Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Thursday, 22 January 2026, 7:26 AM
Nutrition: 4. Infant and Young Child Feeding
Study Session 4 Infant and Young Child Feeding
Introduction
In Study Session 3 you were introduced to nutrition throughout the life cycle. In this study session you will learn about optimal infant and young child feeding during the first two years of life. As the first two years are critical to break the cycle of malnutrition from generation to generation, key feeding issues, including optimal breastfeeding and optimal complementary feeding, will be looked at in some detail. You will learn more about the key messages you can give the mother regarding optimal feeding practices during the different contacts that you have with her.
Learning Outcomes for Study Session 4
When you have studied this session, you should be able to:
4.1 Define and use correctly all of the key words printed in bold. (SAQ 4.1)
4.2 Describe infant and young child feeding problems in Ethiopia. (SAQ 4.1)
4.3 List the key messages to be given to mothers on optimal breastfeeding. (SAQs 4.2 and 4.3)
4.4 Outline the feeding recommendations for mothers who are HIV-positive. (SAQ 4.4)
4.5 List the benefits of breastfeeding for mothers, children and the community. (SAQ 4.2)
4.6 Describe breastfeeding problems and identify their solutions. (SAQ 4.5)
4.7 List the key messages to be given to mothers on optimal complementary feeding. (SAQ 4.6)
4.1 Infant and young child feeding problems in Ethiopia
The first two years of a child’s life are the most important for establishing healthy growth.
Optimal feeding of children during the first two years is critical to break the cycle of malnutrition from generation to generation. The first 24 months is recognised as being the most important window of opportunity for establishing healthy growth. Infant and child feeding practices are major determinants of the risk of malnutrition. A very large proportion of women do not practice optimal breastfeeding and complementary feeding behaviour for their children. About a third of babies do not receive breastfeeding within one hour of birth and only one in three children age four to five months are exclusively breastfed. According to profiles analyses using Demographic Health Survey data, it is estimated in Ethiopia that there are about 50,000 infant deaths a year attributable to poor breastfeeding habits, that is, 18% of all infant deaths every year. You have a critical role to play in helping to address this problem (see Figure 4.1).

Equally important are the serious problems related to when complementary food is introduced, because a large majority of infants are given such foods too early or too late. At six to eight months of age, only one in two children is consuming solid or semisolid food. Much of the inappropriate breastfeeding and complementary feeding behaviour is actually due to lack of knowledge, rather than practical or financial constraints, and you will have plenty of opportunities in your work to give mothers the best information possible.
4.2 Global and national recommendations for child feeding during the first 24 months
Nearly one in five infant deaths each year are attributable to poor breastfeeding habits.
Based on the global infant and young child feeding recommendations developed by the World Health Organisation in 2002, the Ethiopian National Infant and Young Child Feeding (IYCF) Guideline was developed in 2004. The guideline stresses the following IYCF strategies during the first two years:
- Exclusive breastfeeding during the first six months (exclusive breastfeeding is defined as giving only breastmilk and no other food or fluid including water except medication)
- Start optimal complementary feeding at six months with continuation of breastfeeding for the first two years or beyond (complementary feeding means giving solid or semisolid food to a child in addition to breastmilk).
4.2.1 Key messages for optimal breastfeeding practices
An important part of your job is connected to helping mothers and caregivers to feed their children in the most effective way possible. It is therefore very important that you help them to understand the importance of optimal breastfeeding. The following are key messages that need to be explained to the mother. You should make sure that she understands why these behaviours are important and that you have given her the underlying reasons for each of the key messages. You will be using these messages when you are educating or counselling mothers.
The mother initiates breastfeeding within one hour of birth
Initiating breastfeeding within one hour protects the infant from disease by providing the thick, yellowish first milk (colostrum) which is the equivalent to the infant’s first vaccine. It also helps to expel the placenta more rapidly and reduces blood loss by the mother. It also helps expel meconium (the infant’s first stool), stimulates further breastmilk production and keeps the newborn warm through skin-to-skin contact.
