Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Tuesday, 24 February 2026, 10:53 PM
Nutrition: 7. Preventing Micronutrient Problems in Ethiopia
Study Session 7 Preventing Micronutrient Problems in Ethiopia
Introduction
As well as having a diet with a balance of fats, carbohydrates and proteins, the health and vitality of all human beings depends on a diet that includes adequate amounts of vitamins and minerals. These are the ‘micronutrients’ that are necessary to help the body in all its functions, including reproduction, and to make sure that it can fight infection. People need micronutrients so they can use their brains and have the energy to keep their body working as well as possible. Your job as a Health Extension Practitioner will involve helping people to understand the importance of these components in a diverse diet. Among these micronutrients, three have obtained worldwide attention due to their high public health significance. If people don’t get sufficient vitamin A, iodine and iron, this can lead to grave health as well as social and economic consequences.
In this session you will learn more about these micronutrients, as well as the extent and consequences of their deficiency. You will also learn how to prevent and treat the major micronutrient deficiencies in your community.
Learning Outcomes for Study Session 7
When you have studied this session, you should be able to:
7.1 Define and use correctly all of the key words printed in bold. (SAQ 7.1)
7.2 Recognise the magnitude of micronutrient deficiencies in Ethiopia. (SAQ 7.1)
7.3 Identify those at risk of developing vitamin A deficiency. (SAQ 7.2)
7.4 Identify children with anaemia and those at risk of developing anaemia. (SAQ 7.3)
7.5 Recognise people with iodine deficiency disorder (IDD) and those at risk of developing IDD. (SAQ 7.3)
7.6 Identify the causes and consequences of iron deficiency. (SAQ 7.3)
7.7 Understand some of the methods that you will be able to use in your own community to prevent and treat these common micronutrient deficiencies. (SAQ 7.4)
7.1 The importance of micronutrients
Earlier, in Study Session 2, you looked at micronutrients and their sources, and you learned that people’s health and vitality depends on a diet that includes adequate amounts of vitamins and minerals to keep the body functioning efficiently. Vitamins are necessary in small amounts in our diet to facilitate growth, maintenance of health and reproduction. Minerals do not originate in animal or plant life but come from the earth. Although minerals make up only a small portion of body tissues, they are essential for normal growth and functioning.
Because only very minute quantities of vitamins and minerals are needed for health, they are called micronutrients. These elements are essential; they cannot be manufactured by the human body and must be obtained through dietary means. Among these micronutrients, three have obtained worldwide attention and are the focus of this study session due to their high public health significance. Vitamin A, iodine and iron deficiencies lead to grave health, social and economic consequences; but the good news is that there are cost-effective strategies to overcome these deficiencies.
What role do you think that village level health workers could have in helping their communities avoid micronutrient deficiencies?
Village health workers such as yourself can encourage families to grow the right sort of foods, and to attend and bring their children to supplementation and treatment services. You can also work with the women in your village to help identify potential problems and families who need support.
The overall goals and objectives of the prevention and treatment of micronutrient deficiencies in Ethiopian are shown in Box 7.1.
Box 7.1 Overall goals and objectives of the prevention and treatment of micronutrient deficiencies in Ethiopia
Goal: to achieve virtual elimination of micronutrient deficiencies in Ethiopia by 2015.
Objectives:
- To increase coverage of the programmes that improve the micronutrient status of the population
- To develop standards for national programmes
- To provide reference materials and aids to health care professionals.
7.2 Vitamin A, iodine and iron deficiencies in Ethiopia
Vitamin A deficiency (VAD) is a severe public health problem in Ethiopia affecting around 61% of children 6-59 months of age in the 11 regions of the country (DHS, 2005). The situation is probably worse in emergency affected areas. Clinical vitamin A deficiency, untreated can lead to childhood blindness and it is likely that vitamin A deficiency is one of the major contributing factors to the high under-five mortality rate of Ethiopia (174 per 1000, UNICEF).
