treating the person with mental illness, or if the family mainly has faith in traditional cultural methods of treatments talk to them repeatedly to convince them to (also) accept modern treatments for the patient. Geographical distance, financial difficulties and absence of a family member to accompany the patient to the health centre can also be reasons for not starting or continuing medication. You can solve these problems by mobilising other help, such as another person from the same village. In some cases, you could collect the drugs from the doctor yourself and deliver them to your client directly.
A person with mental health problems who shows improvement over time is the best example for others. Use these examples to demonstrate the value of modern treatment to other people with mental health problems and to the people in your community in general.
Summary of Study Session 11
In Study Session 11, you have learned that:
- In the process of helping people with mental illness, it is important to recognise your own reaction towards your client and try to control it. Your clients are sensitive to your approach and respond accordingly.
- Calling the client by their name, listening to them with interest, understanding and respecting their views about illness are some important principles of a good approach to people with mental health problems.
- There are several methods, such as talking to relevant individuals in your community, to identify people with mental health problems.
- There are situations that require emergency care. You should respond to these situations in different ways depending on the type of problems observed. Emergency situations require an urgent referral; non-emergency cases can be referred using the regular referral system.
- After a person with mental health problems is identified and referred to the health centre, they should be followed up to ensure their future wellbeing.
Self-Assessment Questions (SAQs) for Study Session 11
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 11.1 (tests Learning Outcomes 11.1 and 11.2)
Which of the following statements are false? In each case explain why it is incorrect.
A Clients who receive medication for their aggressive behaviour should be informed about the possible unwanted side effects of the treatment.
B People with traditional beliefs like the idea that mental illness is caused by a curse should be directly challenged and told they are wrong and silly.
C If a patient behaves aggressively you should apply physical punishment.
D Encouraging emotional expression and keeping a client’s sensitive information confidential are two principles of a good approach.
Answer
A is true. If the client and their family know about the side effects of drugs it will reduce their anxiety and it may make them more tolerant to mild adverse effects. They also need to know about possible serious unwanted effects, so that they can recognise these easily and ask for help from you or the treating doctor immediately.
B is false. Traditional beliefs have been around for many generations and are often embedded in the community’s culture. A key principle of a good approach to your community members is to be non-judgemental and show them respect regardless of their beliefs. People should thus not be told they are silly and wrong, but instead should be educated about mental health problems and their treatment in a respectful way.
C is false. Patients should not be punished for their behaviour when they are mentally ill. They may behave aggressively because they are not aware of what they are doing or they are not able to control their actions. Rather than being punished, they should receive appropriate treatment.
D is true. You have learned that expression of emotion is one way of relieving the client from their tension. Keeping a client’s sensitive information confidential is ethical and helps to build a good relationship between you and your client.
SAQ 11.2 (tests Learning Outcomes 11.1, 11.3 and 11.4)
Neighbours of Mr Teklu reported to you that they have heard him talking loudly when there was no one there. He thinks everyone in the neighbourhood is against him. Identify what type of problem Mr Teklu has and what you can do in this situation.
Answer
Mr Teklu thinks everyone in his neighbourhood is against him, which is indicative of paranoid delusion. It also seems that he hears things that aren’t there, which is described as hallucination (as discussed in Study Session 10). Both delusions and hallucinations are characteristics of psychosis. Because Mr Teklu is paranoid, make sure to not hide information from him; don’t tell him that his beliefs are wrong and don’t pass any judgement. Try to collect more information about Mr Telku, for instance about other problems he may have. Psychosis is a serious illness, so you should refer Mr Telku to a healthcentre or hospital.
SAQ 11.3 (tests Learning Outcomes 11.3, 11.4 and 11.5)
- a.While doing your routine health care activity, you meet Mrs Mulu, a 27-year-old married mother of one, who acts in a confused way. You are informed that she has fallen on her head following a fit. Explain what Mrs Mulu’s problems are and how you should proceed.
- b.A few months later you meet Mrs Mulu again. After a period of treatment, Mrs Mulu failed to take her medication and developed frequent fits that took a long time before she regained consciousness. How should you handle this new situation and prevent it from happening again in the future?
Answer
- a.Mrs Mulu manifested with confusion following an epileptic attack. The confusion may be because of epilepsy or may be the consequence of her head injury, therefore she should be referred to a health centre or a hospital urgently.
- b.Mrs Mulu has poor adherence to treatment which resulted in a serious medical emergency. She requires first aid and immediate referral accompanied by a health worker or responsible family member. After giving emergency care and referring Mrs Mulu to the health centre or hospital, you need to find out why she has not been taking her medication. This may be because of her poor knowledge of the disease course and need of treatment; in that case you need to educate Mrs Mulu and her family about her condition. If Mrs Mulu has difficulty accessing the treatment you could decide to collect the drugs from the doctor yourself, or ask a member of Mrs Mulu’s family to do this for her.
SAQ 11.4 (tests Learning Outcome 11.5)
Suppose a man with psychosis has received treatment at Amanuel Hospital with a drug called chlorpromazine. After treatment he improved and was sent to you for follow-up. List which aspects are important to discuss during follow-up.
Answer
During follow-up it is important to find out how your client is doing, whether his condition has improved and how he feels more generally, for instance whether he has been able to start working again. You should also ask whether he is taking the medication as prescribed by the doctor, whether he has developed any unwanted effects, and whether any follow-up visits to the treating doctor are planned.