The mother breastfeeds frequently, day and night
The mother should allow the infant to breastfeed on demand (as often as the infant wants) (see Figure 4.2). This means feeding every two to three hours (8–12 times per 24 hours) or more frequently if needed, especially in the early months. The mother needs to breastfeed frequently to stimulate milk production. Breastmilk is perfectly adapted to the infant’s small stomach size because it is quickly and easily digested.

The mother gives infant only breastmilk for the first six months.
The mother needs to breastfeed frequently to stimulate milk production.
Breastmilk contains all the water and nutrients that an infant needs to satisfy its hunger and thirst. Exclusive breastfeeding helps to space births by delaying the return of fertility. Exclusively breasted infants are likely to have fewer diarrhoea, respiratory, and ear infections. You should encourage and support the mother to exclusively breastfeed her baby, explaining how it will help both her and her infant (see Figure 4.3).

The mother continues breastfeeding when either she or the infant is sick
Sick infants need breastfeeding more frequently.
If the mother is sick with a cold, flu or diarrhoea, she can continue to breastfeed because breastmilk still protects the infant against illness. If the infant is sick, mother has to breastfeed more frequently (or express her milk if the infant cannot breastfeed) so that the infant recuperates faster. Breastmilk replaces water and nutrients lost through frequent loose stools, and is the most easily digestible food for the sick infant.
The mother positions and attaches infant correctly at the breast
The mother has to position and attach the infant to the breast correctly to help prevent sore or cracked nipples, and to stimulate her milk supply. Signs that infant is properly positioned are:
- The infant’s whole body is facing the mother and is close to her
- The mother holds infant’s entire body, not just the neck and shoulders.
Signs that infant is properly attached include:
- The mother brings infant toward her breast, not the breast toward her infant
- The infant’s mouth is open wide
- The infant’s lips are turned outwards (like a fish mouth)
- The infant’s chin touches the mother’s breast
- The mother’s entire nipple and a good portion of the areola (dark skin around the nipple) are in the infant’s mouth
- More areola is showing above rather than below the nipple.
The IMNCI Module provides more details about effective breastfeeding and how you can support mothers to achieve this.
The mother offers the second breast after the infant releases the first
The mother has to allow the infant to release the first breast before offering the second breast so that infant receives both ‘fore milk’ which has a high water content to quench the infant’s thirst, and ‘hind milk’ which is rich in fat and nutrients. The mother should not give bottles and pacifiers (dummies) to her breastfed infant because they can interfere with breastfeeding and cause diarrhoea and other possibly serious infections as they are difficult to keep clean.
The mother should eat more than usual
As breastfeeding increases the nutritional requirements of the mother, she needs to have two additional meals (about 500 kcal) every day. Her diet should also be varied (for example by adding vegetables and fruits).
By the age of six months the mother or caregiver must add complementary food
The complementary food given to the child should be varied as much as possible, increasing the quantity, frequency and density of the food as the child gets older. This is in addition to the need for the mother to continue breastfeeding until the child is two years of age or older.
Why should the mother switch the baby to the second breast only after completely suckling the first one?
It is important because the fore milk has a high water content to quench the infant’s thirst and the baby also needs to get the hind milk which is rich in fat and nutrients.
4.3 Benefits of breastfeeding for the baby
Breastmilk has many advantages over cow’s milk or other formula foods. Explaining the following benefits to the mothers will help you to convince them about the practice of breastfeeding.
4.3.1 Nutritional
Breastmilk has all the necessary nutrients needed for the newborn or infant (see Figure 4.4). This is true even if the mother is not taking adequate amounts of the nutrients for her own needs. Moreover it is free of contamination and does not need any preparation. It is also self-regulatory; breastmilk secretion occurs based on the need of the infant, so if there is more feeding there will be more secretion. If the mother tries to introduce supplementary food such as formula milk early in the life of the baby (as early as under four months), there will be replacement of the clean, nutritious breastmilk by formula or cow’s milk which is more likely to be contaminated, resulting in increased risk of infection. Therefore, breastmilk should be considered to be a whole food for the infant because it contains balanced proportions and a sufficient quantity of all the nutrients needed for the first six months. Box 4.1 summarises the key benefits of breastfeeding for the baby.

Box 4.1 Nutritional benefits of breastfeeding.