Globally, 30% of the world’s population is affected with iodine deficiency disorder (IDD). In Ethiopia, one out of every 1000 people is affected and about 50,000 prenatal deaths occur yearly due to iodine deficiency disorder. As you read in Study Session 1, the rate of goitre (caused by iodine deficiency) in Ethiopia is at emergency levels according to WHO standards. This is in part because of the marked decrease in the amount of iodised salt being consumed in Ethiopian households compared with a decade ago. About 685,000 babies are born to mothers with IDD and as a result stand a risk of suffering from some degree of learning disability.
Anaemia is a widespread health problem affecting more than two billion people worldwide — one third of the world’s population. More than half (54%) of Ethiopian children age 6-9 months and 27 % of Ethiopian women aged 15-49 are anaemic (mainly due to low blood iron status).
The consequences of anaemia are multiple. Iron deficiency can delay muscular and nervous system development and mental performance, especially in preschool age children. In adults, anaemia reduces work capacity, mental performance and reduces tolerance to infections. Iron deficiency anaemia can also cause increased maternal mortality due to bleeding problems. Maternal anaemia can lead to prenatal infant loss, low birth weight, and pre-term births.
How could you find out if there are any people in your community with micronutrient deficiencies?
There are a number of potential sources of information you might have listed, for example you could:
- Ask teachers if there are children who miss school (children with anaemia may be too tired to attend)
- Ask family members if there are mothers and children who find it difficult to see after dusk and if children frequently get sick (possible signs of vitamin A deficiency)
- Ask community leaders/families if there are any children/adolescents who have swelling in front neck area (goitre: a sign of iodine deficiency).
7.3 Rationale for action against vitamin A, iron and iodine deficiencies
Ethiopia has developed a National Nutrition Strategy, and a National Nutrition Programme (NNP) was launched in September 2008. This NNP sets out the need for tackling vitamin A, iron and iodine deficiencies.
7.3.1 Rationale for action against vitamin A deficiency
Action against vitamin A deficiency is important, because improving a child’s vitamin A status:
Improving a child’s vitamin A status is a cost-effective way of improving their health.
- increases their chance of survival
- reduces the severity of the childhood illness
- prevents night blindness/blindness and may reduce birth defects
- is very cost-effective.
7.3.2 Rationale for action against iodine deficiency
- Universal salt iodisation (USI) can lead to an increase of the average intelligence of the entire school age population by as much as 13 points
- Salt iodisation will improve the physical and mental development of millions of people
- The intellectual and cognitive development of whole generations of Ethiopian children will be reduced by around 10% unless adequate iodine is provided.
7.3.3 Rationale for action against iron deficiency anaemia
Control of anaemia will:
- Decrease maternal mortality
- Decrease premature birth, inter-uterine retardation and low birth weight
- Decrease infant mortality (due to low birth weight)
- Increase capacity to learn
- Increase productivity in all individuals.
7.4 Causes of vitamin A, iron and iodine deficiencies
Vitamin A deficiency (VAD) results when body stores are used up either because too little vitamin A is present in the foods, or there is insufficient absorption of vitamin A from foods. For example, if a diet is lacking in oils or fats, vitamin A is not well absorbed and utilised. VAD can also result from rapid utilisation of vitamin A during illnesses (particularly measles, diarrhoea and fevers), pregnancy and lactation, and during phases of rapid growth in young children. If the vitamin A status in the body is very low:
- The immune systems become weak and illness is more common and more severe, increasing under-five death rates
- The eye could be damaged with appearance of lesions, and when severe, blindness can occur
- There is an increased risk of a woman dying during pregnancy or during the first three months after delivery.
Iodine is found naturally in topsoil, but in most areas of the country and especially the highlands, top soil has been lost due to deforestation, erosion and flooding, and thus food crops lack iodine resulting in dietary iodine deficiency.
Anaemia has multiple causes. Its direct causes can be broadly categorised as poor, insufficient or abnormal red blood cell production, excessive red blood cell destruction, and excessive red blood cell loss. Contributing causes include poor nutrition related to dietary intake and dietary quality (iron deficiency in particular), infectious and parasitic diseases; inadequate sanitation and health behaviours; lack of access to health services; and poverty. The two major direct causes of anaemia, with excessive red cell destruction, are malaria and worm infections.
The NNP and the Health Sector Development Plan IV have a number of programme objectives and targets and these are set out in Tables 7.1 and 7.2.
| Vitamin A deficiency | Iodine deficiency disease | Iron deficiency anaemia |
|---|---|---|
| Infants and children under five and pregnant and lactating women | People of all ages and sexes are vulnerable More at risk are the fetus, young children, pregnant women, and lactating mothers | Low birth weight infants Children aged six-24 months Adolescent girls Pregnant and lactating women Children between six and 11 years of age People living with HIV and AIDS |
| Vitamin A deficiency | Iodine deficiency disease | Iron deficiency anaemia |
|---|---|---|
Goal: to virtually eliminate vitamin A deficiency by the year 2015 Objectives: At least 90% of children 6-59 months given vitamin A every six months (all the country except Addis Ababa) Supplement 70% of postpartum women with high doses of vitamin A within 45 days of delivery | Goal: Virtual elimination of iodine deficiency disorders by the year 2015 by means of universal salt iodisation (USI) Objectives: Decrease current goitre rate by 50%. Increase access to iodised salt among households up to 80% | Goal: Virtual elimination of ion deficiency amaemia Objectives: Reduce the prevalence of ion deficiency anaemia in women of reproductive age and children under five, by one third by 2015 |
7.5 Strategies to control vitamin A, iodine and iron deficiencies
As a Health Extension Practitioner, the strategies and activities outlined in the national strategies will be carried out by you with the help of village Community Health Workers and supervisors.
7.5.1 Strategies for the control of vitamin A deficiency
The main strategies which have been adapted globally to control and eliminate vitamin A deficiency are explained below:
Promote and support exclusive breastfeeding up to six months of age
As you read in earlier study sessions, breastmilk protects infants in their first six months against infectious diseases that can deplete vitamin A stores and interfere with vitamin A absorption. The vitamin A intake of a breastfed child depends on the vitamin A status of the mother, the stage of lactation, and the quantity of breastmilk consumed. From birth to about six months of age, exclusive, frequent breastfeeding can provide the infant with all the vitamin A needed for optimal health, growth and development. Therefore, exclusive breastfeeding until six months of age helps ensure sufficient vitamin A intake. Figure 7.1 below shows a poster that advertised the importance of breastfeeding for young babies.
Vitamin A supplementation (VAS)
Supplementation is a low-cost and highly effective means of improving vitamin A status, and the quickest intervention that can be implemented on a national scale.
- Vitamin A capsules given twice yearly at six months intervals to children 6 to 59 months is protective, and sufficient for a child’s requirement
- Vitamin A capsules given to postpartum mothers within 45 days after delivery increases the amount of the vitamin A in the breastmilk and therefore the infant’s intake of vitamin A.
- Dietary approaches are also important and include:
- Fortification which is the process of adding vitamin A to foods commonly consumed by vulnerable population. It is an effective and sustainable strategy to combat vitamin A deficiency
- As well as breastfeeding, home gardens are also an essential component of vitamin A deficiency reduction programmes.
7.5.2 Estimating vitamin A supplements requirements
If you do not have a census or register with the total number of children in your catchment area, use the following national statistics to plan how many vitamin A supplies you need for your community:
- 2% of the total population as an estimate for the number of children six-11 months
- 14% of the total population as an estimate for the number of children 12-59 months.
An additional 10% is always added for wastage.
You should order enough supplies for follow-up doses every four to six months through routine services.