- Breastmilk is always clean
- Breastmilk is always ready and at the right temperature
- Breastmilk is easy to digest
- Nutrients are easily absorbed from breastmilk
- Breastmilk protects against allergies
- Breastmilk antibodies protect the baby’s gut by preventing harmful substances from passing into the blood
- Breastmilk contains enough water for the baby’s needs
- Breastmilk has a low protein content which makes it suitable for feeding small infants before their kidneys are fully developed. The amount of protein is adequate to promote the normal growth of the baby
- Breastmilk is low in saturated fatty acids; saturated fatty acids from cow’s milk may form a hard curd when they react with hydrochloric acid in the baby’s stomach and may result in the impacting of the curd in the intestine. Cow’s milk is rich in these acids and also contains large amounts of protein. Breastmilk is much safer.
4.3.2 Builds up immunity
Breastmilk has many active immune agents that protect the child from developing diseases and therefore promotes the normal growth of the child.
4.3.3 Growth factors
Breastmilk is important for the normal growth of the baby.
4.3.4 Development factors
The fat in breastmilk has been found to be very important for the development of the brain. Breastfed children show better intelligence as compared to bottle or formula-fed children.
- Breastfeeding helps jaw and tooth development; suckling develops facial muscles
- Frequent skin-to-skin contact during breastfeeding leads to better psychomotor, affective and social development of the infant and promotes bonding between mother and child.
4.3.5 The infant benefits from colostrum
Colostrum is the first breastmilk that is produced after delivery and protects the baby from diseases. The colostrum acts as a laxative cleaning the infant’s stomach. It is also the equivalent of the first immunisation for the baby as it has many immunologic factors and a high concentration of vitamin A.
4.4 Benefits of breastfeeding for the mother
As well as breastfeeding bringing benefits to the baby, you can explain to the mother that there are important benefits to her. Box 4.2 sets out some of these.
Box 4.2 Benefits of breastfeeding for mothers
- Breastfeeding is more than 98% effective as a contraceptive method during the first 6 months provided breastfeeding is exclusive and amenorrhoea persists (menstruation has not started)
- Putting the baby to the breast immediately after birth facilitates expulsion of the placenta as the baby’s suckling stimulates uterine contractions
- Breastfeeding reduces risks of bleeding after delivery
- Breastfeeding immediately after birth stimulates breastmilk production
- Immediate and frequent suckling prevents engorgement of the breasts
- Breastfeeding reduces the mother’s workload (no time is involved in boiling water, gathering fuel or preparing formula milk)
- Breastmilk is available at any time and anywhere, is always clean, nutritious and at the right temperature
- Breastfeeding is economical
- Breastfeeding stimulates bonding between mother and baby
- Breastfeeding reduces risks of pre-menopausal breast and ovarian cancer.
4.5 Benefits of breastfeeding for the family
As well as the benefits that breastfeeding has for the baby in promoting health and optimal growth, it also has some essential economical and social benefits to the family. These are set out in Box 4.3.
Box 4.3 Benefits of breastfeeding for families with infants and young children
- There are no expenses in buying formula, firewood or other fuel to boil water, milk, or utensils. The money saved can be used to meet the family’s other needs
- There should be no medical expenses due to the sickness that formula milk might cause. The mothers and their children are healthier
- As illness episodes are reduced in number, the family encounters fewer emotional difficulties associated with the baby’s illness
- Births are spaced thanks to the contraceptive effect of breastfeeding
- Time is saved as breastmilk does not need preparation
- Breastfeeding the baby reduces the mother’s work load because the milk is always available and ready.
4.6 Benefits of breastfeeding for the community
The benefits of breastfeeding go beyond just having a positive impact for the mother and family. It also has important benefits for the community and therefore the nation. Box 4.4 sets out examples of some of these benefits.
Box 4.4 Benefits of breastfeeding for the community
- Breastmilk does not require importing formula and utensils, which saves hard currency (money)
- Healthy babies make a healthy nation
- Breastfeeding leads to a decrease in the number of childhood illnesses, which leads to decreased national expenditure on treatment. This means that savings are made in the health sector
- Breastfeeding improves child survival (reduces child morbidity and mortality)
- An indirect benefit of breastfeeding if it is practised widely is that the environment is protected. This is because trees are not used for firewood to boil water, milk and utensils. Breastmilk is a natural renewable resource.