Doses and schedules for vitamin A supplements
Vitamin A supplementation should be given to those at risk using the amounts given in the table below.
| Age | Dose | Frequency |
|---|---|---|
| Children 6-11 months | 100,000 IU (one capsule of 100,000 IU) | Once |
| Children 12-59 months | 200,000 IU (two capsules of 100,000 IU) | Once every four to six months |
| Postpartum women | 200,000 IU (three capsules of 100,000 IU) | Within 45 day after delivery |
7.5.3 Administering vitamin A supplements safely using a capsule
Giving a child vitamin A using a capsule can be done easily and safely if you follow these steps:
- Check the age of the child
- Ask the caregiver if the child has received vitamin A capsule in the last month. If the answer is yes, you do not need to give the child vitamin A at this time
- If the answer is no, ask the caregiver to hold the child firmly and make sure the child is calm
- Give the appropriate dose of vitamin A to the child:
- 100,000 IU to child 6-11 months
- 200,000 IU to child 12-59 months.
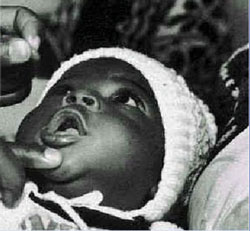
- Cut the nipple of the capsule at the middle (not at the tip or bottom) with scissors and immediately squeeze the drops of liquid into the child’s mouth (see Figure 7.2)
- Check if the child is comfortable after swallowing the drops
- Put all capsules that have been used into a plastic bag
- Wipe your hands to clean off the drops of oil
- Record the dose given on the tally sheet.
![]() Do not put the vitamin A capsule into the child’s mouth or allow the child to swallow the capsule.
Do not put the vitamin A capsule into the child’s mouth or allow the child to swallow the capsule.
Do not give a vitamin A capsule if the child has already received a dose within the last month.
Do not give a vitamin A capsule to any woman of reproductive age during an Enhanced Outreach Strategy Programme. A large dose of vitamin A supplements can damage the fetus if the woman is pregnant.
7.5.4 Choking after a vitamin A dose
If an infant or child starts choking when you administer the vitamin A dose you should do the following:
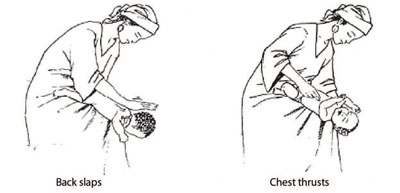
For infants:
- Lay the infant on your arm or thigh in a head down position
- Give five blows to the infant's back with heel of hand
- If obstruction persists, turn the infant over and give five chest thrusts with two fingers, one fingerbreadth below nipple level in midline (see Figure 7.3).
For children:
- Give five blows to the child's back with heel of hand with child sitting, kneeling or lying
- If the obstruction persists, go behind the child and pass your arms around the child’s body; form a fist with one hand immediately below the child’s breast bone (sternum); place the other hand over the fist and pull upwards into the abdomen; repeat this Heimlich manoeuvre five times (see Figure 7.4)
- If the obstruction persists, check the child’s mouth for any obstruction, which can be removed
- If necessary, repeat this sequence with backslaps again.
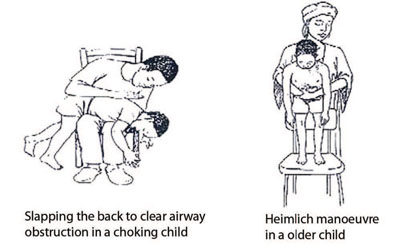
Table 7.4 below is a summary of the different symptoms you might observe as side effects of vitamin A administration, which include overdose and accidental choking. It also describes how you can prevent these from happening and what actions you need to take to overcome these problems if they occur.