What are the benefits of colostrum to the baby?
Colostrum is the first breastmilk produced after delivery. It protects the baby from diseases and it also acts as a cleaning substance (laxative) for the baby’s stomach. It is the equivalent of first immunization of the baby, because of its immunologic factors and high concentration of vitamin A.
What is the benefit of breastfeeding to the mother in terms of child spacing?
Breastfeeding is more than 98% effective as a contraceptive method during the first six months provided that breastfeeding is exclusive and amenorrhoea persists.
4.7 Breastfeeding difficulties
In your work helping mothers to breastfeed optimally, you may come across mothers who have one or more breastfeeding difficulties. It is very important that you know the common difficulties, how these can be prevented, and ways that you can help mothers to manage and overcome any problems. Table 4.1 summarises the common breastfeeding difficulties that mothers encounter, some prevention methods and possible solutions if problems develop.
| Difficulty or condition | Prevention | Solution |
|---|---|---|
Engorgement | Correct positioning and attachment Breastfeed immediately after birth Breastfeed on demand (as often and as long as baby wants) day and night: 8–12 times per 24 hours Allow baby to finish the first breast before switching to the second breast | Apply a cold compress (a cloth dipped in cold water) to breasts to reduce swelling; apply warm compresses to get milk flowing Breastfeed more frequently or for longer Improve infant positioning and attachment Massage breasts Express some milk Apply a warm bottle |
Sore or cracked nipples | Correct positioning of baby Do not use bottles, dummies or pacifiers Do not use soap on nipples | Make sure the baby is positioned well at the breast Make sure the baby latches on to the breast correctly Apply drops of breastmilk to nipples and allow to air dry Remove the baby from the breast by breaking suction first Begin to breastfeed on the side that hurts less Do not stop breastfeeding Do not wait until the breast is full to breastfeed; if full, express some milk first |
Plugged breast ducts and mastitis (red, painful and swollen breast) | Get support from the family to perform non-infant care activities Ensure correct attachment Breastfeed on demand Avoid holding the breast in scissors hold (with two fingers in the form of scissors) Avoid sleeping on stomach (mother) Avoid tight clothing Use a variety of positions to rotate pressure points on breasts | Apply heat before the start of breastfeeding Massage the breasts before breastfeeding Increase maternal fluid intake Rest (mother) Breastfeed more frequently Seek medical treatment; if mastitis, antibiotics may be necessary If mother is HIV-positive: express milk and heat, treat or discard Position baby properly |
Insufficient breastmilk (mother ‘thinking’ she does not have enough milk) | Breastfeed more frequently Exclusively breastfeed day and night Breastfeed on demand at least every three hours Correct positioning of baby Encourage support from the family to perform non-infant care chores Avoid bottles and pacifiers | Withdraw any supplement, water, formulas, tea or liquids Feed the baby on demand, day and night Increase frequency of feeds Wake the baby up if it sleeps throughout the night or longer than three hours during the day Make sure the baby latches on to the breast correctly Reassure the mother that she is able to produce sufficient milk Baby takes fore and hind milk |
Insufficient breastmilk Insufficient weight gain Fewer than six wet diapers per day Dissatisfied (frustrated and crying) baby | Same as above | Same as above Refer the mother and baby to nearest health centre |
Pause reading for a while and think of the difficulties of breastfeeding commonly encountered in your community and think about how you would try to prevent and solve these problems if they occur.
What will you advise a mother who thinks she does not have enough milk?
You should reassure the mother that breastmilk can be sufficiently produced as long as the baby sucks very well. To ensure sufficient milk production you can advise the mother to do the following:
- Withdraw any supplement, water, formulas, tea or liquids she has been giving the baby
- Feed the baby on demand, day and night
- Increase the frequency of feeds
- Wake the baby up if the baby sleeps a long time between feeds.
It is possible that you may encounter times where breastfeeding may be difficult because of situations that affect either the capacity of the baby to suck, the availability of the mother or the capacity of the mother to breastfeed. Table 4.2 summarises the solutions to a range of different situations where a mother is having problems breastfeeding.
| Special Situation | Solutions |
|---|---|
Sick baby | Baby under six months: if the baby has diarrhoea or fever the mother should breastfeed exclusively and frequently to avoid dehydration or malnutrition Breastmilk contains water, sugar and salts in adequate quantities, which will help the baby recover quickly from diarrhoea If the baby has severe diarrhoea and shows any signs of dehydration, the mother should continue to breastfeed and provide ORS either with a spoon or cup Baby older than six months: if the baby has diarrhoea or fever, the mother should breastfeed frequently to avoid dehydration or malnutrition. She should also offer the baby bland food (even if the baby is not hungry) and increase the frequency of feeding If the baby has severe diarrhoea and shows any signs of dehydration, the mother should continue to breastfeed and add ORS |
Sick mother | When the mother is suffering from headaches, backaches, colds, diarrhoea or any other common illness, she should continue to breastfeed her baby The mother needs to rest and drink a large amount of fluids to help her recover If the mother does not get better, she should consult a doctor and say that she is breastfeeding |
Premature baby (baby born before nine months) | The mother needs support for correct breastfeeding Breastfeeding is advantageous for pre-term infants; supportive holds may be required Direct breastfeeding may not be possible for several weeks, but expressed breastmilk may be stored for use by the infant If the baby sleeps for long periods of time, he/she should be unwrapped to encourage waking and held vertically to awaken The mother should watch the baby’s sleep and wake cycle and feed during quiet-alert states Crying is the last sign of hunger. Cues of hunger include rooting, licking movements, flexing arms, clenching fists, tensing body and kicking legs |
Malnourished mothers | Mothers need to eat extra food (‘feed the mothers, nurse the baby’) Mothers need to take micronutrients |
Mother who is separated daily from her infant | The mother should express or pump milk and store it for use while separated from the baby; the baby should be fed this milk at times when he/she would normally feed The mother should frequently feed her baby when she is at home The mother who is able to keep her infant with her at the work site should feed her infant frequently |
Twins | The mother can exclusively breastfeed both babies The more each baby nurses, the more milk is produced |
Inverted nipples | Detect during pregnancy Try to pull nipple out and rotate (like turning the knob on a radio) Make a hole in the nipple area of a bra. When a pregnant woman wears this bra, the nipple protrudes through the opening If acceptable, ask someone to suckle the nipple |
Baby who refuses the breast | Position the baby properly Treat engorgement (if present) Avoid giving the baby teats, bottles, pacifiers Wait for the baby to be wide awake and hungry (but not crying) before offering the breast Gently tease the baby’s bottom lip with the nipple until he/she opens his/her mouth wide Do not limit duration of feeds Do not insist on more than a few minutes if baby refuses to suckle Avoid pressure to potential sensitive spots (pain due to forceps, vacuum extractor, clavicle fracture) Express breastmilk, and give to the baby by cup |
Mother who will be away from her infant for an extended period expresses her breastmilk; caregiver feeds expressed breastmilk from a cup. | The mother expresses breastmilk by following these steps:
The mother stores breastmilk in a clean, covered container. Milk can be stored 8-10 hours at room temperature in a cool place and 72 hours in the refrigerator The mother or caregiver gives the infant expressed breastmilk from a cup. Bottles are unsafe to use because they are difficult to wash and can be easily contaminated |
HIV-positive mother who chooses to breastfeed | The mother should practice exclusive breastfeeding for six months. At six months the mother should introduce appropriate complementary foods A mother who experiences breast difficulties such as mastitis, cracked nipples or breast abscess should breastfeed with the unaffected breast and express and discard milk from the affected breast The mother should seek immediate care for a baby with thrush or oral lesions A mother who presents with AIDS-related conditions (prolonged fever, severe cough or diarrhoea, or pneumonia) should visit a health centre immediately A lactating mother should use condoms to protect herself from exposure to infected semen |
HIV-positive mother who chooses to replacement feed | The mother should practice safe and appropriate use of infant formula or animal’s milk (with additional sugar) exclusively for the first six months The mother should use a cup, not a bottle The mother should NOT mix-feed – give only breastmilk substitutes, do not breastfeed |
What solutions would you advise the mother of a sick baby under six months with diarrhoea?