| Symptoms | Preventable? | Action required | |
|---|---|---|---|
| Side-effect | Headache, loss of appetite, vomiting or a bulging fontanel (in infants) | NO, it happens with approx. 5% of children | Advise the parent that this is normal, symptoms will pass and no medical treatment is necessary |
| Not harmful | |||
| Overdose | Vomiting and lethargy/listlessness | YES, if protocol is followed | Refer for medical treatment |
| Only occurs if child takes multiple doses together | Report | ||
| Choking | Accidental blocking of trachea | YES, if proper administration of the vitamin A dose is carried out | Resuscitation |
| Report |
7.5.5 Dietary diversification and modification for Vitamin A
As well as the strategies you read about in 7.5.1, there are longer-term and more sustainable interventions for the prevention of vitamin A deficiency. As a Health Extension Practitioner, you are expected to encourage family members to grow and consume vitamin A rich foods at all times. This requires input from several of your colleagues, such as the development agents, teachers, local administration and local NGOs. You can initiate and coordinate the establishment of horticultural demonstration gardens in health post and schools, as well as agricultural extension demonstration plots in farming areas. These horticultural gardens can also serve as examples for dissemination of information on the use of fruits and vegetables, and the distribution of seedlings that could be grown around rural homes. Health Extension Practitioners can therefore play a significant role in promoting the introduction of vitamin A rich foods and improving consumption and storage of such foods. Box 7.2, describes foods that are good sources of vitamin A and in Figure 7.5 you can see photos taken during a visit to a women’s project where food is being produced for their village.
Box 7.2 Examples of food sources rich in vitamin A.
Animal sources of Vitamin A
- The best food sources are animal foods such as egg yolks, organ meats such as liver, whole milk and milk products, small fish with the liver intact, fish, cod liver oil, butter, and ghee.
- The best source of vitamin A for infants is breastmilk. The mother’s secretion of vitamin A into breastmilk is related to her own vitamin A status.
Plant Sources of Vitamin A
- The best plant sources of vitamin A are dark orange or dark yellow fruits and vegetables such as papayas, mangos, pumpkins, carrots, and yellow or orange sweet potatoes, and dark green vegetables such as spinach and kale
- ‘Gommen’ is an example of a traditional plant which is rich in vitamin A and commonly included in the Ethiopian diet.
Food fortification
This involves adding one or more vitamins and minerals to commonly consumed foods, especially those for children, with the purpose of preventing or correcting a demonstrated deficiency. It is difficult to fortify foods in Ethiopia because no staple food has been identified as widely consumed in the entire country. However, efforts are underway to fortify oils that are being produced in some of the larger factories.
7.5.6 Strategies for the control of Iodine deficiency
The main strategies to control and eliminate iodine deficiency are the following:
Universal iodisation of salt for human and animal consumption
Iodine deficiency disorder can be eliminated by the daily consumption of iodised salt which is both a preventive and corrective measure for iodine deficiency and the most effective, low-cost, long-term solution to a major public health problem. The daily requirement of iodine for adults is 150 micrograms.
Your responsibility in control of IDD is to check twice a year if families in your community are consuming iodised salt. You read how to conduct testing of the salt that families consume in Study Session 4.
Supplementation of iodine capsules to populations in areas where iodine deficiency in very common
Iodine capsule dosages are:
One capsule for pregnant women and children under five.
Two capsules for women of reproductive age and children five to 14 years of age.
As a short-term strategy in highly endemic areas, iodised oil capsules should be distributed on a one-time basis to individuals. This will cover the recipients for one to two years until salt iodisation processes are in place.
7.5.7 Strategies for the control of iron deficiency anaemia
The strategy for the reduction of iron deficiency anaemia should be holistic and sustainable. For this to happen there is a need to involve relevant stakeholders from agriculture, education, information and other relevant sectors in planning and implementation of priority programs. The main strategies are the following:
Supplementation of iron and folic acid for pregnant and lactating women
Pregnant women require a much higher amount of iron than is met by most diets and therefore it is important that they routinely receive iron supplements. In places where anaemia is high, supplementation should continue into the postpartum period to enable them to acquire adequate stores of iron. Table 7.5 sets out the correct dosage and duration for iron and folic acid for pregnant and lactating women.
| Iron-folic acid doses | Duration |
|---|---|
Iron: 60 mg/day Folic acid: 400 mcg/day |
|
Supplementation for children and adolescents
Many children from six to 24 months of age need more iron than is available in breastmilk and common complementary foods. Infants with low birth weight have fewer iron stores, and are thus at a higher risk for deficiency after two months of age. In areas where iron fortified complementary foods are not available for regular consumption, children should routinely receive supplements in the first year of life. In areas where anaemia prevalence in young children is 40% or more, delivery of iron supplements should continue through the second year of life, and also be given to adolescent girls. Look at Table 7.6, which sets out the correct doses of iron and folic acid according to the age of the child.