You would advise the mother to breastfeed exclusively and frequently to avoid dehydration or malnutrition. You would explain to her that breastmilk contains water, sugar and salts in adequate quantities, which will help her baby recover quickly from diarrhoea. If the baby has severe diarrhoea and shows any signs of dehydration, tell the mother she should continue to breastfeed and provide Oral Rehyderation Solution (ORS) either with a spoon or cup.
4.8 Key messages for optimal complementary feeding practices
Both the quantity and quality of complementary foods are important to ensure good health and development for the baby and young child. Infants older than six months should eat a variety of nutrient-rich foods, including animal products (e.g. eggs, beef, chicken, lamb, milk, cheese and butter), fruits, and vegetables. It is usually not possible for an infant to consume sufficient quantities of plant foods to meet their needs for iron, zinc and calcium. Therefore, the addition of animal source foods enables the different nutrients to be absorbed more easily and is essential in the preparation of complementary foods.
When you are advising mothers and caregivers about optimal complementary feeding, there are a number of key messages you can give. These are set out below.
At six months, the mother or caregiver must introduce soft, appropriate foods and continue breastfeeding on demand.
- When the infant is six months old the mother must give the infant complementary foods in addition to breastmilk to help the infant grow strong and healthy. At this age, breastmilk alone cannot meet all the nutritional needs for growth and development
- The mother should continue to give breastmilk as the main food throughout the infant’s first year. Breastmilk will continue to protect the child against illness
- The mother or caregiver should begin complementary feeding by adding available, feasible, local foods (vegetables, fruits, eggs, milk) to staple foods (cereals and legumes) and increase the amount of food as the child grows
- The mother should continue breastfeeding until child is at least two years old.
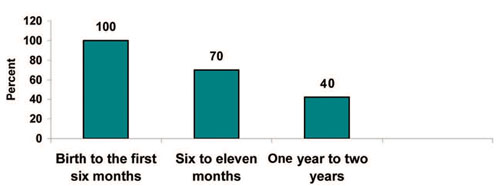
Breastmilk constitutes the largest portion of young child’s food during the first two years. Figure 4.5 shows what percentage of breastmilk should be in a child’s diet from birth to two years.
Here are some additional important messages about feeding.
Increase frequency of feedings
As the child gets older, the mother needs to provide more food and increase the frequency of meals.
- The mother or caregiver should increase the frequency of feedings and the amount of food as the child gets older
- The mother or caregiver should use a separate bowl for the child and continue frequent breastfeeding
- The mother or caregiver should give young children small feeds frequently throughout the day (both day and night) because they have very small stomachs
- As the child grows, the mother or caregiver should give the child more food. One way to know children are getting enough food is to put their portions in separate bowls and to help them eat. This is known as responsive feeding. Table 4.3 summarises the frequency of meals, and their number according to the age of the child.
| Age (months) | Meal frequency per day for breastfed baby | Meal frequency per day for non-breastfed baby |
|---|---|---|
| 6-9 | 2-3 times + 1-2 snacks | 4-5 times + 1-2 snacks |
| 10-23 | 3-4 times + 1-2 snacks | 4-5 times + 1-2 snacks |
Increase food thickness and variety
Increase food thickness (density) and variety as the child gets older, to meet changing nutritional requirements, and the child’s physical abilities.
At six months, the mother or caregiver can give the infant puréed (softened), mashed and semi-solid foods. She should also add protein-rich foods (animal/plant); beans, soya, chick peas, groundnuts, eggs, liver, meat, chicken and milk. Adding germinated (malt) flour to the gruel liquefies cereal gruels and helps to increase the energy value and other nutrient density. At eight months the mother or caregiver can give foods that infant can eat alone, such as cut-up fruit and vegetables (for example, mangoes, papaya, leafy greens, oranges, bananas, pumpkin, carrots and tomatoes). During complementary feeding, the aim is for the mother or caregiver to gradually accustom the child to family foods. By 12 months the child should be eating family foods.