| Group | Iron-folic acid doses | Duration |
|---|---|---|
| Low-birth weight infants (under 2500 g) | Iron: 2 mg/kg body weight/day Folic acid: 50 mcg/day | Two-24 months of age |
| 6-24 month old children | Iron: 2 mg/kg body weight/day Folic acid: 50 mcg/day |
|
| 24-59 month old children | Iron: 20-30 mg iron | At least once a week for three months |
| School-age children (6-11 years) | Iron: 30-60 mg/day | At least once a week for three months |
| Adolescents | Iron: 60 mg/day Folic acid: 400 mcg/day | At least once a week for three months |
Generally there are no side effects to supplementation if protocols are followed.
When might you deliver iron supplementation for children and adolescents?
There are a number of points in a child’s or adolescent’s development when you can encourage the mother, or the older child, to ensure that children and adolescents take iron supplements. For example early on, during postnatal care and the well baby visits, you can talk to the mother about this. You can also talk to the mother about iron supplements during a sick child visit. Other opportunities include school health programmes that you might advise on, or when you are providing family planning services and doing home visits.
Treatment of severe anaemia
Children with severe acute malnutrition should be assumed to be severely anaemic. Oral iron supplementation should be delayed until the child starts eating again and gains weight, usually after 14 days.
If anaemia is diagnosed by clinical examination (extreme pallor of the palms of the hands) or by laboratory tests at health centre, treatment is as set out in the table below.
| Group | Iron-folic acid dose | Duration |
|---|---|---|
| Children under two years old | Iron: 25 mg/day Folic acid: 100-400 mcg/day | Three months |
| Children two-12 years old | Iron: 60 mg/day Folic acid: 400 mcg/day | Three months |
| Adolescents and adults, including pregnant women | Iron: 120 mg/day Folic acid: 400 mcg/day | Three months |
Dietary diversification
Food diversification is an important strategy for prevention of iron deficiency. Populations should be encouraged to produce and consume iron-rich foods throughout the country at all times. Health Extension Practitioners can play a significant role in promoting the introduction of iron-rich foods and improving consumption and storage of such foods. As you know by now, the best source of iron for infants is breastmilk. Look at Table 7.8 overleaf. It describes the best animal and plant sources of iron. As you can read, the way food is processed and cooked has an impact on how well iron is absorbed.
| Animal sources of iron | Plant sources of iron |
|---|---|
| Animal products (meat, organs and blood) provide the best food sources of dietary iron. If these are available, children six to 24 months of age and pregnant women should have priority to include small amounts in their diet. Animal products provide iron that is absorbed easily. Animal products are also the only source of vitamin B12, an important micronutrient for preventing anaemia. | The best plant sources of iron include dark green leafy vegetables and legumes. Legumes are also excellent sources of folic acid. Consumption of foods which are rich in vitamin A will also prevent anaemia. Food processing techniques such as cooking, germinating, fermenting and soaking of grains should be encouraged as they reduce factors that inhibit iron absorption. |
Control of malaria and worms
To control non-iron deficiency anaemia it is also critical to coordinate action with the malaria control and worms control programmes. Pregnant and lactating women and children should sleep under insecticide-treated bed nets.
Children between one and five years of age should receive de-worming drugs. The correct dosage is set out in Table 7.9
| Drugs | Dose for each age group | Comments | ||
|---|---|---|---|---|
| 0-1 year | 1-2 years | 2-5 years | ||
| Albendazole | No treatment | ½ tablet | 1 tablet | These two are particularly attractive because they are single dose and there is no need to weigh the children |
| Mebendazole 500 mg tablet | No treatment | 1 tablet | 1 tablet | |
- De-worming drugs are extremely safe and have no significant side effects
- Minor side effects like nausea and abdominal discomfort are rare usually well tolerated by the children
- Children under one year old are not treated, as they are not exposed to infection
- Accidental repeated treatment with several doses of de-worming drugs is not dangerous.