Interact with the child during feeding
The mother or caregiver should interact with the child during feeding. This is known as active or responsive feeding. This helps the child take in the food they need and stimulates the child’s verbal and intellectual development. The mother or caregiver should also feed the infant directly and help older children eat and experiment with food combinations, tastes and textures. Most mothers will be able to find ways to encourage children who refuse certain foods. In order to help the baby finish its food, the mother or caregiver should minimise distractions during meals, especially if the child loses interest easily. The mother or caregiver has to remember that feeding times are periods of learning and love; talking to a child during feeding, with eye-to-eye contact and patience, encouraging but not forcing the infant to eat, is important. The mother can also sing songs or tell stories to make feeding enjoyable.
Practice good hygiene and safe food preparation
In resource-poor settings, the mother or caregiver can feed liquids to the child from a small cup or bowl, as bottles are difficult to keep clean, and contaminated bottles can cause diarrhoea. Before feeding the child, the mother or caregiver should wash their hands and the child’s hands with soap and water and use clean utensils and bowls or dishes to avoid introducing dirt and germs that might cause diarrhoea and other infections. The mother or caregiver can use their fingers (after washing) to feed the child. Food can be contaminated as a result of poor basic hygiene, poor sanitation, and poor methods of food preparation and storage, so food should be served immediately after preparation.
Increase the amount of food provided each day
As children grow older, they need to eat more food each day. Table 4.4 shows the increase in calories needed every day by a child according to their age.
| Age (months) | Amount of kilocalories for the breastfed baby | Amount of kilocalories for the non-breastfed baby |
|---|---|---|
| 6-8 | 200 Kcal | 600 Kcal |
| 9-11 | 300 Kcal | 700 Kcal |
| 12-23 | 550 Kcal | 900 Kcal |
Increases complementary food if the child becomes sick
The mother should continue to breastfeed when the child is ill and should encourage the child who is older than six months to eat during and after illness (sick child feeding). The mother should offer the child who is older than six months soft, mashed favourite foods. Breastfeeding is extremely important during illness. Children who are ill will often continue to breastfeed even if they refuse other foods.
The mother diversifies the complementary food
The mother should mix foods from plant sources such as fruits, vegetables, cereals and legumes with foods of animal origin in order to diversify the complementary food. During illness and for two weeks after illness, the mother or caregiver should increase the quantity of food and feed the child more often so that the child recovers quickly. Children are often very hungry during recovery from illness and need more food to support catch-up growth and to replace nutrient stores.
Kedija’s daughter is six months old and she wants to start giving her complementary food. What do you advise Kedija about feeding her child at this age?
You would talk to Kedija about the different types of food she can give her daughter to promote optimum growth and the baby’s health. At six months Kedija can give her daughter puréed, mashed and semi-solid foods. She should also add protein-rich foods (animal/plant): beans, soya, chick peas, groundnuts, eggs, liver, meat, chicken, milk. Adding germinated (malt) flour to the gruel liquefies cereal gruels, and helps to increase the energy and other nutrient density. You should also advise her to continue breastfeeding until her daughter is at least two years old.
The first 24 months of life provide a critical opportunity to ensure a child has a healthy start through optimal feeding. You have learned that malnutrition can be prevented through exclusive breastfeeding for the first six months of a baby’s life, followed by the introduction of complementary food.
Complementary food should be started at exactly six months, not before or after six months, as either would lead to poor nutritional status of the young child. The consequences of poor nutritional status include morbidity, poor growth and development and mortality.
Summary of Study Session 4
In Study Session 4 you have learned that:
- Children should be fed optimally during the first 24 months of their lives as this is a critical window of opportunity to break the cycle of malnutrition which otherwise can be passed from generation to generation.
- Breastmilk is the best and most nutritious food for the baby during the first two years. It has several advantages for the baby compared to cow’s milk or other replacement food.
- Feeding for the first 24 months should be based on exclusive breastfeeding during the first six months, with complementary foods introduced at six months in addition to ongoing breastfeeding.
- Complementary food should be increased in frequency, amount and density (thickness and nutrient content) as the child grows.
- Mothers should increase the frequency of breastfeeding and complementary feeding (if the child has already started it) during illness.
- Mother should give a diversified diet to their baby and include animal sources of foods to increase the density of nutrients in the complementary food.
- HIV-positive mothers should either exclusively breastfeed or exclusively replacement feed. Mixed feeding is dangerous as it exposes the baby to mother-to-child transmission of HIV.
Self-Assessment Questions (SAQs) for Study Session 4
Now that you have completed the study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers on your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the notes on the Self-Assessment Questions at the end of the Module.
SAQ 4.1 (tests Learning Outcomes 4.1 and 4.2)
Why is it so important for you to be able to advise mothers about how to feed babies and very young children?
Answer
If babies and young children can be fed well there is a real opportunity to break the cycle of malnutrition. However, at the moment, many babies are not exclusively breastfed and many infants are given complementary food too early or too late. These problems are due to lack of knowledge on the mother’s part. Therefore, it is important they receive more information and advice, and as a Health Extension Practitioner you are in a good position to be able to do this.
SAQ 4.2 (tests Learning Outcomes 4.3 and 4.5)
Whilst giving education to mothers about breastfeeding, they may ask you why they need to breastfeed their babies when they can give them cow’s milk or formula and go to work. What would you tell them to try to convince them?
Answer
When giving education to mothers about breastfeeding, you could tell them that breastmilk is an irreplaceable gift of the mother to the baby because it protects the baby from different infectious diseases. In addition, the fat in breastmilk has been found to be very important for the development of the brain. Breastfed children show better intelligence compared to bottle or formula fed ones.
Breastfeeding also has other advantages. It has contraceptive and uterine-contracting effects that help the mother to space pregnancies and prevent postpartum haemorrhage, respectively. And it is also readily and freely available, and saves household expenditures for feeding the baby.
So the working mother should express her breastmilk and get the baby fed by the caregivers when she is at the work.
SAQ 4.3 (tests Learning Outcome 4.3)
A mother who is expecting her first baby soon is very keen to breastfeed and asks for your advice. What is the key advice you should give her now so she is prepared for the first few weeks?
Answer
When advising a mother who is expecting her first baby you need to tell her to start breastfeeding within an hour of birth; to breastfeed frequently; to give the baby only breastmilk for the first six months; and to eat more than usual herself. You might also want to tell her now about how to position the baby. And you should also tell her that if she has any difficulties she should ask you how to overcome these.
SAQ 4.4 (Tests Learning Outcome 4.4)
What advice should you give to an HIV-positive mother who is unable to buy replacement foods?
Answer
If you are advising an HIV-positive mother who cannot afford to buy replacement foods, you should tell her that:
- She should practice exclusive breastfeeding for six months and then introduce appropriate complementary foods
- If she experiences breast difficulties such as mastitis, cracked nipples or breast abscess, she should breastfeed with the unaffected breast and express and discard milk from the affected breast
- She should seek immediate care for a baby with thrush or oral lesions
- If she experiences AIDS-related conditions (prolonged fever, severe cough or diarrhoea, or pneumonia) she should visit a health centre immediately
- She should use condoms to protect herself from exposure to infected semen.
SAQ 4.5 (tests Learning Outcome 4.6)
A mother tells you that breastfeeding is hurting her. What kinds of pain might she be referring to? Would you advise her to stop breastfeeding until the pain goes? Give reasons for your answer.
Answer
If a mother tells you that breastfeeding hurts, the reasons might be engorgement, sore or cracked nipples, or plugged breast ducts and mastitis. You should advise her to continue breastfeeding, giving her information about the appropriate solutions to relieve the problem.
SAQ 4.6 (Tests Learning Outcome 4.7)
Suppose you want to educate a mother about optimal complementary feeding. What are the key messages you will give her?
Answer
Key messages about optimal complementary feeding include the following:
- At six months, the mother or caregiver should introduce soft, appropriate foods and continue breastfeeding on demand
- She should give a range of different foods
- She should increase complementary food if the child becomes sick
- The mother has to increase the amount of food the baby eats as the baby grows older, increasing food thickness (density) and variety
- She should practice good hygiene and safe food preparation
- She should interact with the child during feeding (active/responsive feeding).