No special training is needed to administer de-worming drugs. Non-health workers with minimal training can easily and safely give them. Training someone on how to administer the drugs and the benefits of de-worming can be done in a few hours. In addition, it is important to encourage hygiene and environmental sanitation to prevent women, children, or people living with HIV and AIDS from getting parasites such as worms.
7.6 Prevention and control of vitamin A and iodine deficiencies
In addition to the supplementation and treatment services you have just read about, there are other equally important activities that you can do within your community to address micronutrient deficiencies.
To address vitamin A deficiency you can:
- Help to mobilise and support communities to produce fruit and vegetable gardens to improve access to vitamin A rich foods
- Support community child health days
- Ensure an adequate supply of vitamin A capsules for your community
- Monitor vitamin A supplementation coverage in your community.
To address iodine deficiency disorder you can:
- Help to strengthen the national iodine deficiency control and prevention programme by monitoring use of iodised salt in your community twice a year (Study Session 5)
- Implementing advocacy and creating demand for universal consumption of iodised salt.
7.7 Prevention and control of zinc deficiency
Zinc is an essential nutrient for human health. It is a key factor for normal growth and in the fight against child illness and mortality in developing countries and therefore very important for public health. In addition, when zinc is provided as a supplement to children in lower-income countries, it reduces the frequency and severity of diarrhoea, pneumonia and possibly malaria. There is also some evidence that zinc supplementation of women during pregnancy may prevent adverse outcomes of pregnancy and contribute to increased infant weight gain and a reduced risk of infection.
Zinc supplements have been shown to increase the growth and weight gain of stunted or underweight children. Moreover, studies have shown that children who receive zinc supplements have lower death rates.
Approximately one third of the world’s population live in areas at high risk of zinc deficiency. The most vulnerable population groups are infants, young children, and pregnant and lactating women because of their additional requirements for this essential nutrient.
7.7.1 Zinc deficiency and the Millennium Development Goals
Zinc intervention programmes can help to achieve three of the four health-related MDGs:
- MDG 4: Reduce child mortality — zinc deficiency contributes substantially to diarrhoea and pneumonia, which are the most common causes of death among children in developing countries. Therefore, interventions to enhance the zinc intake of children in low-income countries are a useful strategy to reducing child mortality rates
- MDG 5: Reduce maternal mortality — zinc deficiency can result in protracted labour, which increases maternal mortality rates and adversely affects the fetus. Therefore, improving the zinc intake of women before and during pregnancy may help to reduce maternal mortality and benefit infant growth and survival
- MDG 6: Combat HIV/AIDS, malaria, and other diseases — there is evidence that zinc supplementation may reduce the severity of malaria. In addition, zinc supplementation reduces the risk of both diarrhoea and pneumonia, which frequently complicate HIV infections. Therefore, zinc supplementation may reduce fatalities from these diseases.
7.7.2 Addressing zinc deficiency
Exclusive breastfeeding during the first six months of life should be supported because breastmilk is an excellent source of zinc. For young children, complementary feeding practices should be implemented with zinc-rich foods, such as animal source foods, and zinc-fortified complementary foods. The table below shows food sources with different levels of zinc content.
| Zinc content | Types of food |
|---|---|
| Foods that provide the highest concentrations of zinc | Lean red meat, whole-grain cereals, pulses and legumes |
| Food sources with moderate zinc content | Processed cereals with low extraction rates, polished rice, and chicken, pork or meat with high fat content |
| Foods with small amount of zinc | Fish, roots and tubers, green leafy vegetables and fruits are only modest sources of zinc |
| Foods with very low zinc content | Saturated fats and oils, sugar, and alcohol |
Opportunities to improve zinc status should be considered in the context of ongoing general health and nutrition programme such as growth monitoring programmes, diarrhoea treatment facilities, integrated management of childhood illnesses (IMCI) interventions and national fortification programmes.
Summary of Study Session 7
In Study Session 7 you have learned that:
- If the vitamin A status in the body is very low, the immune system becomes weak and illness is more common and more severe, increasing under-five death rates.
- Lack of vitamin A can lead to eye damage or, when severe, can cause blindness.
- There is an increased risk of a woman dying during pregnancy and the first three months after delivery, if her vitamin A status is low.
- Babies born to mothers with iodine deficiency are at risk of suffering from some degree of learning disability.
- Iron deficiency reduces learning capacity especially in preschool age children. In adults, anaemia reduces work capacity and mental performance as well as tolerance to infections. Iron deficiency anaemia can also cause increased maternal mortality due to bleeding problems.
- Zinc is required for normal child growth. In addition, zinc reduces the frequency and severity of diarrhoea, pneumonia, and possibly malaria.
- There are several strategies that can be used to treat and control anaemia and vitamin A, iodine and zinc deficiencies, including promoting diverse diets and providing supplements at critical times such as during early childhood and pregnancy.
Self-Assessment Questions (SAQs) for Study Session 7
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the questions below. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 7.1 (tests Learning Outcomes 7.1 and 7.2)
How does vitamin A deficiency impact on the health of children in Ethiopia?
Answer
Vitamin A deficiency (VAD) results in a child’s immune system being severely weakened. This means illness is more common and likely to be more severe, and leads to an increase under-five death rates. VAD can also lead to eye damage; if lesions on the eye are severe, this can cause blindness.
SAQ 7.2 (tests Learning Outcome 7.3)
Who are the individuals most vulnerable to vitamin A deficiency, iodine deficiency disorder and iron deficiency anaemia in your community?
Answer
The most vulnerable group affected by micronutrient deficiencies, in any community, are frequently children and lactating mothers. This is certainly the case in relation to VAD. However, for iodine deficiency disorder (IDD), people of all ages and sexes are vulnerable, but this deficiency is more critical for the fetus, young children, pregnant women and lactating mothers. In case of iron deficiency anaemia (IDA), vulnerable individuals include low birth weight infants, children aged 6–24 months, adolescent girls, pregnant and lactating women, and people living with HIV and AIDS.
SAQ 7.3 (tests Learning Outcomes 7.4, 7.5 and 7.6)
What are the consequences of iodine deficiency disorder and iron deficiency anaemia for children and women in Ethiopia?
Answer
The consequences of IDD are summarised in the table below
| In pregnant women, fetuses and newborns | In infants, children and adolescents | In adults |
|---|---|---|
| • Decreased fertility | • Hypothyroidism | • Goitre and its complications |
| • Spontaneous abortion | • Impaired coordination | • Hypothyroidism |
| • Stillbirths, congenital abnormalities | • Impaired mental function | • Impaired mental function |
| • Neonatal mortality | • IQ 13 points lower | • Lower energy and productivity |
| • Cretinism | • Retarded mental and physical development | |
| • Psychomotor defects | • Diminished school performance |
Iron deficiency anaemia affects more than half of children under the age of five and around 27% of women in Ethiopia so it is a serious issue. The consequences of IDA are possible increased risk of maternal mortality, premature birth to low birth weight, and infant mortality. It also impacts of children’s capacity to learn and adult productivity.
SAQ 7.4 (tests Learning Outcome 7.7)
Imagine you have identified people in your community who are suffering from vitamin A deficiency, iodine deficiency disorder and iron deficiency anaemia. What can you do to address these problems?
Answer
There are a range of actions you can take as a Health Extension Practitioner to prevent and treat micronutrient deficiencies in your community. For example you can provide Vitamin A capsules, iodine capsules and iron folate for prevention of VAD, IDD and IDA respectively. You can work with individuals and families and advise on food diversification and food fortification, which will help to ensure a more healthy diet.
The other important aspect of your role is to mobilise communities and work with other development workers in your community to produce of fruit and vegetables using backyard gardens, which will help to improve access to vitamin A-rich foods. You can also support community child health days and use these to ensure a supply of vitamin A capsules and the other necessary materials to supplement people’s diets.
